A case report of ds DNA negative with ANA positive SLE induced neuropsychosis diagnosis dilemma
Received: 03-Oct-2022, Manuscript No. AMHSR-22-75947; Editor assigned: 06-Oct-2022, Pre QC No. AMHSR-22-75947; Reviewed: 19-Oct-2022 QC No. AMHSR-22-75947; Revised: 26-Oct-2022, Manuscript No. AMHSR-22-75947; Published: 03-Nov-2022
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
When a young female with no past or family history of mental illness presents with psychotic features, unprovoked panic and limbic symptoms always ask for minor or transient symptoms and signs referable to the other systems which might give valuable clues like of diagnosis like SLE induced psychosis ,For diagnosis of SLE ds DNA is used most of time but many times ANA alone can be used for diagnosis of SLE if patient clinically suggestive SLE signs and symptoms and early diagnosis of SLE psychosis can improve the patient outcome.
Keywords
Antinuclear Antibody (ANA); Anti-double strand DNA antibodies (anti-ds DNA); Mitotic pattern of ANA; Neuropsychiatric SLE (NPSLE);Systemic Lupus Erythematosus ( SLE)
Introduction
Systemic Lupus Erythematosus (SLE) is an autoimmune disorder characterized by the production of a wide range of auto antibodies as a result of polyclonal B cell stimulation, malfunctioning apoptotic pathways, or idiopathic network dysfunction. [1]Anti-double strand DNA antibodies (anti-ds DNA) are thought to be a specific biomarker for SLE, Because of their high frequency (ranges from 70% to 98%), sensitivity and specificity (59% and 97%, respectively), the presence of these auto antibodies could be used most of time for diagnosis of SLE, Despite significant role of these antibodies in SLE diagnosis, 2% to 30% of SLE patients test negative for anti-ds DNA.1But Antinuclear Antibody (ANA) can be used as diagnostic hallmark for SLE, having a frequency of 95%. [2]The most common reported ANA staining involves: speckled, homogeneous, nucleolar and centromere pattern while rare patterns (seen in <1% of ANA-positive patients) have been studied and divided into following categories cell cycle related, nuclear and cytoplasmatic among these patterns, the most studied pattern is mitotic spindle apparatus (MSA).[3]Neuropsychiatric symptoms of SLE is however a diagnosis of exclusion when it presented symptomatically. [4]It is believed to be least understood and missed but probably a not uncommon form of lupus .Here we presenting rare case of ANA positive with ds DNA negative SLE presenting as neuropsychiatric symptoms with vasuculitis changes.
Case Report
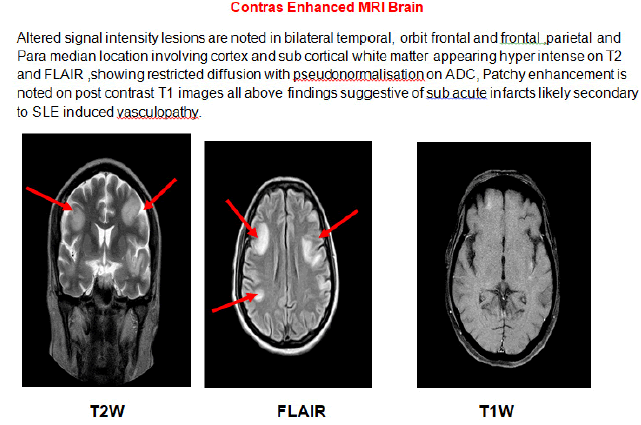
A 40 year old female known case of diabetes with hypertension come to casualty with complains of fever intermittent since 3-4 month, history of altered sensorium in form irrelevant talk and irritability since last 10 days. On leading questions we got the history of joint pains (Polyarthritis large joints >> small joints with arthralgia) since 2 months. History of rash over face and trunk and limbs off and on since 2 years but now prominent since last 2 months (Figure 1). Patient had correlated the rash to be started after drug and labeled as drug reaction from outside hospital. She also have history of oral ulcers since 10 days. History of hair and weight loss was present ,on examination patient was conscious but irritable. She was febrile having tachycardia, BP 130/80, RR20/min there was no neck stiffness, bilateral pupil normal size reacting to light. She was moving all 4 limbs equally bilateral planters flexor. Patient had mild pallor, anictric, no lymphaenopathy, clubbing, cyanosis ,pedal edema. JVP not raised. respiratory, per abdomen and cardiovascular examination was normal. On 2nd day of admission patient was in drowsy state hence intubated for protection of airway. On routine examination patient complete blood count was suggestive of decreased hemoglobin 8.2 mg/dl,TLC-7090/cumm, Platelet counts-1,37,000. Her MRI brain plain with contrast suggestive of SLE induced vasculopathy (Figure 2), Cerebrospinal Fluid(CSF) CBNAAT and culture sensitivity was within normal limit, Urine routine suggestive of albuminuria but her serum creatinine was within normal limit with adequate urine output. Rapid Malarial Test ( RMT), Dengue were negative. ANA by Immunofluorescence done on 16/05/2022 before admission showing mitotic pattern with titer of 1:100 and repeat ANA profile it shows cytoplasmic and speckled pattern with titer of 1:320 all other antibodies of ANA profile where negative [Table 1]. Before the test of ANA report ,based on clinical diagnosis (According to EULAR criteria patient is having 14 points) was started with Inject able steroids (Methylprednisolon), Pulse therapy given for 5 days followed by oral steroids, patient was improved neurologically, and got extubated, her rashes was decreased , patient was discharged with Mycophenolate mofitil a steroid sparing drug, plan to give immunosuppressant later on if required.
| Table 1: It shows the Investigations. | |||
|---|---|---|---|
| Parameter | Normal Values | Patient values (average of three values mentioned) | |
| Hemoglobin | 12-16 mg/dl | 8.2 | |
| TLC | 3500-9000/cmm | 7090 | |
| Platelets | 15000-450000/cmm | 137000 | |
| Urea | 7-20 mg/dl | 18 | |
| Creatinine | 0.5-1.2 mg/dl | 1 | |
| Urine routine | |||
| Urine albumin | +++ | ||
| ANA PROFILE | |||
| Anti Nuclear Antibody(ANA) via IFA | Positive Titer - 1:320 (Cytoplasmic and speckled pattern) | ||
| ds-DNA antibody | Negative | ||
| SSA-RO Ig G | Negative | ||
| SSB-La Ig G | Negative | ||
| Sm Antibody, Ig G | Negative | ||
| RNP Sm Antibody | Negative | ||
| JO-1 Antibody | Negative | ||
| Centromere Antibody | Negative | ||
| SCL-70Ig-G | Negative | ||
| U1 snRNP Ig G | Negative | ||
| CSF | Glucose -71, Protein- 50, TLC-12cells/cumm | ||
Discussion
New onset of Psychosis in young females has to be investigated for biological reasons even if severe personal stress has been described as a triggering factor, Lupus erythematosus presents with diverse clinical features and psychiatric symptoms can precede other obvious features, A high index of suspicion and an exploration previously unnoticed mild signs like malaise, fever, evanescent rashes, and loss of hairs will provide important clues for diagnosis. [4]ANA are immunoglobulin’s that attack against the nuclear and cytoplasmic components of autologus cells there are different ANA patterns that are associated with the different autoimmune disorders and severity of disorders.[5] The most common reported ANA staining involves: speckled, homogeneous, nucleolar and centromere pattern while rare patterns (seen in <1% of ANA-positive patients) have been studied and divided into following categories cell cycle related, nuclear and cytoplasmatic pattern among them the most studied is pattern is mitotic spindle apparatus (MSA)[3].
The assessment of four factors, including clinical symptoms, histology, tissue immunofluorescence, and antibody detection testing, is necessary for the proper diagnosis of a patient with a suspected SLE. One of the American College of Rheumatology's (ACR) diagnostic standards for SLE is the presence of ANA and anti-dsDNA antibodies, In routine practice, clinical diagnostic laboratories use the ELISA test But, there are several parameters that indicate the value of a immunofluorescent technique is better than ELISA test hence we used immunoflrescent test for ANA[5].
Mchochberg et al 1997 given diagnostic criteria for SLE which involves following marker and signs ,Malar rash, Discoid rash, Photosensitivity, Recurrent oral ulcers, Arthritis, Serositis, Renal, Neurological and Hematological involvement, Immunological abnormalities in the form of Anti-dsDNA antibody, Anti-Smith antibody, Anti-phospholipid antibody, and Anti-nuclear antibody (ANA) by immune fluorescence suggest the possibility of SLE if four of these are present at any time in a patient's history.4 The diagnosis of SLE depends on the patient’s clinical and laboratory abnormalities different kinds of auto antibodies are present in the sera of SLE patients, and ANA can be used as diagnostic hallmark for SLE, having a frequency of 95%[2].
The pathogenesis of neuropsychiatric symptoms is thought to be caused by lupus cerebritis, auto antibodies attacking neurons, neurolysis caused by antibodies, vasculopathy, and cytokine-induced damage and Neuropsychiatric symptoms precede overt manifestations of SLE in 28%-40% of patients, and this group of patients face diagnostic difficulty. [4]A subgroup of SLE patients primarily manifest central, peripheral, or autonomic nervous system manifestations these are referred as Neuropsychiatric SLE (NPSLE) ,for the purpose of facilitating diagnosis and maintaining validity across clinical investigations, the ACR published 19 case definitions of NPSLE in 1999, Out of 19 cases definition 12 definitions were given for the syndromes linked to CNS involvement[6] mentioned in [Table 2].
| Table 2: Case definitions of neuropsychiatric SLE. | ||
|---|---|---|
| Sl.No | Neuropsychiatric SLE | |
| 1 | Aseptic meningitis | |
| 2 | Cerebrovascular disease | |
| 3 | Demyelinating syndromes | |
| 4 | Headaches | |
| 5 | Movement disorders(Chorea) | |
| 6 | Myelopathy | |
| 7 | Seizure disorder | |
| 8 | Acute confusion states | |
| 9 | Anxiety disorder | |
| 10 | Cognitive dysfunction | |
| 11 | Mood disorders | |
| 12 | Psychosis | |
In case of radiological imaging for neuropsychiatric SLE (NPSLE) MRI is the choice of radiological imaging, One study was done by J.Luyendijk on 74 patients of NPSLE after fulfilling criteria ACR by patients which showed following radiological lesions of MRI brain (1) Punctiform or focal hyper intensities in White Matter (WM) is observed in 75% cases and Grey Matter(GM) 18% of cases suggestive of vascular inflammation that is vasuculitis or autoimmune mediated mechanism of vascular occlusion or narrowing that is vasculopathy with ischemia.(2) Diffuse cortical GM lesions mimicking with an autoantibody mediated response to neuronal tissues (3) Significant confluent hyperintensites in WM suggestive of chronic hypo perfusion due to vasuculitis; while in case various studies on radiological findings of NPSLE vasuculitis shows most common findings of as a white matter hyperintensites which similar to J Luyendijik study. [7]A CSF examination does not help in direct diagnosis of lupus vasuculitis but may becomes most useful in excluding infections caused by bacterial, viral, and parasitic pathology[8].
For physicians, diagnosis of central nervous vasuculitis is challenging. The only reliable form of diagnosis is a brain biopsy, however it is a very invasive technique with little sensitivity and a significant risk of damaging brain structures. Instead of a brain biopsy, a combination of neuro imaging, clinical manifestations, and appropriate diagnostic investigations usually provides an early diagnosis, even though the new EULAR (European League Against Rheumatism) criteria for SLE should be used as a clinical guide, the severity of the condition and its symptoms should be taken into account when designing SLE vasuculitis treatment Usually, mild-to-moderate symptoms can be treated with oral corticosteroids and immunosuppressant’s such Methotrexate, Azathioprine, and Mycophenolate mofetil. But in case severe and life-threatening manifestations, a more aggressive therapy with intravenous high-dose Corticosteroids, Cyclophosphamide, Rituximab, Intravenous immunoglobulin, and Plasmapheresis is taken into consideration[8]
Conclusion
Neuropsychiatric lupus is one of the common manifestations of lupus erythematosus in young females. It can be precipitated by severe stressful conditions and infections. Mild systemic symptoms and signs are present in most patients which are ignored by both patients and medical clinicians during assessment. Albuminuria , and mild hematological changes should be taken up as serious clues to diagnosis to avoid treatment delay resulting in serious complications. New onset psychoses with soft neurological signs need thorough evaluation to rule out Neuropsychiatric SLE and patient can be improved if diagnosed early with treatment.
References
- Conti F, Ceccarelli F, Perricone C, Massaro L, Marocchi E, Miranda F, et al. Systemic lupus erythematosus with and without anti-DSDNA antibodies: Analysis from a large monocentric cohort. Mediators Inflamm. 2015;2015:328078.
[Crossref], [Google Scholar], [Indexed]
- Kim HA, Chung JW, Park HJ, Joe DY, Yim HE, Park HS, et al. An antinuclear antibody-negative patient with lupus nephritis. Korean J Intern Med. 2009;24:76-9.
[Crossref], [Google Scholar], [Indexed]
- Betancur JF, Londoño A, Estrada VE, Puerta SL, Osorno SM, Loaiza A, et al. Uncommon patterns of antinuclear antibodies recognizing mitotic spindle apparatus antigens and clinical associations. Medicine (Baltimore). 2018;97:e11727.
[Crossref], [Google Scholar], [Indexed]
- Chandra SR, Issac TG, Ayyappan K. New onset psychosis as the first manifestation of neuro-psychiatric lupus. A situation causing diagnostic dilemma. Indian J Psychol Med. 2015;37:333-8.
[Crossref], [Google Scholar], [Indexed]
- https://jag.journalagent.com/ejm/pdfs/EJM_20_1_7_10.pdf
- Lüngen EM, Maier V, Venhoff N, Salzer U, Dersch R, Berger B, et al. Systemic lupus erythematosus with isolated psychiatric symptoms and antinuclear antibody detection in the cerebrospinal fluid. Front Psychiatry. 2019;10:226.
[Crossref], [Google Scholar], [Indexed]
- Luyendijk J, Steens SC, Ouwendijk WJ, Steup‐Beekman GM, Bollen EL, Huizinga TW, et al. Neuropsychiatric systemic lupus erythematosus: lessons learned from magnetic resonance imaging. Arthritis&Rheumatism. 2011;63:722-32.
[Crossref], [Google Scholar], [Indexed]
- Leone P, Prete M, Malerba E, Bray A, Susca N, Ingravallo G, Racanelli V. Lupus vasculitis: An overview. Biomedicines. 2021;9:1626.
[Crossref], [Google Scholar], [Indexed]





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.