A Comprehensive HIV Program by an Indigenous Organization in Nigeria: A 5-Year Progress Report
2 Faculty of Medicine, Imperial College London, St Mary’s Hospital Campus, Norfolk Place, London W2 1PG, UK
Citation: Oleribe OO, et al. A Comprehensive HIV Program by an Indigenous Organization in Nigeria: A 5-Year Progress Report. Ann Med Health Sci Res. 2017; 7: 101-105
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Nigeria has a high HIV burden with over 3,500,000 infected and more than 200,000 deaths annually. Since 2004, international donor agencies and implementing partners managed HIV programs in Nigeria. Excellence and Friends Management Care Centre (EFMC) was the first local organization to be funded to provide comprehensive HIV services in Nigeria. Aim: To document the need, processes and products of five years of indigenous HIV programming in Nigeria. Materials and Methods: PEPFAR funded EFMC from 2011 to provide comprehensive HIV services in Nasarawa State and Abuja, the Federal Capital Territory (FCT). EFMC engaged staff, assessed and activated sites, trained and empowered healthcare workers, provided consumables, enrolled clients and provided preventive, treatment and support services. EFMC also strengthened healthcare systems and refurbished and equipped facilities for integrated HIV services. Results: EFMC decentralized, commonized and integrated HIV services in over 120 service delivery points with an average cost per target of US$ 273.12. We tested 623,148 people for HIV. The positivity rate was 3.3% (annual range 1.9–4.5%). We placed 10,150 on Highly Active Antiretroviral Therapy. In addition, we tested 164,746 pregnant women for HIV with 5,442 (3.3%) positive and provided 4,189 (77.0%) positive pregnant women with ARV prophylaxis. More than 500 healthcare workers in HIV program management. Conclusions: EFMC’s “commonization” model is cost-effective and efficient. Progressively funding local partners will ensure sustainability of HIV programs. Using program results as national figures will save cost from periodic sentinel studies. Government should support local NGOs to control the HIV epidemic in Nigeria.
Keywords
HIV and AIDS; EFMC; Nigeria; Indigenous programming
Introduction
Over 35 million people have died from AIDS-related illnesses since the start of the epidemic, including 1.1 million in 2015, while approximately 36.7 million people worldwide were living with HIV/AIDS at the end of 2015. [1,2] Sub-Saharan Africa is the most affected region - having about 25.6 million people living with HIV in 2015. This accounts for two-thirds (i.e. 66%) of the global burden of new HIV infections. [1,2]
Effective treatment with antiretroviral drugs controls the virus, ensures improved quality of life for people infected with HIV and reduces the risk of transmitting the virus to others. [3,4] Expansion of antiretroviral therapy greatly transformed HIV infection from a killer disease into a manageable chronic condition. [5]
Need for programming in Nigeria
Nigeria has over 3,500,000 people infected with HIV and accounts for over 10% of the global burden of the disease. [6] Local Non-Governmental Organizations (NGOs) such as Excellence and Friends Management Care Center (EFMC) were funded to support international partners such as Institute of Human Virology. Nigeria (IHVN) in a united fight against HIV and AIDS in Nigeria. For over 5 years (2011 – 2016), EFMC has been involved in the planning, implementation and monitoring of quality HIV prevention, care and treatment services in various states in Nigeria. EFMC employed several methods and techniques that have proven to be effective, and ensured quality care. This report is a summary of the results of EFMC HIV projects in the past 5 years.
Aim
The aim of this work is to document the need, processes and products of five years of indigenous HIV programming by Excellence and Friends Management Care Center (EFMC) in selected states of Nigeria.
Materials and Methods
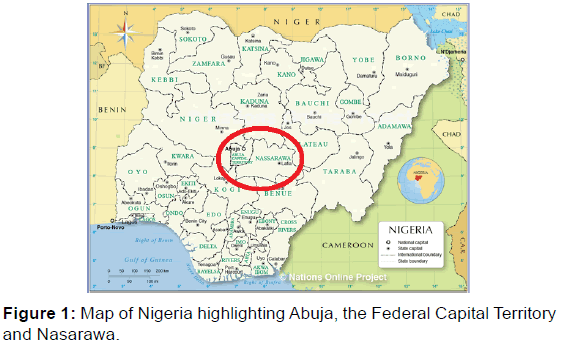
EFMC was funded by PEPFAR directly in 2011 and indirectly through IHVN from 2012 – 2016 to provide comprehensive HIV services in Nasarawa State and Abuja, the Federal Capital Territory (FCT) [Figure 1]. EFMC engaged staff, assessed and activated sites, trained and empowered healthcare workers, provided consumables, enrolled clients and provided preventive, treatment and support services. EFMC also strengthened healthcare systems and refurbished and equipped facilities for integrated HIV services.
Approval to activate sites was obtained from both the state government and management of individual supported facilities. Both existing standards of practice and EFMC innovative operational manuals were used to ensure quality of services, improve effectiveness and efficiency of care, and minimize wastages.
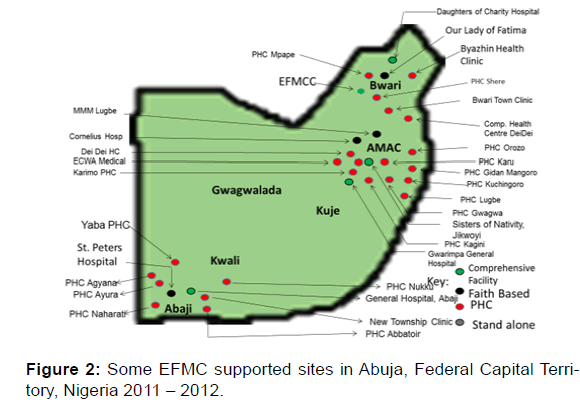
As the primary goal of the projects was to mitigate the HIV epidemic in Nigeria through the provision of quality comprehensive HIV services in Abuja and Nasarawa State, EFMC strategically designed to provide: (1) HIV counselling and testing services at both facility and community levels; (2) Prevention of Mother to child Transmission of HIV services; (3) Clinical care and support services including laboratory services; (4) Strategic information/monitoring and evaluation; (5) Health system strengthening and capacity building; and (6) Support and care for orphans and vulnerable children (OVC). EFMC activated and equipped over 120 sites across the states and ensured functional Project Management Team (PMT) [Figure 2].
EFMC also ensured multi-site HIV Testing and Counselling including innovative door-to-door approach, commonized HIV services in 2012. [7,8] In addition, we established complete referral systems, made prevention of Mother to Child Transmission (PMTCT) a priority, trained and empowered traditional birth attendants (TBA) as feeder sites, provided services in hard to reach communities; and established Antiretroviral Pick-Up Points which were also functional during industrial actions. We used bulk cell-phone SMS text messages were to follow-up clients, reach people with clinical care and treatment services where they lived and worked through the commonization process and piloted “test and treat” strategy in Nigeria by enrolling PLHIVs on treatment irrespective of CD4 count results. [7] We also used Switch Committee to minimize the effects of ARV resistance, restructured support group services to ensure that PLHIVs were properly reoriented and empowered and established sustainable Laboratory and Data Quality Management Systems. Staff and sites capacity development was institutionalized and relevant consumables were regularly provided to the sites.
As part of our preventive packages, counsellors provided prevention messages to clients. We also developed billboards, handbills, jingles and established child health clubs in secondary schools to ensure primary prevention [Figure 3].
Results
Training
Over the last five years, EFMC trained close to 1000 healthcare workers in facilities supported for HIV services. In addition to this, EFMC trained 388 persons in various forms of HIV management, monitoring and evaluation and 381 in leadership, management and effective communication.
Site activation and management
EFMC activated 122 sites in FCT and Nasarawa state. A number of these sites were, in line with the Federal government and US PEPFAR Partnership Framework, handed over to the government as part of the project sustainability plan, or to other implementing partners like Pro Health International, AIDS Prevention Initiative in Nigeria (APIN), CCCRN, etc. EFMC supported sites are provided with regular supply of antiretroviral drugs, laboratory reagents, equipment and their maintenance, and technical support through supportive supervisions and on the job mentoring. Over the 5 years under review, EFMC supported 72 sites on the average (range 42 – 95). Majority of the sites (average 65.2, 90.8%) were within the Federal Capital Territory, Abuja. Site growth was highest in 2013 (95 sites) after which there was a plateau at 73 – 75 in subsequent years.
Staff management
An average of 40 (range: 31 – 57) staff were engaged to execute the comprehensive HIV program in the two states. Staff include public health physicians, nurses, pharmacists, logisticians, community health workers, and administrative staff (accountant, human resource and office managers, drivers, cleaners and other support staff). Although there was high staff turnover due to poor remuneration, staff motivation was high following leadership style of the top management, friendship in the work environment and the impact of the work delivered to clients and families. Staff growth was highest in 2013 (57) after which there was a decline with a marginal increase in 2016.
HIV testing and counseling services
EFMC tested a total of 623,148 within the period under review. Out of this, 20,641 were found to be reactive with HIV antibodies giving a positivity rate of 3.3%. (This data is presented in Table 1).
| General Population HTC | |||
|---|---|---|---|
| Year | Tested | Positive | Percentage |
| 2012 | 107,109 | 4,301 | 4.00% |
| 2013 | 200,746 | 6,243 | 3.10% |
| 2014 | 97,096 | 4,367 | 4.50% |
| 2015 | 84,866 | 3,207 | 3.80% |
| 2016 | 133,331 | 2,523 | 1.90% |
| Total | 623,148 | 20,641 | 3.30% |
| Testing for Pregnant Women alone | |||
| Year | Tested | Positive | Percentage |
| 2012 | 20,742 | 832 | 4.00% |
| 2013 | 34,224 | 955 | 2.80% |
| 2014 | 38,967 | 1,354 | 3.50% |
| 2015 | 37,976 | 1,260 | 3.30% |
| 2016 | 32,837 | 1,041 | 3.20% |
| Total | 164,746 | 5,442 | 3.30% |
| Positive pregnant women who commenced ART | |||
| Year | Positive | Started on ART | Percentage |
| 2012 | 832 | 433 | 52.00% |
| 2013 | 955 | 451 | 47.20% |
| 2014 | 1,354 | 1,105 | 81.60% |
| 2015 | 1,260 | 1,187 | 94.20% |
| 2016 | 1,041 | 1,013 | 97.30% |
| Total | 5,442 | 4,189 | 77.00% |
| Antiretroviral treatment for PLHIVs | |||
| Year | Target | Achievement | Percentage |
| 2012 | 8,894 | 5,374 | 60.40% |
| 2013 | 6,125 | 1,395 | 22.80% |
| 2014 | 4,531 | 5,131 | 113.20% |
| 2015 | 7,631 | 5,539 | 72.60% |
| 2016 | 9,630 | 8,476 | 88.00% |
| Total | 36,811 | 25,915 | 70.40% |
Table 1: HIV testing and counseling services for the general population and pregnant women and initiation of ART for positive pregnant women.
Prevention of mother to child transmission of HIV
164,746 pregnant women (representing 215.3% of ascribed targets) were tested and received their HIV test results. This ranged from 96.7% of ascribed targets in 2014 to 136.1% in 2016. Of all those tested, 5,442 were HIV positive – giving a positivity rate of 3.3% as shown in Table 1. 4,189 HIV positive pregnant women identified in this work received antiretroviral prophylaxis in their index pregnancy. This translates to 77.0% of the total HIV positive pregnant women identified within the period. Review of ART adoption showed the lowest uptake in the first year (52%) and highest in 2016 (97.3%) as shown in Table 1.
Antiretroviral treatment
A total of 25,915 adults and children were placed on highly active antiretroviral treatment (HAART), within the period. Of this, 10,150 (39.2%) were newly commenced on HAART in EFMC supported sites over the five-year period. This represents 32.9% (2011) to 100.7% (2016) of the ascribed target to EFMC by the funders. It also represents just 49.2% of all the identified positive clients (20,641) identified over the same period. Compared to target ascribed, EFMC achieved the least in 2013 (22.8%) and the highest in the very next year (113.2%) as shown in Table 1.
HIV test positivity rate between pregnant women and general population
Although there was annual variation, five year aggregate shows that population and antenatal figures were the same [Table 2].
| Positivity Rate | ||
|---|---|---|
| Year | Pregnant Women | General Population |
| 2012 | 4.0% | 4.0% |
| 2013 | 2.8% | 3.1% |
| 2014 | 3.4% | 4.5% |
| 2015 | 3.3% | 3.8% |
| 2016 | 3.2% | 1.9% |
| Total | 3.3% | 3.3% |
Table 2: The positivity rate of pregnant women compared to general population testing.
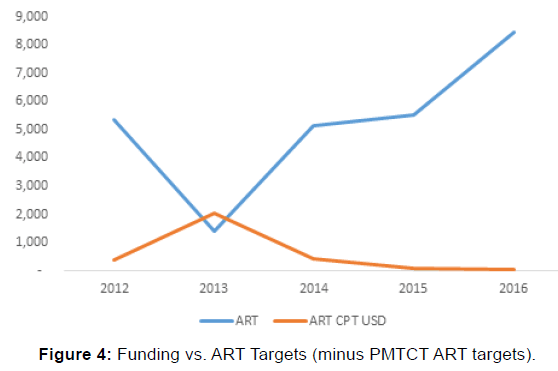
Funding for HIV program over the 5-year period
Funding for the first year was received directly from the United States Centers for Disease Control and Prevention (CDC), while the rest were through Institute of Human Virology, Nigeria (IHVN). Funding progressively decreased over time due challenging economic climate. However, targets to be achieved increased over the same period as shown in Figure 4. This resulted in improved efficiency in the management of resources at all levels.
Discussion
This project allowed EFMC to touch and change lives of patients, healthcare workers and communities. However, in implementing this project, there were several challenges, the majority of which were structural such as poorly trained and demotivated workers in the health facilities. This resulted in poor documentation in care cards and registers. Another challenge that affected service delivery was the drought of personnel at most supported centers which necessitated the use of none healthcare workers in the management of HIV infected patients – especially at the primary healthcare level.
Also, there was the challenge of poor and failing infrastructure across many facilities. In addition, many patients were indigent and thus, unable to pay for relevant laboratory investigations. These factors affected the quality of patient care as baseline or follow up tests were rarely done. These problems became more prominent when the US PEPFAR program discontinued payment for some services. Healthcare workers’ persistence that clients pay for HIV services resulted in loss to follow-up or selftransfers of clients.
Inadequate numbers of qualified healthcare workers, and hospital-based stigma/discrimination led to absence of physical examination including blood pressure and weight measurement, insufficient adherence counseling, poor staging of disease, and weak linkage/referral to other medical specialties. In some facilities, HIV services were still centralized and not fully integrated. Too frequent transfers of trained healthcare worker made retraining frequent and sustained high quality of care very difficult.
These challenges added more work on already overworked EFMC staff that had to continuously review and update care cards and registers. This led to near burnout syndrome as the number of staff was limited. This was not sustainable and may result in future litigation.
The work carried out by EFMC over the past 5 years and its diverse success is a clear indication that since health problems are local in nature, local organizations and solutions can be deployed at a comparative quality and lower cost. This also shows that with more flexible local institutions, critical capacity can be built around healthcare services and program delivery within a short turnaround time. Working with experienced organizations, like Institute of Human Virology Nigeria (IHVN) and Centre for Clinical Care and Research, Nigeria (CCCRN), provided EFMC staff direct mentorship and hands-on experience to navigate difficult problems and was able to succeed where bigger organizations found it difficult to succeed.
Key innovations and achievements of EFMC in the years under review include:
• “Commonization” of HIV/AIDS services at supported facilities: This was a major achievement of EFMC during program implementation where demystification of HIV was strongly advocated and achieved. [7,8] Healthcare workers were constantly reminded that HIV should not be regarded as a special disease requiring special personnel, infrastructure, and clinic days, but should be integrated into the general healthcare system to eliminate stigma and discrimination of HIV-infected persons. Other units of hospitals were integrated as HIV testing points, all in the bid to improve access to HIV services. Some of EFMC’s supported facilities run HIV clinics on all days of the week and not on special days. This, in the long run, enhanced sustainability.
• Inclusiveness: All healthcare workers, rather than a select few, were trained on HIV management to make HIV services available at all levels of healthcare. This encouraged and facilitated task shifting and task sharing. During this process, many facilities in hard-to-reach areas, which had been seemingly abandoned by other implementing partners were taken up, activated and upgraded by EFMC to commence provision of HIV/ AIDS services, making HIV services available in those places.
• Test and Treat: The “Test and Treat” strategy for newly identified HIV positive clients was first piloted by EFMC in 2012 and it is presently being implemented across the priority areas in Nigeria as a means to achieving the UNAIDS 90-90-90 target by 2020. [9] With proper planning, accurate forecasting and reliable supply chain management systems, it is possible for all HIV-infected clients to be started on ART right after diagnosis in Nigeria.
• Feeder Sites Strategy: EFMC built the capacity of unconventional/ alternative systems such as Traditional Birth Attendants (TBA) to offer HIV Testing Services and referral of reactive pregnant women to facilities providing ARVs. Providing services at TBAs enhanced access of pregnant women who preferred to patronize those centers instead of conventional hospitals to HIV/AIDS services as many rural Nigerian pregnant women prefer to deliver their babies at TBA centers. Without EFMC’s provision of services at these centers, many of them would have missed opportunities to be tested for HIV, reactive ones placed on antiretroviral medications, and HIV exposed babies screened and placed on prophylaxis.
• Graduate Internship: EFMC provided opportunities for over 100 fresh graduates to drawn from various Nigerian universities to gain work experience. This prepared them for employment and the challenges of the work-place that lies ahead of them. Those that completed the 8 – 12 months internship were given certificates of completion/proficiency in HIV management or public health depending on their primary unit.
Future Perspectives
Recently, Nigeria adopted the “Test and Treat” strategy to be piloted in some donor supported sites. We see this becoming the norm rather than exception in a few years from now in all service delivery sites.
The new National Agency for the Control of AIDS (NACA) Director General has identified three main areas of focus – community prevalence studies, prevention of mother to child transmission and local production of antiretroviral drugs. We believe that the new NACA emphasis on PMTCT will results in national adaptation of our elimination concept with national change in nomenclature.
NACA is also working at reducing national dependence on donor funds for by galvanizing local funding from government and private sector. If successful, this will help national program achieve the long awaited sustainability it deserves.
Finally, the US government has just awarded PEPFAR III. Although EFMC did not get the primary award, she will work with prime recipients to implement comprehensive HIV program in supported states. Depending on the level of award and involvement, we hope to continue the work we are doing as well as implement new strategies to ensure better quality of care. We also hope that, like Test and Treat, our other innovative strategies will be adopted by the national AIDS program and expanded to all the states.
Conclusion
Currently, most HIV programs in Nigeria are funded by donors. Dependence on external funding is not sustainable. Thus, there is the need for local funding supporting local institutions. Similar local organizations should be encouraged to continue to provide critical services especially in rural areas where the bigger and international organizations would usually not go.
A true private-public partnership should be developed and used to fund HIV programs in Nigeria. Staff and healthcare workers should be properly motivated and oriented to manage HIV cases as any other chronic health condition in their facility. To this end, HIV services should be fully integrated into the healthcare system – destroying the silo system that currently exists in most facilities.
The Nigerian Government should take full ownership of the program and see the donors’ support as an addition to governmental efforts. The Government should either heavily subsidize or completely fund the laboratory investigations which many clients are unable to pay for. This will help improve treatment monitoring and ultimately, treatment outcomes. Government ownership of the HIV program in Nigeria will be an avenue for improvement of the overall health system, especially when there is integration of services into the general health care system. The capacity of different cadres of healthcare workers should be built for better and wider scope of service delivery and there should be better infrastructure. Documentation should be improved upon, and misconceptions by people and organizations should be properly resolved. When documentation is improved upon, reliable data will be available for program evaluation and policy changes.
EFMC and other local NGOs have shown that indigenous programming is possible, effective and efficient. Despite progressively decreasing funding, more clients were tested and placed on active antiretroviral therapy across 75 supported sites, using fewer and moderately paid healthcare workers. The Nigerian government, through the Federal and State Ministries of Health and National Agency for the Control of AIDS (NACA), should sustainably fund local NGOs to end the HIV epidemic in Nigeria.
Finally, local NGOs have attained relevant experience and expertise in implementing HIV programs over the years and are well equipped to significantly impact on HIV program activities. Greater involvement of these NGOs and the Nigerian government in HIV programming is an avenue for improvement in the health system.
Acknowledgements
Oleribe OO acknowledges EFMC for institutional support and Institute of Human Virology Nigeria (IHVN) for HIV programme funding. SDT-R is grateful to the National Institute for Health Research (NIHR) Biomedical Facility at Imperial College London for infrastructure support and to the Wellcome Trust ISSF for funding (WSGHF28295).
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- UNAIDS. AIDS by the numbers. AIDS is not over, but it can be. 2016. Accessed 26 January 2017 http://www.unaids.org/sites/default/files/media_asset/AIDS-by-the-numbers-2016_en.pdf
- AIDS.gov. Global Statistics. Accessed 26 January 2017 https://www.aids.gov/hiv-aids-basics/hiv-aids-101/global-statistics/
- UNAIDS. Get on the fast-track - The life-cycle approach to HIV 2016.
- FMOH. Integrated National Guidelines for HIV Prevention, Treatment and Care. National AIDS/STIs Control Programme, Federal Ministry of Health, Abuja, Nigeria. 2014
- Baggaley R, Dalal S, Johnson C, Macdonald V, Mameletzis I, Rodolph M, et al. Beyond the 90-90-90: refocusing HIV prevention as part of the global HIV response. Journal of the International AIDS Society. 2016; 19.
- UNAIDS, 201 UNAIDS. HIV and AIDS estimates (2015).
- Oleribe OO, Oladipo O, Osita-Oleribe P, Nwachukwu C, Nkwopara F, Ekom E, et al. Commonization of HIV/AIDS services in Nigeria: the need, the processes and the prospects. The Pan African Medical Journal. 2014; 19.
- Oleribe O, Ojo O, Agbro M, Nwachukwu C, Olutola A, Osita-Oleribe P, et al. Commonizing HIV Services in Nigeria Through Massive Door-2-Door HIV Testing and Counseling (HTC) in Nigeria. West African College of Physicians: 38th Annual General & Scientific Meeting, Sokoto, Nigeria, July 7 – 11 2014. Book of Abstracts: Pg. 40.
- UNAIDS. 90-90-90-An Ambitious treatment target to help end the AIDS epidemic.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.