A Rare Case Report of Spontaneous Resolution of Hepatic Portal Venous Gas Associated with Cocaine‑Induced Intestinal Ischemia
- *Corresponding Author:
- Dr. Hamid Shaaban
Department of Hematology and Oncology, St. Michael’s Medical Center, 111 Central Avenue, Newark, NJ 07102, USA.
E-mail: hamidshaaban@gmail.com
Abstract
Hepatic portal venous gas (HPVG) is a rare disease entity. It is an ominous finding, usually, associated with intraabdominal ischemic necrosis. It frequently requires emergent surgical intervention. Herein, we present a case of a patient who complained of intense abdominal pain, with radiographic findings of HPVG as a result of cocaine‑induced vascular insufficiency. After 5 h of nonoperative and conservative management, the HPVG spontaneously resolved. The patient clinically improved and was discharged home in a stable condition.
Keywords
Hepatic portal vein, gas, intestinal ischemia.
Introduction
Hepatic portal venous gas (HPVG) was first described in 1978 by Liebman et al. as air in the hepatic and portal vein.[1] The use of modern computed tomography (CT) has resulted in finding HPVG in more benign conditions. It is a worrisome radiological sign, which indicates an underlying critical gastrointestinal condition like ischemia and/or inflammation of the small or large bowel in the majority of the patients. They, usually, require surgical intervention to treat this potential life-threatening condition. Other than ischemia or inflammatory conditions of the bowel many other abdominal conditions can cause HPVG such as pancreatitis, suppurative cholangitis, peptic ulcer disease, volvulus and fecal impaction.[1-4] The prognosis is related to the underlying pathology and the coexistence of a chronic medical disease, such as chronic renal failure, diabetes mellitus or hypertension and not to the HPVG itself.[5,6] Early diagnosis can result in early treatment in a more controlled setting. In a stable patient, a conservative approach can be followed by monitoring of the patient’s clinical condition and laboratory parameters, followed by colonoscopy and repeated CT.[7] In a patient who is clinically deteriorating an emergent explorative laparotomy should be performed.[7] There is a paucity of data describing the radiographic findings of cocaine-induced intestinal ischemia. Our case report describes the unusual presentation of the portal vein air related to recreational cocaine use, which resolved within a few hours with just conservative treatment alone.
Case Report
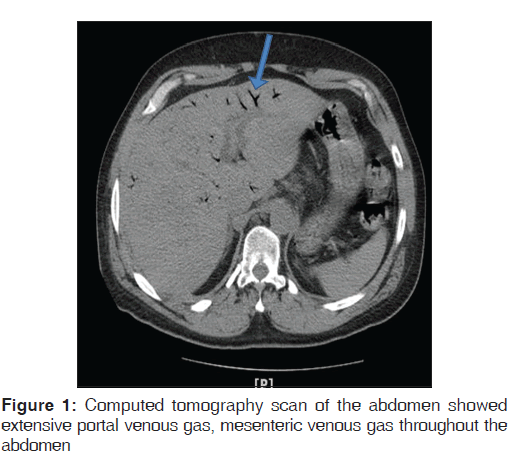
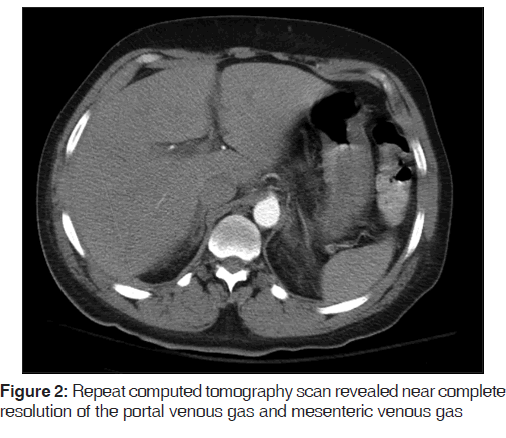
A 51-year-old black male with a past medical history of hypertension and cardiomyopathy (ejection fraction 15%) was brought to the emergency room with complaints of severe stabbing, abdominal pain located in the epigastric area radiating to the right upper quadrant. The pain was precipitated after intravenous cocaine injection. The pain was associated with nausea, nonbloody vomiting, and diarrhea with nonbloody, liquid stools. Pertinent positive finding on physical exam was moderate abdominal tenderness in the epigastric area and right upper quadrant on deep palpation. Lung exam revealed bilateral pulmonary congestion and tachycardia on heart examination. On initial vitals, blood pressure was 188/95 and heart rate was 104. No significant changes in the baseline laboratory studies were noted except urine drug screen was positive for cocaine. CT scan of the abdomen showed extensive portal venous gas, mesenteric venous gas throughout the abdomen [Figure 1]. There was gas also seen in right inguinal region extending into the right hemiscrotum, with wall thickening of the ascending colon. The electrocardiogram showed no ST/T changes. The patient was given a nitroglycerin patch for the elevated blood pressure. Empiric intravenous antibiotics and analgesics were administered. Before the patient was taken to the operating room for the diagnostic laparoscopy to find out the cause of portal vein air, CT scan of the abdomen was repeated and it was done 5 h after the first CT abdomen. The repeat CT scan revealed near complete resolution of the portal venous gas and mesenteric venous gas [Figure 2]. Next day abdominal X-rays were done, which were also negative for extra luminal air. Septic workup including blood culture, urine culture, stool for clostridium difficile, HIV, hepatitis A, B, C was negative. Hepatobiliary iminodiacetic acid scan was also negative for acute cholecystitis and showed a patent biliary tree. After 4 days in the hospital, the patient’s clinical condition improved and he was subsequently discharged home.
Discussion
There are many case reports in the medical literature that have described HPVG but very few of those cases of HPVG had spontaneous resolution within 24 h. One case was reported with complete disappearing of portal venous gas within 24 h.[2] This is the first case report describing cocaine-induced mesenteric ischemia that resulted in HPVG, which spontaneously resolved within 5 h.
Many different etiologies have been reported to cause HPVG, and the mortality rate depends on the cause of HPVG.[1,3] Up to 75% of mortality rates have been reported when bowel ischemia is the cause of HPVG.[8] There is a decline in mortality rate in different case studies from 75% to 29% for HPVG when there is early recognition of HPVG by frequent use of imaging studies followed by early intervention of underlying etiology[7,9-11] The possible reason for the gas in the portal vein, in our patient, was an impaired colonic mucosal barrier caused by transient mesenteric ischemia induced by cocaine-mediated vasoconstriction. The pathophysiology of HPVG is an intricate process in which two or three situations are combined. Our patient’s underlying low ejection fraction (<20%) augmented the risk for bowel ischemia precipitated by the use of cocaine. The gas produced by the colonic bacteria transmigrated through the intestine wall from a mucosal damage in the vein and lymphatics of the colon. These bacteria migrate all the way to the portal vein and liver. These processes are hypothesized to contribute to the pathophysiology of HPVG.[1,3] The trigger insult (i.e. cocaine use) was not of a constant nature, which might explain why the portal vein air, in our patient, resolved quickly within a few hours. One case was reported of HPVG precipitated by cocaine-induced severe bowel ischemia that required surgical intervention, but our patient clinically and radiographically improved solely with conservative management.[12] It is interesting to note that our patient, even though developed transient bowel ischemia due to cocaine use, there was a notable absence of other systemic effects of cocaine like elevated troponins, abnormal elevation of liver enzymes, acute kidney injury or stroke. HPVG is frequently a serious radiographic and clinical finding. Patients typically present with an acute abdomen although, they may occasionally have vague abdominal symptoms, wide-ranging clinical symptoms and laboratory findings. Plain radiographs, CT scans, and ultrasound, can be utilized to diagnose HPVG. CT scans and ultrasonography are optimally better at detecting smaller degrees of HPVG than plain radiographs.[13] Hepatic gas accumulation is usually seen in the anterior and superior aspect of the left lobe of the liver, which is the most anti-dependent portion of the liver. HPVG should be distinguished from pneumobilia in which there is gas in the hepatic biliary tree. In HPVG, gas distribution is typically seen within 2 cm of the liver capsule while, in pneumobilia, gas remains central around the portal hilum and does not extend to within 2 cm of a liver capsule.
Whether the patient should be treated with surgery or just with conservative management depends on the patient’s clinical condition and etiology, which causes the portal venous gas. Bani Hani et al. identified that risk factors like older age, peritoneal signs, and high blood urea nitrogen was correlated with ischemia and necrosis, proposing a potentiality to predict which patients need surgical intervention. It has also been demonstrated that CT findings traditionally suggestive of ischemic HPVG do not diagnose ischemic necrosis accurately enough to reliably identify patients needing surgical intervention.
Our case is very unique in that the HPVG spontaneously resolved radiographically and clinically with only conservative management within 5 h of from the time of diagnosis.
With the increased use of radiographic imaging studies, we are more likely to make the diagnosis of portal venous gas in daily practice. Hence, it is imperative to understand the etiology, pathophysiology and management of portal venous gas. The mainstay of treatment is not always surgical intervention, but the patient should be monitored closely. Conservative management can sometimes result in gradual and rarely spontaneous clinical and radiologic improvement as had happened with our patient.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Liebman PR, Patten MT, Manny J, Benfield JR, Hechtman HB. Hepatic – Portal venous gas in adults: Etiology, pathophysiology and clinical significance. Ann Surg 1978;187:281-7.
- Niki M, Shimizu I, Horie T, Okazaki M, Shiraishi T, Takeuchi H, et al. Hepatic portal venous gas disappearing within 24 hours. Intern Med 2002;41:950-2.
- Kesarwani V, Ghelani DR, Reece G. Hepatic portal venous gas: A case report and review of literature. Indian J Crit Care Med 2009;13:99-102.
- Hepatic portal venous gas: An unusual complication following upper endoscopy and dilation. ACG Case Rep J 2014;1:128-30. Available from: http://www.acgcasereports. gi.org/2014/04/04/hepatic-portal-venous-gas-an-unusua l-complication-following-upper-endoscopy-and-dilation/. [Last accessed on 2014 Oct 23].
- Abboud B, El Hachem J, Yazbeck T, Doumit C. Hepatic portal venous gas: Physiopathology, etiology, prognosis and treatment. World J Gastroenterol 2009;15:3585-90.
- Chan SC, Wan YL, Cheung YC, Ng SH, Wong AM, Ng KK. Computed tomography findings in fatal cases of enormous hepatic portal venous gas. World J Gastroenterol 2005;11:2953-5.
- Nelson AL, Millington TM, Sahani D, Chung RT, Bauer C, Hertl M, et al. Hepatic portal venous gas: The ABCs of management. Arch Surg 2009;144:575-81.
- Kinoshita H, Shinozaki M, Tanimura H, Umemoto Y, Sakaguchi S, Takifuji K, et al. Clinical features and management of hepatic portal venous gas: Four case reports and cumulative review of the literature. Arch Surg 2001;136:1410-4.
- Wiot JF, Felson B. Gas in the portal venous system. Am J Roentgenol Radium Ther Nucl Med 1961;86:920-9.
- Little AF, Ellis SJ. ‘Benign’ hepatic portal venous gas. Australas Radiol 2003;47:309-12.
- Faberman RS, Mayo-Smith WW. Outcome of 17 patients with portal venous gas detected by CT. AJR Am J Roentgenol 1997;169:1535-8.
- Rittenhouse DW, Chojnacki KA. Massive portal venous air and pneumatosis intestinalis associated with cocaine-induced mesenteric ischemia. J Gastrointest Surg 2012;16:223-5.
- Bani Hani M, Kamangar F, Goldberg S, Greenspon J, Shah P, Volpe C, et al. Pneumatosis and portal venous gas: Do CT findings reassure? J Surg Res 2013;185:581-6.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.