Candidiasis, A Rare Cause of Gastric Perforation: A Case Report and Review of Literature
- *Corresponding Author:
- Dr. Francis Ikechukwu Ukekwe
Department Morbid Anatomy, University of Nigeria, Enugu Campus, P.M.B. 01129, Enugu 400241, Nigeria
E-mail: drikukekwe@hotmail.com
Citation: Ukekwe FI, Nwajiobi C, Agbo MO, Ebede SO, Eni AO. Candidiasis, a rare cause of gastric perforation: A case report and review of literature. Ann Med Health Sci Res 2015;5:314-6.
Abstract
Fungi are unusually rare causes of gastric perforation, with most cases of gastric perforation occurring as complications of peptic ulcer disease (PUD), nonsteroidal anti‑inflammatory drugs (NSAIDs) and gastric neoplasms. Here, we report the case of a 70‑year‑old Nigerian male who presented with severe epigastric pain, with no associated history of PUD, NSAIDs use or gastric neoplasm. An emergency exploratory laparotomy was performed and a gastric perforation was discovered and repaired. Histopathological examination of the gastric perforation edge biopsy revealed an intense Candida growth consisting of numerous fungal spores and hyphae invading and destroying the gastric wall. He was subsequently treated with fluconazole antifungal and discharged home after an uneventful postoperative period.
Keywords
Candidiasis, Fluconazole, Gastric perforation, Peritonitis, Surgical pathology
Introduction
Most cases of gastric perforation occur as complications of peptic ulcer disease (PUD), nonsteroidal anti-inflammatory drugs and gastric neoplasms.[1] Though Candida species are regarded as normal commensals of the gastrointestinal tract, infections of the gastrointestinal tract do very rarely occur and have been reported as very rare causes of gastric perforation, seen mostly in immunocompromised and debilitated patients as well as in healthy persons who indulge in habitual use of strong antacids.[1,2] A prudent search of literature show that this condition has not been previously reported in Nigeria. Here we report the first Nigerian case of gastric perforation from invasive gastric candidiasis in a 70-year-old Nigerian male and review the relevant literature.
Case Report
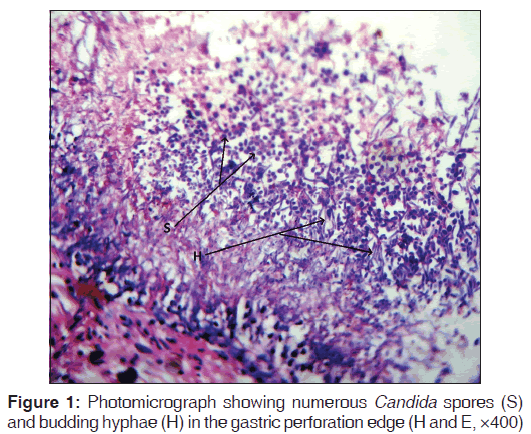
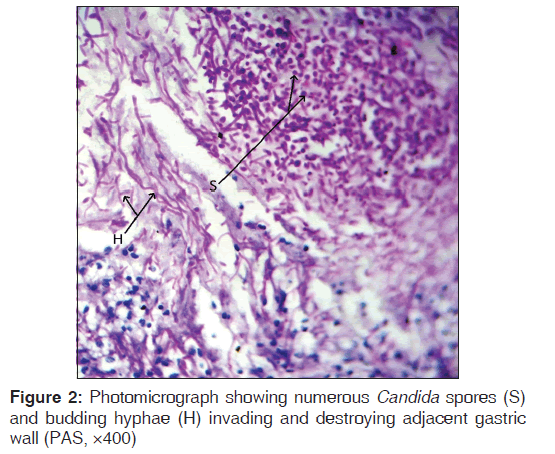
A 70-year-old Nigerian man presented at the emergency unit of our hospital with a 2 weeks history of abdominal pain. The pain was epigastric; severe, deep-seated, progressive, non-radiating, not relieved by food intake and not associated with vomiting or diarrhea. His condition worsened 5 days to presentation with generalized abdominal pain and abdominal wall rigidity. There was no change in bowel habit, no blood in stool, no abdominal distension, no associated fever, weight loss, alcohol binge or trauma. No history of previous medication, PUD or abdominal surgery, not a known diabetic, hypertensive, epileptic, asthmatic or sickler but has a history of moderate alcohol and cigarette use of more than 20 years. On clinical examination was an elderly man, conscious and alert but in obvious painful distress. He was afebrile, not pale, anicteric, not cyanosed, no pedal edema but was moderately dehydrated. The respiratory rate was 60 breaths per minute, pulse rate – 120 beats per minute and blood pressure - 100/70 mmHg. The abdomen was flat, tense, and with minimal movement on respiration, marked generalized abdominal tenderness, rebound tenderness, and rigidity. The examination of the liver, spleen, kidneys, and rectum were unremarkable but the prostate was moderately enlarged. An impression of peritonitis 2° to perforated PUD was made and he was placed on omeprazole, tramadol, paracetamol, flagyl, ceftriaxone, hydrocortisone, and fluid hydration. The preoperative laboratory investigations were hemoglobin concentration - 13 g/dl, serum electrolyte concentration - sodium (Na+) - 138 mmol/L, potassium (K+) - 4.1 mmol/L, bicarbonate (HCO3 −) - 20 mmol/L, chloride (Cl−) - 108 mmol/L, and negative HIV 1 and 2 antibodies. Abdominal ultrasonography showed intraperitoneal echo-rich collection with dilated small bowel loops. The patient measured 1.67 m tall, weighed 60 kg, and had a body mass index of 21.5 kg/m2. An emergency exploratory laparotomy was performed and a 3.1 cm by 1 cm gastric perforation covered with fibrinous exudate was seen with vegetative material within the peritoneum. An edge biopsy of the ulcerated perforation was taken and an omental patch repair and peritoneal lavage with normal saline was done. The gross examination of the specimen showed pieces of irregular grayish white tissues aggregating to 0.7 cm × 0.4 cm × 0.2 cm. The microscopic examination of the specimen showed an intense Candida growth consisting of numerous spores and budding hyphae [Figures 1 and 2] invading and destroying the gastric wall with marked granulation tissue formation, intense mixed inflammatory cell infiltration consisting of mainly eosinophils, macrophages, plasma cells, and lymphocytes. No Helicobacter pylori like organisms or atypical cellular proliferations were seen. A histopathological diagnosis of gastric perforation from invasive candidiasis was made and the patient was subsequently treated with fluconazole, clindamycin, ciprofloxacin, levofloxacin, imipenem, tamsulosin, and discharged home after an uneventful postoperative period.
Candida species are a major constituents of the normal commensal flora of the gastrointestinal tract in humans. They cause infections mostly in immunocompromised and severely ill patients, patients on steroid therapy and chemotherapy, diabetics, and HIV/AIDS patients,[1,2] and very rarely in healthy persons who indulge in habitual use of strong antacids.[2] The level of the gastrointestinal fungi is normally controlled by beneficial commensal gut bacteria and low pH but regular use of antacids as well as hyperglycemia can lead to an increased risk of fungal overgrowth, infection and invasion leading to multiple ulcers and perforation.[2,3] The bacterial-fungal balance is also upset by improper usage of antibiotics or compromised immune system leading to Candida overgrowth and infection. Diagnosis of this condition is however, difficult, due to the prevalence of colonization with no accompanying infection, nonspecific symptoms, and variability of presentation.[4] Our patient was immunocompetent, apparently healthy, and without the usual associations mentioned above. Invasive Candida infections are characterized by fever and shock along with low blood pressure, an elevated heart rate, respiratory distress, and multi-organ failure.[1] It is a serious medical emergency requiring an immediate medical attention. A high index of suspicion is required by the attending clinician as well as the pathologist studying the biopsy edge of such perforations for early and accurate diagnosis of such presentations. Fungal infections from Candida species constitute the fourth most common cause of nosocomial bloodstream infections, and are associated with high morbidity and mortality in critically ill patients, particularly those who have recently undergone extensive gastro-abdominal surgery.[5] An early diagnosis can prevent fatal complications as have been reported,[6] but in our case, the diagnosis was made evidently early enough and treatment commenced thereby forestalling its associated high morbidity and mortality. Despite the availability of new, rapid, sensitive, and probably expensive methods for diagnosing fungal infection,[7] histopathologic examination of the perforation edge biopsy remains a major diagnostic tool allowing observation of invasive budding hyphae (virulence factor) in tissues which suggest real overgrowth and a pathogenic role.[4,8,9] This technique was used in the diagnosis of our case with the classical budding hyphae and spores of Candida demonstrated on microscopy [Figures 1 and 2]. The unavailability of immunohistochemistry, in situ hybridization and direct sequencing (polymerase chain reaction) for fungal studies in our center and our inability to do microbiological culture because the perforation edge biopsy was formalin fixed limited further Candida classification into species. The absence of previously reported associations in our patient could point to the presence of other predisposing factors or the presence of a more virulent Candida strain in the etiopathogenesis of gastric perforation from gastrointestinal candidiasis.
Conclusion
This report underscores fungal etiology as an unusually rare but important cause of the gastric perforation even in apparently healthy patients. Early diagnosis and treatment would reduce the significant mortality associated with this condition which is hitherto unreported in our environment.
References
- Gupta N. A rare cause of gastric perforation-Candida infection: A case report and review of the literature. J Clin Diagn Res 2012;6:1564-5.
- Bakhshi GD, Borisa AD, Shaikh AS, Thadeshwar NR, Kher Y, Kapadnis LA. Invasive gastric candidiasis with perforation. Bombay Hosp J 2011;53:264-65.
- Buddington RK, Williams CH, Chen SC, Witherly SA. Dietary supplement of neosugar alters the fecal flora and decreases activities of some reductive enzymes in human subjects. Am J Clin Nutr 1996;63:709-16.
- Di Carlo P, Di Vita G, Guadagnino G, Cocorullo G, D’Arpa F, Salamone G, et al. Surgical pathology and the diagnosis of invasive visceral yeast infection: Two case reports and literature review. World J Emerg Surg 2013;8:38.
- Tortorano AM, Peman J, Bernhardt H, Klingspor L, Kibbler CC, Faure O, et al. Epidemiology of candidaemia in Europe: Results of 28-month European Confederation of Medical Mycology (ECMM) hospital-based surveillance study. Eur J Clin Microbiol Infect Dis 2004;23:317-22.
- Minoli G, Terruzzi V, Butti G, Frigerio G, Rossini A. Gastric candidiasis: An endoscopic and histological study in 26 patients. Gastrointest Endosc 1982;28:59-61.
- Ohrmalm C, Eriksson R, Jobs M, Simonson M, Strømme M, Bondeson K, et al. Variation-tolerant capture and multiplex detection of nucleic acids: Application to detection of microbes. J Clin Microbiol 2012;50:3208-15.
- Sangoi AR, Rogers WM, Longacre TA, Montoya JG, Baron EJ, Banaei N. Challenges and pitfalls of morphologic identification of fungal infections in histologic and cytologic specimens: A ten-year retrospective review at a single institution. Am J Clin Pathol 2009;131:364-75.
- Ruchi A, Hemlata K, Parveen R, Sanjay V. A rare case of invasive gastric candidiasis causing perforation and peritonitis. J Krishna Inst Med Sci Univ 2015;4:183-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.