Clinical and Economic Evaluation of Laparoscopically Assisted Percutaneous Endoscopic Gastrostomy Versus Open Gastrostomy in Patients for Whom Endoscopic Gastrostomy Is Difficult
Received: 31-Jan-2025, Manuscript No. Amhsr-25-163908; Editor assigned: 03-Feb-2025, Pre QC No. Amhsr-25-163908 (PQ); Reviewed: 17-Feb-2025 QC No. Amhsr-25-163908 (Q); Revised: 24-Feb-2025, Manuscript No. Amhsr-25-163908 (R); Published: 03-Mar-2025
Citation: Kameyama A, et al. Clinical and Economic Evaluation of Laparoscopically Assisted Percutaneous Endoscopic Gastrostomy versus Open Gastrostomy in Patients for Whom Endoscopic Gastrostomy Is Difficult. Ann Med Health Sci Res. 2025; 1097-1101
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Percutaneous endoscopic gastrostomy is a widely used technique for long-term enteral nutrition. However, some patients have anatomical or pathological conditions making standard percutaneous endoscopic gastrostomy infeasible. Traditionally, open gastrostomy has been performed in these cases, although it is more invasive. Laparoscopically Assisted Percutaneous Endoscopic Gastrostomy (LAPEG) has recently been introduced as an alternative. This study aimed to compare the surgical outcomes and economic feasibility of LAPEG and open gastrostomy in patients with conditions that render standard percutaneous endoscopic gastrostomy unfeasible. Materials and methods: A retrospective review was conducted of all patients undergoing gastrostomy at our institution between January 2016 and February 2025. Among 378 total gastrostomies, sixteen were classified as “difficult”, meaning that endoscopic transillumination or the finger sign could not be confirmed, or preoperative imaging revealed organs overlapping the stomach. Data collected included operative time, blood loss, perioperative complications, and hospital economic outcomes based on Japan’s public insurance reimbursement. Statistical analyses were performed using t-tests, with statistical significance defined as P<0.05. Results: Sixteen patients were analyzed (four LAPEG and twelve open gastrostomy). Median operative times (49 min vs. 55.5 min) and blood loss (3.5 g vs. 5 g) did not differ significantly between the LAPEG and open groups, respectively. Three perioperative complications occurred in the open group (bowel pneumatosis in two patients and aspiration pneumonia in one), while none were observed in the LAPEG group. Although LAPEG incurred higher material costs and a significantly higher total hospital cost (162,138 yen vs. 145,053 yen, P=0.00365), the hospital’s gross profit was similar between groups (13,839 yen vs. 13,580 yen, P=0.606). Conclusion: Within the limitations of this small, retrospective study, LAPEG was comparable to open gastrostomy in terms of operative time and surgical outcomes. LAPEG showed higher material costs, but overall hospital profit remained similar. Large-scale, prospective investigations are warranted to validate these findings and further clarify the clinical and economic benefits of LAPEG in patients with difficult indications for percutaneous endoscopic gastrostomy.
Keywords
Laparoscopically assisted PEG; Open gastrostomy; Percutaneous endoscopic gastrostomy; Cost analysis; Difficult PEG
Introduction
Gastrostomy plays a crucial role in patients who require long-term nutritional management but cannot maintain adequate oral intake. Percutaneous endoscopic gastrostomy is widely considered the standard approach due to its relatively low invasiveness and high success rate [1]. However, standard percutaneous endoscopic gastrostomy cannot be safely performed in certain patients with challenging anatomical or pathological conditions, such as extensive adhesions or an overlapping transverse colon.
Traditionally, open gastrostomy has been performed for these “difficult” cases, yet open surgery is more invasive and carries a higher risk of postoperative morbidity. Laparoscopically Assisted Percutaneous Endoscopic Gastrostomy (LAPEG) has emerged as an alternative, allowing adhesiolysis, direct visualization of the stomach, and precise placement of the gastrostomy tube under laparoscopic guidance. Although there is increasing interest in LAPEG, few studies have evaluated its clinical and economic impact in “difficult percutaneous endoscopic gastrostomy” cases.
Therefore, we conducted a retrospective analysis comparing open gastrostomy and LAPEG in terms of operative time, complications, and financial feasibility under Japan’s public health insurance reimbursement system [2].
Materials and Methods
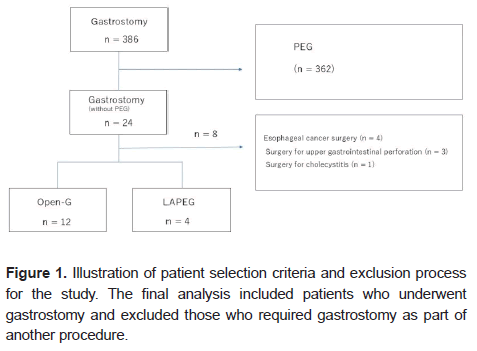
A retrospective chart review was conducted for patients undergoing gastrostomy (tube placement) at Aizawa Hospital between January 2016 and February 2025. Among 378 gastrostomy procedures, sixteen were classified as “difficult percutaneous endoscopic gastrostomy,” defined by failure to confirm the transillumination or finger sign on endoscopy or by imaging evidence that an organ (e.g., transverse colon) overlapped the stomach. Patients requiring a gastrostomy as part of another concurrent procedure (e.g., combined surgeries) were excluded. (Figure 1)
We examined patient demographics, baseline clinical status, and American Society of Anesthesiologists (ASA) classifications. Outcome measures included operative time, blood loss, perioperative complications, and hospital gross profit. The choice between open gastrostomy and LAPEG depended on surgeons’ discretion, especially in earlier years when laparoscopic approaches were not fully standardized.
Under Japan’s public health insurance system, fees reimbursed to hospitals include surgical and anesthesia costs. We calculated total hospital cost as the sum of these reimbursements plus major surgical material costs. Capital expenditures (e.g., operating room equipment) and personnel costs (e.g., nursing staff) were excluded. We defined “hospital gross profit” as total reimbursement minus the non-reimbursed surgical materials for each procedure.
Statistical analyses were performed using t-tests with significance set at P<0.05. All statistical analyses were performed using EZR, a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Surgical procedures
Open gastrostomy
Under general anesthesia, a midline upper abdominal incision (typically 8–16 cm) was made. The stomach was visualized directly, and a 20-French balloon-type Foley catheter was introduced through the left lateral abdominal wall and fixed using the Stamm method. The gastric wall was sutured to the abdominal wall to ensure stability. About 1 month later, the balloon catheter was typically exchanged for a commercial button-type gastrostomy tube using a guidewire.
Laparoscopically Assisted Percutaneous Endoscopic Gastrostomy (LAPEG)
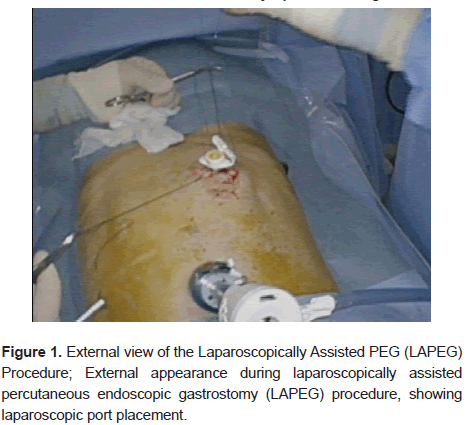
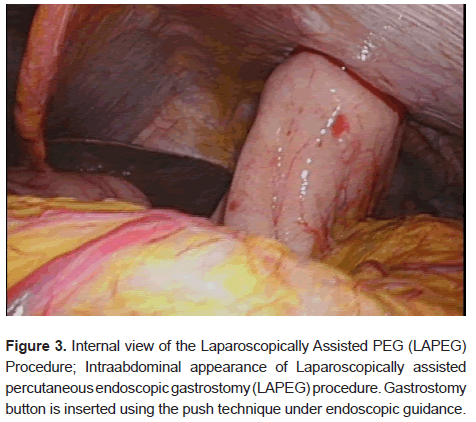
LAPEG was performed under general anesthesia in the supine position. Surgeons inserted two or three laparoscopic ports near the umbilicus (Figure 2). Adhesiolysis was carried out as needed. An endoscope was passed into the stomach, and the ideal gastrostomy site was identified under combined laparoscopic and endoscopic guidance. (Figure 3). The “push” technique was used to place a button-type gastrostomy tube (EndoVive Bumper Button) during the initial procedure. Laparoscopic visualization minimized the risk of inadvertent injury to other organs.
Results
The incidence of these complications did not differ significantly between the two cohorts.
Patient demographics
Sixteen patients (four LAPEG and twelve open gastrostomy) met the inclusion criteria. In the LAPEG group, all were male with a mean age of seventy-nine years (range: seventy-four to eighty-five years). The most frequent underlying diagnoses were neurodegenerative diseases, such as Parkinson’s disease or progressive supranuclear palsy. The open gastrostomy group comprised twelve patients (eight males, four females) with a mean age of seventy-one years (range: sixty-one to eighty-six years). Baseline characteristics, including ASA classification, showed no significant intergroup differences (Table 1).
| Parameter | Open-G (n=12) | LAPEG (n=4) |
|---|---|---|
| Sex (M/F) | 8/4 | 4 / 0 |
| Age (median [range]) | 71.5 [61–86] | 79 [74–85] |
| ASA Classification (2/3) | 7/5 | 2/2 |
| Primary underlying disease | ||
| Neurodegenerative disease | 6 | 4 |
| Cerebrovascular disease | 3 | |
| Head and neck cancer | 2 | |
| Hiatal hernia | 1 | |
| Reason for PEG difficulty | ||
| Negative finger sign | 5 | 2 |
| Transverse colon overlying the stomach | 3 | 2 |
| Esophageal stricture after RT | 1 | |
| Esophageal cancer/perforation | 1 | |
| Severe hiatal hernia | 1 | |
| Tracheoesophageal fistula | 1 | |
Note:*Neurodegenerative diseases include Parkinson’s disease, progressive supranuclear palsy, multiple system atrophy, Amyotrophic Lateral Sclerosis (ALS), spinocerebellar degeneration, and related disorders.
Table 1: presents demographic and clinical characteristics of patients undergoing Open-G and LAPEG procedures
Operative time and perioperative complications
Median operative time was forty-nine minutes (LAPEG) versus fifty-five and one-half minutes (open), with no significant difference (P=0.977). Blood loss was modest in both groups (3.5 g vs. 5 g) and did not differ significantly (P=0.121). No perioperative complications occurred in the LAPEG group. In the open group, three complications were noted: two cases of bowel pneumatosis and one case of aspiration pneumonia. The frequency of these complications did not differ significantly between the groups (Table 2).
| Parameter | Open-G (n=12) | LAPEG (n=4) | p-value |
|---|---|---|---|
| Operative time (min) (median [range]) | 55.5 (43–75) | 49 (42–94) | 0.977 |
| Blood loss (g) (median [range]) | 5 (2–10) | 3.5 (2–5) | 0.121 |
| Postoperative complications | 3 (25%) | 0 (0%) | 0.529 |
| Bowel pneumatosis/paralytic ileus | 2 | - | - |
| Aspiration pneumonia | 1 | - | - |
Table 2: Operative and postoperative outcomes in Open-G versus LAPEG procedures.
Insurance reimbursement, costs, and hospital gross profit
Total hospital cost (including reimbursed surgical and anesthesia fees plus the cost of key surgical materials) was significantly higher for LAPEG (162,138 yen) compared to open gastrostomy (145,053 yen, P=0.00365) (Table 3). Despite this higher total cost, the hospital’s gross profit calculated after subtracting the cost of non-reimbursed materials did not differ significantly between groups (13,839 yen vs. 13,580 yen, P=0.606). Material expenses were higher in the LAPEG group, largely reflecting the cost of disposable laparoscopic equipment and the button-type gastrostomy device. We did not account for operating-room overhead or personnel costs, so the true economic impact may vary.
| Parameter | Open-G (n=12) | LAPEG (n=4) | p-value |
|---|---|---|---|
| Surgical fee (JPY) (mean [range]) | 61,988 (52,530–69,350) | 72,000 (71,020–73,790) | 0.00125 |
| Anesthesia fee (JPY) (mean [range]) | 76,753 (6,647–89,55) | 80,760 (78,320–82,210) | 0.18 |
| Anesthesia management (JPY) (mean [range]) | 6,313 (3,000–10,500) | 9,375 (5,250–11,250) | 0.107 |
| Total cost (JPY) (mean [range]) | 145,053 (13,571–169,40) | 162,138 (161,050–163,780) | 0.00365 |
| Gross profit from surgical costs (JPY) (mean [range]) | 135,803 (12,646–160,150) | 138,39 (137,300–140,030) | 0.606 |
Table 3: Illustrates the cost comparison, including surgical, anesthesia, and total costs between Open-G and LAPEG procedures.
Discussion
Open surgical Gastrostomy (Open-G) was first reported by Stamm in 1894 as a method for long-term enteral feeding and gastric decompression. Subsequently, PEG was introduced by Gauderer et al., in 1980 and rapidly gained widespread acceptance due to its minimally invasive nature, technical simplicity, and high success rate (exceeding 95%) [3-5]. However, many of the patients who require PEG have severe underlying diseases and limited physiological reserves, which can lead to a substantial risk of complications [6,7]. In particular, serious complications such as inadvertent puncture of the colon or small intestine and liver injury have been reported [8,9]. These events often occur at the time of gastrostomy placement but may initially go unnoticed.
To avoid injury to other organs, it is crucial to confirm transillumination by endoscopy (illumination sign) and the indentation caused by finger pressure on the abdominal wall (finger sign). In cases where these signs cannot be confirmed, the risk of accidental puncture of other organs increases, making safe PEG placement difficult. At our institution, confirming transillumination of the upper gastrointestinal endoscope through the abdominal wall, along with visible indentation by finger pressure under endoscopy, is a prerequisite for PEG. Patients not meeting these criteria such as those with stenosis or perforation of the upper gastrointestinal tract, or CT findings indicating that the liver or transverse colon lies anterior to the stomach are categorized as having “difficult PEG” and undergo surgical gastrostomy in the Department of Gastrointestinal Surgery.
We have traditionally performed open gastrostomy for PEG-difficult patients. However, the need for a large incision and the cumbersome guidewire manipulation required when replacing a balloon catheter with a commercial kit have been noted as drawbacks.
LAPEG, first described by Raaf et al., eliminates the risk of blind injury to abdominal organs and enables optimal selection of the gastrostomy site on both the stomach and anterior abdominal wall [10]. By providing direct visualization under laparoscopy, the procedure allows for the stomach to be pulled into a normal position using minimal incisions, thereby avoiding organs that overlap the stomach. In addition, standard PEG kits can be used, simplifying post-procedure management [11-15].
In this study, we compared outcomes between LAPEG and open gastrostomy (Open-G) in patients for whom PEG was deemed difficult. Although some reports suggest that LAPEG may reduce operative time and complications, the present analysis found no substantial difference between LAPEG and Open-G in terms of operative time or perioperative complication rates. However, the smaller incision in the LAPEG group may offer advantages in postoperative pain control and cosmetic outcomes.
While LAPEG showed a higher reimbursement in terms of surgical fees, calculations of gross profit after subtracting material costs revealed no significant difference between the two groups. This finding suggests that the cost-effectiveness of LAPEG may be influenced by the higher cost of surgical materials and button-type gastrostomy devices. However, the present study did not fully account for factors such as personnel expenses for endoscopic staff or the overhead costs associated with acquiring and maintaining laparoscopic and endoscopic equipment. Therefore, more detailed economic evaluations are required to determine the true impact on clinical finances. From a practical perspective, Open-G can be performed by surgeons independently, whereas LAPEG necessitates collaboration with endoscopy personnel and equipment, potentially inflating costs related to staffing and resources.
In summary, when PEG is difficult, LAPEG offers certain practical advantages by allowing safe gastrostomy placement with the possibility of adhesiolysis and direct gastric repositioning under laparoscopic guidance. Moreover, a smaller incision and the early use of button-type tubes may contribute to improved patient quality of life. However, given that our facility only recently standardized laparoscopic approaches, the choice between Open-G and LAPEG depended largely on the surgeon’s discretion. Consequently, selection bias cannot be ruled out, and larger-scale, prospective studies are needed to draw more definitive conclusions.
Limitations
This study was conducted at a single center with a small sample size especially in the LAPEG group which limits the statistical power. The decision-making process regarding the choice of Open-G or LAPEG was not governed by a strict protocol and may have been influenced by the lack of a standardized laparoscopic approach in our hospital until 2023.
Our cost analysis was based on Japanese public health insurance fees and may not be generalizable to other healthcare systems. Furthermore, we did not include personnel costs, overheads for laparoscopic equipment, or objective measures of postoperative pain in our analysis. Thus, the cost-effectiveness findings should be interpreted with circumspection. Therefore, caution is warranted in interpreting the cost-effectiveness findings. Future multicenter or prospective studies incorporating larger patient populations, more detailed operative data, and comprehensive cost calculations (including personnel and equipment costs) will be essential for a thorough evaluation.
Conclusion
In this study comparing LAPEG and Open-G for patients with difficult PEG, there were no significant differences in operative time or perioperative complications. We found no significant difference in hospital gross profit between the two methods, suggesting that LAPEG can be a financially viable option despite its higher upfront costs.
However, our sample size was small and the study is exploratory, limiting the strength of any firm conclusions. Given the potential advantages of smaller incisions, it remains a promising alternative for patients in whom standard PEG is not feasible. These findings, while preliminary, underscore the need for future research. Further large-scale, prospective studies are warranted to clarify the clinical and economic impacts of LAPEG and to guide optimal patient selection.
References
- Gauderer MW, Ponsky JL, Izant RJ. Gastrostomy without laparotomy: A percutaneous technique. J Pediatr Surg. 1980;15(6):872-875.
[Crossref] [Google Scholar] [PubMed]
- Ministry of Health, Labour and Welfare (MHLW). Overview of medical service regime in Japan. 2025.
- Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg. 1988;207(5):598-603.
[Crossref] [Google Scholar] [PubMed]
- Bergstrom LR, Larson DE, Zinsmeister AR, Sarr MG, Silverstein MD, et al. Utilization of surgical gastrostomies and jejunostomies in an era of percutaneous endoscopic gastrostomy: A population-based study. Mayo Clin Proc. 1995;70(9):829-836.
[Google Scholar] [PubMed]
- Fanelli RD, Ponsky JL. A simplified technique for percutaneous endoscopic gastrostomy. Surg Endosc. 1992;6(5):261-262. doi:10.1007/BF02498818.
[Crossref] [Google Scholar] [PubMed]
- Larson DE, Burton DD, Schroeder KW, et al. Percutaneous endoscopic gastrostomy: indications, success, complications and mortality in 314 consecutive patients. Gastroenterology. 1987;93(1):48-52.
[Google Scholar] [PubMed]
- Miller ER, Castlemain B, Lacqua JF, et al. Percutaneous endoscopic gastrostomy: Results in 316 patients and review of literature. Surg Endosc. 1989;3(4):186-190.
[Crossref] [Google Scholar] [PubMed]
- Kanie J. A study of postoperative complications in endoscopic gastrostomy: Analysis of cases over a 10-year period. Gastroenterol Endosc. 2003;45(9):1267-1272.
[Crossref]
- Trenschel R, Geraghty F, Mirza J, Chacon D, et al. Percutaneous endoscopic gastrostomy misplacement in the transverse colon of a neurocognitively compromised patient. Cureus. 2022;14(2):e22063.
[Crossref] [Google Scholar] [PubMed]
- Raff JH, Manney M, Okafor E, Gray L, Chari V. Laparoscopic Placement of A Percutaneous Endoscopic Gastrostomy (PEG) feeding tube. J Laparoendosc Surg. 1993;3(6):411-414.
[Crossref] [Google Scholar] [PubMed]
- Kusumoto E, Sugiyama M, Ota M. Laparoscopic-assisted percutaneous endoscopic gastrostomy: Report of three cases [Japanese]. Fukuoka Igaku Zasshi. 2015;106(9):262-265.
- Thaker AM, Sedarat A. Laparoscopic-assisted percutaneous endoscopic gastrostomy. Curr Gastroenterol Rep. 2016;18(9):46.
[Crossref] [Google Scholar] [PubMed]
- Tanaka T, Ueda T, Yokoyama T, Sadamitsu T, Yoshimur A, et al. Laparoscopic percutaneous endoscopic gastrostomy is useful for elderly. JSLS. 2019;23(2):e2019.00011.
[Crossref] [Google Scholar] [PubMed]
- Lodin D, Gupta AK, Rubay D, Genuit T, Hus N, et al. The effectiveness of laparoscopic-assisted percutaneous endoscopic gastrostomy in patients with unfavorable anatomy: A single-center retrospective cohort study. Cureus. 2020;12(1):e6647.
[Crossref] [Google Scholar] [PubMed]
- Tomioka K, Fukoe Y, Lee Y, Lee M, Aoki T, et al. Clinical Evaluation of Laparoscopic-Assisted Percutaneous Endoscopic Gastrostomy (LAPEG). Int Surg. 2014;99(6):623-628.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.