Considerations in Management of Rhegmatogenous Retinal Detachment in One Eyed Pregnant Females: A Report of Two Cases
- *Corresponding Author:
- Dr. Ashish Mitra
Sadguru Netra Chikitsalaya, Jankikund, Chitrakoot - 210 204, Madhya Pradesh, India.
E-mail: ashishmitra14@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
The aim of this case report is to discuss issues related to management of one eyed pregnant female. A 26‑year‑old female (Patient A) and 28‑year‑old female (Patient B) both in second trimester and one eyed presented to our outpatient department with diminution of vision due to rhegmatogenous retinal detachment (RRD). Retina was attached in Patient A following scleral buckling surgery but Patient B required pars plana vitrectomy with silicon oil tamponade. Best corrected visual acuity in both patients did improve from 1/60 to 6/24 and 6/18, respectively at 6 months follow‑up. Exudative RDs are known to occur in pregnancy as a complication of preeclampsia, but RRD in pregnancy although co‑incidental poses certain challenge with regard to management of such cases especially if the patient is one‑eyed. Things to consider for management include (1) type of anesthesia (2) surgical positioning (3) positioning after surgery (4) anti‑glaucoma medication if required (5) corticosteroid treatment in pregnancy (6) to provide them ambulatory vision as early as possible. With proper management and monitoring it is possible to provide them with early ambulatory vision without offering any harm to her pregnancy and fetus.
Keywords
Ambulatory vision, One-eyed, Pregnancy, Rhegmatogenous retinal detachment
Introduction
Retinal detachment (RD) occurs when subretinal fluid accumulates in the potential space between the neurosensory retina and the underlying retinal pigment epithelium. Exudative detachments as a complication of eclampsia are seen in pregnancy, but rhegmatogenous RD (RRD) in pregnancy is co-incidental and very few reports are there in the literature for the management of such patients.[1,2] We hereby present two cases of one eyed females who were in the second trimester of pregnancy and presented to us with RRD. The aim of this case report is to discuss issues related to management of such patients and provide ambulatory vision as early as possible.
Case Report
We present two cases of macula-off RRD in one eyed pregnant patients.
Patient A
A 26-year-old female who was 5 months pregnant presented to our outpatient department (OPD) with loss of vision in the right eye (RE) since 2 months and left eye (LE) since 2 years. Best corrected visual acuity (BCVA) in RE was 1/60 and LE had a perception of light (PL). On examination, RE had RD with lattices and LE had exotropia of 30 prism diopter and old RD with multiple lattices. She was advised for surgery of the RE. LE surgery was planned at a later date. Exotropia evaluation was done by strabismus team of our institute.
Patient B
A 28-year-old female who was 6½ months pregnant presented to our OPD with history of loss of vision LE since 8 days (visual acuity in LE was 1/60). RE denied PL since childhood following trauma. She underwent cataract surgery in LE 2 years back. Following diminishing of vision since last 8 days, she went to a local ophthalmologist where she was wrongly diagnosed as having posterior capsular opacification for the cause of diminished vision, and Yag capsulotomy was done. She then presented to our center and was diagnosed to have RRD with horseshoe tear at the edge of the lattice and was advised surgery for the same.
Table 1 shows surgical details and postoperative visual acuity.
| Patients | Date of presentation | SB + SRFDwas done on | PPV + FAX + EL +SOI was done on | BCVA on discharge | BCVA (follow-upvisit at 6 months) |
|---|---|---|---|---|---|
| A | 04/01/2014 | 07/01/2014 | Not required | 1/60 | 6/24 |
| B | 06/01/2014 | 08/01/2014 | 10/01/2014 | 1/60 | 6/18 |
SB: Scleral buckle, SRFD: Subretinal fluid drainage, PPV: Pars plana vitrectomy, FAX: Fluid air exchange, EL: Endolaser, SOI: Silicon oil insertion, BCVA: Best corrected visual acuity
Table 1: Surgical details and postoperative visual acuity
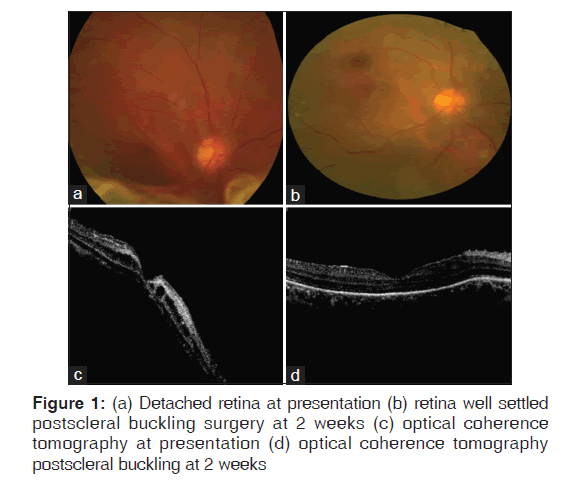
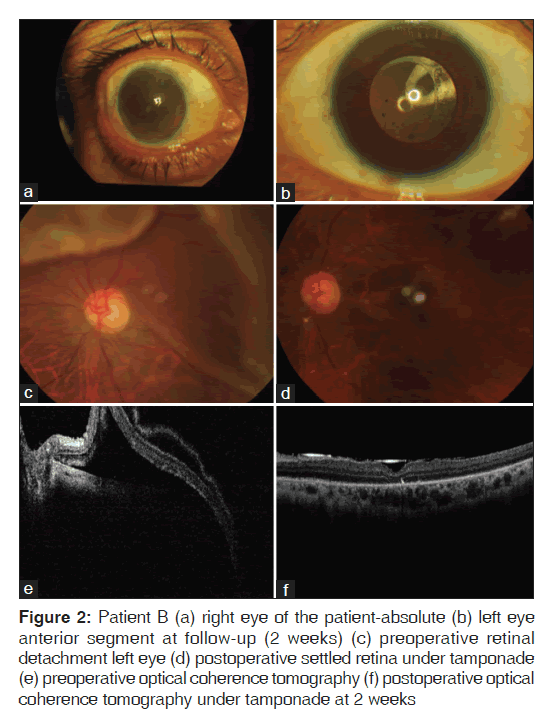
Retina was attached in Patient A following scleral buckling surgery [Figure 1] but Patient B required pars plana vitrectomy with silicon oil tamponade [Figure 2]. Time duration in both procedures was about an hour. Silicon oil being optically clear was preferred over gas as it would provide ambulatory vision soon after the surgery (patient being one-eyed). Silicon oil was removed after 2 months of delivery.
Figure 2: Patient B (a) right eye of the patient-absolute (b) left eye anterior segment at follow-up (2 weeks) (c) preoperative retinal detachment left eye (d) postoperative settled retina under tamponade (e) preoperative optical coherence tomography (f) postoperative optical coherence tomography under tamponade at 2 weeks
Both patients were discharged on topical steroids drops with two hourly instillation and cycloplegics 3 times a day. They did not require anti-glaucoma medication and had uneventful vaginal delivery.
At 6 months follow-up:
• Patient A - 2 months postvaginal delivery, retina was attached with BCVA of 6/24
• Patient B - 4 months postvaginal delivery, the retina was attached with BCVA of 6/18.
Discussion
RD could be treated either by carrying out scleral buckling or doing pars plana vitrectomy and silicon oil/gas tamponade. Management of RRD, in pregnancy needs special consideration as both patients were one-eyed and any delay in surgery would alter the visual prognosis, and at the same time managing such patients without causing any harm to their pregnancy and fetus. The questions on our mind were (1) type of anesthesia (2) posture during surgery (3) posture following surgery (4) safety of medications in pregnancy (5) to provide them vision as early as possible.
Type of anesthesia
Surgical anesthesia in pregnancy poses some risks to both mother and fetus. Maternal physiology is altered such that plasma volume and cardiac output are greater, and peripheral vascular resistance is reduced, thus lowering blood pressure. In addition, supine position in the second and third trimester can induce profound hypotension due to aortic and vena caval compression by the uterus. Ideally, the pregnant women should be placed on her left side. She should be well hydrated and oxygenated before anesthesia induction to prevent maternal hypotension and hypoxia.[3]
A pregnant woman can develop hypoxia and hypercapnia more quickly than in a nonpregnant woman. Furthermore, airway management is hard in pregnant patients with breast enlargement, weight gain, and laryngeal edema.[3] The risk for gastric acid aspiration through anesthesia induction is raised in gravid patients as gastroesophageal sphincter tone, and intestinal motility are reduced.[3]
For general anesthesia cases, narcotics, paralyzing agents, and inhaled anesthetic agents can negatively affect the fetus.[3] The side effects of these medications make local anesthesia (LA) much more preferable. Regarding LA, literature has shown that lidocaine has not been associated with any adverse effect on the fetus.[4]
Surgical positioning such as supine position in the second and third trimester can induce profound systemic hypotension due to aortic and vena caval compression by the uterus. Consideration should be given to rotating the patient’s hips, abdomen, and thighs while maintaining a normal head position for ophthalmic surgery.[3]
Positioning after surgery
With the use gas like C3F8, it is important for the patients to maintain prone position for tamponade to be effective, but it is difficult for a pregnant female to maintain such posture.
Anti-glaucoma medicine in the second trimester
In the second trimester, brimonidine can be applied, and beta-blockers can be used with regular fetal heart rate and fetal growth monitoring. If prostaglandin analogs are used, premature labor symptoms and signs should be described to the patient, and the medication should be stopped if such symptoms are noted. When topical or oral carbonic anhydrase inhibitors are used, fetal growth retardation monitoring may be considered.[3]
Corticosteroids are classified as a category C medication (category C is used to describe medicines which showed side effects in animal models or where inadequate animal and human studies are available). Topical corticosteroids are nearly always used after RD surgery. All systemic glucocorticoids cross the placenta. Prednisolone and methylprednisolone cross the placenta-less than dexamethasone and may have minimal effect on the fetus.[3] Some studies have been published suggesting the absence of fetal teratogenicity with oral steroids.[5] Given the strong tendency to use topical steroids after RD surgery, and the absence of clear complications associated with these medicines, these medicines can be used in the pregnant or breastfeeding woman.[3] For all topical medications used in conjunction with RD surgery, punctal occlusion, and eyelid closure should be considered to decrease the systemic absorption of the medication. Giving the subject ambulatory vision should be seen as a priority: Silicone oil tamponade has a number of advantages over gas tamponade. Unlike gas tamponades, silicone oil is not absorbed, so the injected volume never decreases. This allows prolonged tamponade and improved tamponade of inferior retinal breaks without positioning. Patients can see through the silicone oil as it is crystal clear optically (although there is a hyperopic refractive shift). Silicone oil does not expand so air travel or return to higher elevations is permitted.[6] With gas as tamponade, vision recovery is delayed until the time gas remains in the vitreous cavity as it takes few weeks for gas to get absorbed.
Having taken all these points into consideration and after obtaining clearance from the obstretician, scleral buckling with subretinal fluid drainage was opted for over pars plana vitrectomy under LA using lignocaine with the patient in supine position. Patient B required pars plana vitrectomy to achieve anatomical success. Patient was allowed to move legs and rotate hips every 10 min. Anesthesia team ensured that patient was well hydrated before the surgery, and her vitals were maintained and monitored continuously along with noninvasive fetal monitoring. With proper monitoring, we can achieve a good visual outcome without any harm on pregnancy and fetus.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Kent-Smith BT, Wilson GA. Management of rhegmatogenous retinal detachment in a full-term pregnancy. Clin Experiment Ophthalmol 2005;33:101.
- Herbert EN, Williamson TH, Laidlaw DA. Management of rhegmatogenous retinal detachment in pregnancy. Clin Experiment Ophthalmol 2005;33:554-5.
- Glaucoma Management in Pregnancy and Post-Partum. Available from: http://www.eyewiki.aao.org. [Last updated on 2012 Feb 15; Last cited on 2011 Apr 13].
- Moore PA. Selecting drugs for the pregnant dental patient. J Am Dent Assoc 1998;129:1281-6.
- Coleman AL, Mosaed S, Kamal D. Medical therapy in pregnancy. J Glaucoma 2005;14:414-6.
- The Use of Silicone Oil in Vitrectomy Surgery. Available from: http://www.universovisual.com.br. [Last updated on 2011 Feb 10].




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.