Correlation of Platelet Indices with Clinical Profile in Elderly Patients: A Study in Rural Teaching Hospital
Citation: Agrawal A, et al. Correlation of Platelet Indices with Clinical Profile in Elderly Patients: Study in Rural Teaching Hospital. Ann Med Health Sci Res. 2018;8:163-169
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: There are evidence of age-related changes in platelet count and function, driven by changes in hematopoietic tissue, the composition of the blood and vascular health. Platelet count remains relatively stable during middle age but falls in elderly people. In this study we had tried to correlate platelet indices with the clinical profile like blood sugar, Lipid profile, blood pressure, Ischemic Heart disease and Chronic Obstructive Pulmonary Disease in elderly patients admitted in rural teaching hospital. Materials and methods: In this study, we have included 1000 patients among them 601 (60.1%) were males and 399 (39.9%) were females with the mean age of 66.02 ± 5.76 years. We studied platelet indices like plateletcrit (PCT), platelet distribution width (PDW) and mean platelet volume (MPV). Observation and results: The platelet indices (PCT, MPV and PDW) showed negative correlation with FBS and it was statistically significant (p<0.05). The platelet indices showed positive correlation with blood pressure, negative with total cholesterol, positive with HDL, negative with LDL, negative with VLDL and negative correlation with TG. The platelet indices had negative correlation with IHD and COPD and they were statistically significant (p<0.05). Conclusion: The platelet indices showed significant correlation with various clinical profiles of the elderly patients and they should be used routinely to aid in diagnosis.
Keywords
Platelet distribution width; Mean platelet volume; Platelet crit; Clinical profile; ElderlyIntroduction
Aging is associated with an increased risk of functional dependence, hospitalization, and mortality. In India, the total population of elderly was 8.2% in the year 2011, which is expected to increase over the next four decades to 19% by 2050. In January 1999, Government of India adopted ‘National Policy on Older Persons’ which defined ‘senior citizen’ or ‘elderly’ as a person who is of age 60 years or above. [1] The age-related physiological decline is intimately associated with poor quality of life, the need for long-term care and higher healthcare costs. [2] Therefore, many recent studies have investigated the usefulness of various parameters as biomarkers for adverse clinical outcomes in the elderly. [3-6] An important focus of this field is to determine whether typical parameters of automated blood cell counters demonstrate an association with adverse outcomes in the elderly. For example, total leucocytes and some subpopulations of leucocytes have been associated with frailty. [7,8] In addition, red blood cell distribution width seems to be a good indicator of morbidity/mortality in older adults. [9] Platelet indices have received an increasing amount of attention as potential markers for disease. Several epidemiological studies have reported platelet indices, in particular, the mean platelet volume (MPV), as markers for cardiovascular disease. Elevated MPV has been proposed as a risk factor for ischemic heart disease. [10] High levels of MPV seem to be associated with acute myocardial infarction and mortality following myocardial infarction, suggesting that MPV is a potentially useful prognostic biomarker in patients with cardiovascular disease. [11] The mean platelet volume (MPV), platelet distribution width (PDW), and platelet crit (PCT) values exhibited significant variability. A significant inverse relationship was observed between parasitemia and PCT. [12] Elevated Platelet size is also seen in individuals with hypertension and DM, both situations that influence the development of vascular disease. [13] Since this is such a huge health problem in the community, the risk factors of stroke categorized as non-modifiable (age/gender/race) and modifiable (hypertension, smoking, alcohol, abdominal obesity, dietary habits) and increase in fibrinogen level and hyperhomocysteinemia and increase in MPV. It is in this context that this study has its significance. Platelets play important role in pathogenesis of atherosclerotic complication, contributory factor in thrombus formation. [14]
However, the current knowledge of the usefulness of platelet indices as markers for adverse clinical outcomes in the elderly population is limited. The lack of data addressing this issue is somewhat surprising when one considers the relevant health, social, and economic implications of adverse clinical outcomes of elderly subjects and the need to identify risk factors at a stage of age-related decline that would be amenable to preventive interventions. In addition, the availability of powerful biological markers for clinical profile, hospitalization, and mortality would allow for an assessment of the efficacy of possible interventions. To address this issue, we have the plan to analyze the association of the following platelet indices with clinical profile in elderly subjects: Platelet distribution width (PDW), MPV, and platelet crit.
Material and Methods
The prospective observational study was carried out from 2015 to 2017 at Acharya Vinoba Bhave Rural Hospital attached with Datta meghe institute of medical sciences (DU) Wardha, in central india. The patients were enrolled for the study after obtaining permission from the institutional ethics committee (Reg No. - DMIMS (DU)/IEC/2015-16/1489).
Recent or current infections, malignant disease, malnutrition, pharmacological interferences (antiplatelet drugs, immunosuppressive drugs, and antineoplastic drugs) were excluded from the study.
Sample size
The sample size was calculated based on the previous study where the proportion from the previous study was 28.5% and level of significance was 5%. [15] The sample size for our study came out to be 905.66.
N=(za2/2.p (1-p))/ d2
Za2/2=level of significance at 5%=1.96
P=proportion from previous studies=28.5%=0.285
d=desired error of margin=3%=0.03
n=(1.962 × 0.285 (1-0.285))/0.052=905.66
The review was done regarding subjects medical and pharmacological history, a physical examination. The disease status of the patient is based on the explicit diagnosis in the patient’s medical history. Diseases that were considered in this study are hypertension, chronic obstructive pulmonary disease, ischemic heart disease and type II DM. Each participant’s guardian received information about the purpose and objective of the study and signed an informed consent.
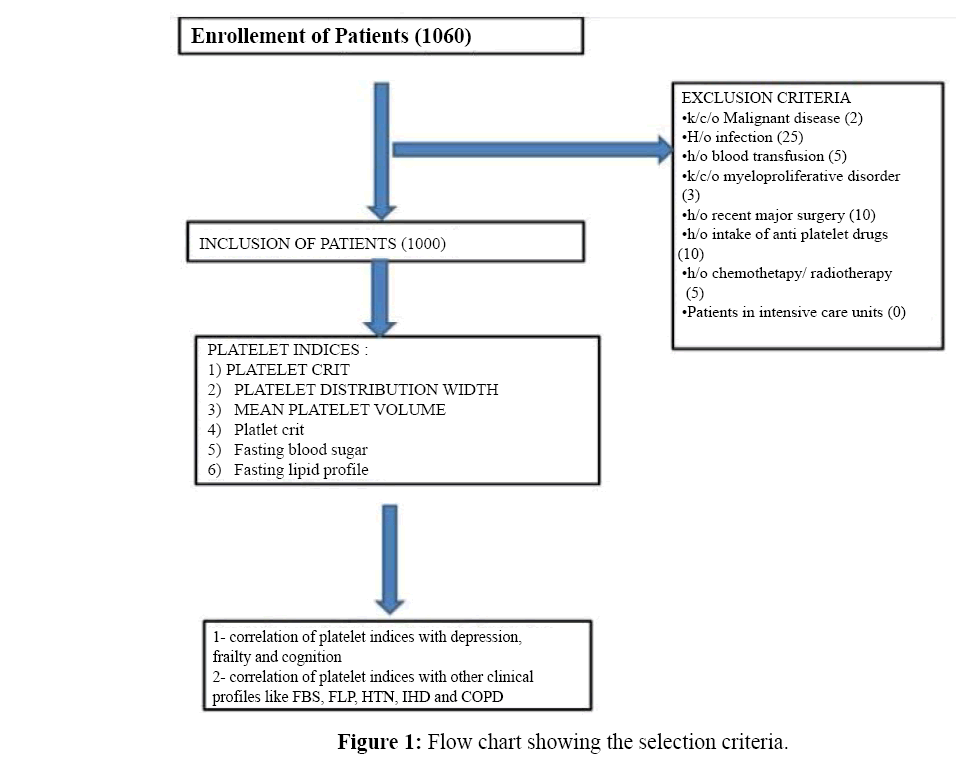
A total of 1060 patients were enrolled in the study of which 1000 patients were included, blood investigations were done and past history for the diseases considered for our study was taken. The inclusion is depicted in our flowchart [Figure 1].
Blood collection
Blood samples were obtained by venipuncture for biochemical analysis. The platelet indices were observed by the counter report from the central lab of the hospital. Following platelet indices were measured using automated hematology analyzer in the same laboratory (mean platelet volume and platelet distribution width and platelet crit).
Blood sugar measurement
The blood sugar level was measured by glucose oxidase and glucose peroxidase method. 1000 micro litre of reagent (glucose mono kit) had mixed with 10 microlitres of plasma, which was separated from the blood by centrifugation. Then half an hour after mixing readings was taken by using Robonic Semi Auto Analyzer. A fasting blood sugar sample was taken after 8 hours of overnight fasting. Sugar bulb was used for collection of the sample. The values will be expressed in gm/dl.
Fasting lipid profile measurement
Blood sample for a fasting lipid profile was collected in plane bulb after 8 hrs. Of fasting, the Randox Daytona analyzer was used to measure lipid profile (Triglyceride, High-density lipoprotein).
Lipid profile (Total cholesterol, HDL, triglycerides) was estimated by using the CODPOD method by Bayers kit. LDL was calculated using the Friedewald formula.
LDL cholesterol=(Total cholesterol – HDL cholesterol – Triglycerides/5)
The samples for fasting blood sugar and lipid profile were taken the early morning after a fasting period of 8 hours. The levels of the individual fraction of the lipid profile were interpreted in accordance with the range in central laboratory of our hospital as follows: Serum cholesterol: 120 – 200 mg/dl, HDL cholesterol: 35- 50 mg/dl, Serum triglycerides: 90 - 150 mg/dl, Serum LDL: 20 – 40 mg/dl, Serum VLDL: 90 – 165 mg/dl. The diagnosis of ischemic heart disease (IHD) will be done on the basis of history and ECG changes (New onset bundle branch block, Q waves, ST changes like T wave inversions, ST depression, and ST elevation) as per AHA guidelines. [16]
The diagnosis of COPD was done on the basis of history and changes in Chest x-ray PA view like hyperinflation of lung fields, tubular heart, flattening of diaphragm. [17]
Definitions
• Plateletcrit: It is a measure of total platelet mass (0.150 to 0.500%).
• Mean platelet volume: It is the average size of platelets (6.0 to 11.0/cu micrometer).
• Platelet distribution width: It is the variability in the size of the smallest and the largest platelets (11.0 to 18.0%).
Statistical analysis
Statistical analysis was done by using descriptive and inferential statistics using Chi-square test, Pearson’s correlation coefficient and software used in the analysis were SPSS 20.0 version, GraphPad Prism 6.0 version and p<0.05 is considered as the level of significance.
Observations and Results
In this study, we included 1000 patients of whom 601 (60.1%) were males and 399 (39.9%) were females, mean age was 66.02 ± 5.76 years. We investigated for platelet indices, fasting blood sugar, and fasting lipid profile, blood pressures, ischemic heart disease and COPD in all the patients. The mean platelet crit 0.29 ± 0.17%, mean platelet volume was 9.25 ± 5.70 per μm3, and the mean platelet distribution width 14.18 ± 5.63%. There were 165 males who were chronic smokers and 107 males who were chronic alcoholics. Mean FBS was 121.84 ± 44.29 gm/dl, the mean total cholesterol was 85.34 ± 8.81 mg/dl, the mean HDL was 30.65 ± 3.66 mg/dl, the mean LDL was 36.52 ± 5.76 mg /dl, the mean VLDL was 18.16 ± 3.2 mg/dl, the mean triglyceride level was 184.11 ± 58.10 mg/dl, mean SBP was 117.78 ± 12.79 mm Hg, the mean DBP was 67.00 ± 10.60 mm Hg. There were 206 patients who were diagnosed as IHD and 245 patients who were diagnosed with COPD. All the baseline characteristics are shown in Table 1.
| Patient (n=1000) | Values (mean) | SD |
|---|---|---|
| Age (years) | 66.02 | ± 5.76 |
| Sex: Male Female |
601 (60.1%) 399 (39.9%) |
|
| Platelet count (lac/cu mm): | 303210 | ± 21296 |
| Platelet crit (%): | 0.29 | ± 0.17 |
| Mean platelet volume (µm3) | 9.25 | ± 5.70 |
| Platelet distribution width (%): | 14.18 | ± 5.63 |
| FBS (gm/dl) | 121.84 | ± 44.29 |
| Total Cholesterol (mg/dl) | 85.34 | ± 8.81 |
| HDL (mg/dl) | 30.65 | ± 3.66 |
| LDL (mg/dl) | 36.52 | ± 5.76 |
| VLDL (mg/dl) | 18.16 | ± 3.32 |
| Triglyceride (mg/dl) | 184.11 | ± 58.10 |
| SBP (mm hg) | 117.78 | ± 12.79 |
| DBP (mm hg) | 67.00 | ± 10.60 |
Table 1: Baseline characteristics
We compared the platelet indices with fasting blood sugar. The mean value of FBS was 121.84 gm/dl. All the platelet indices (platelet crit, MPV and PDW) showed negative correlation with FBS (r=-0.109, r=-0.105 and r=-0.128) respectively and it was statistically significant (p=0.001, p=0.0001 and p=0.0001) respectively. Thus the platelet indices decreased significantly with the increasing level of FBS [Table 2].
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | -0.109 | 0.001,S |
| MPV | 9.25 | 5.70 | 1000 | -0.105 | 0.001,S |
| PDW | 14.18 | 5.63 | 1000 | -0.128 | 0.0001,S |
Table 2: Correlation of platelet indices with FBS.
In our study the platelet indices showed positive correlation with SBP (r=0.027, r=0.027 and r=0.036) respectively but it was statistically not significant (p<0.05). This correlation is shown in Table 3.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | 0.027 | 0.401,NS |
| MPV | 9.25 | 5.70 | 1000 | 0.027 | 0.396,NS |
| PDW | 14.18 | 5.63 | 1000 | 0.036 | 0.258,NS |
Table 3: Correlation of platelet indices with SBP.
The platelet indices showed positive correlation with DBP (r=0.090, r=0.059 and r=0.084) respectively, it was statistically significant for platelet indices such as (platelet crit and PDW) as p=0.004 and p=0.008 respectively but not for MPV (p=0.064). The correlation is shown in Table 4.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | 0.090 | 0.004,S |
| MPV | 9.25 | 5.70 | 1000 | 0.059 | 0.064,NS |
| PDW | 14.18 | 5.63 | 1000 | 0.084 | 0.008,S |
Table 4: Correlation of platelet indices with DBP.
All the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.007, r=-0.011 and r=-0.022 respectively) with total cholesterol and they were statistically not significant (p=0.825, p=0.717 and p=0.491 respectively). Thus the platelet indices decreased with the increasing level of TG but it was not significant. The correlation is shown in Table 5.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.179 | 1000 | -0.007 | 0.825,NS |
| MPV | 9.25 | 5.704 | 1000 | -0.011 | 0.717,NS |
| PDW | 14.18 | 5.631 | 1000 | -0.022 | 0.491,NS |
Table 5: Correlation of platelet indices with TC.
All the platelet indices had positive correlation (r=0.036, r=0.039 and r=0.035 respectively) with HDL and they were statistically not significant (p=0.251, p=.216 and p=0.265 respectively), the platelet indices increased with the increasing HDL but it was not significant. The correlation is shown in Table 6.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.179 | 1000 | 0.036 | 0.251,NS |
| MPV | 9.25 | 5.704 | 1000 | 0.039 | 0.216,NS |
| PDW | 14.18 | 5.631 | 1000 | 0.035 | 0.265,NS |
Table 6: Correlation of platelet indices with HDL.
All the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.026, r=-0.028 and r=-0.041 respectively) with LDL and they were statistically not significant (p=0.408, p=.373 and p=0.193 respectively). The platelet indices decreased with the increasing LDL but it was not significant. The correlation is shown in Table 7.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.179 | 1000 | -0.026 | 0.408,NS |
| MPV | 9.25 | 5.704 | 1000 | -0.028 | 0.373,NS |
| PDW | 14.18 | 5.631 | 1000 | -0.041 | 0.193,NS |
Table 7: Correlation of platelet indices with LDL.
All the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.013, r=-0.025 and r=-0.025 respectively) with VLDL and they were statistically not significant (p=0.678, p=.434 and p=0.423 respectively). The platelet indices decreased with the increasing VLDL but it was not significant. The correlation is shown in Table 8.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | -0.013 | 0.678,NS |
| MPV | 9.25 | 5.70 | 1000 | -0.025 | 0.434,NS |
| PDW | 14.18 | 5.63 | 1000 | -0.025 | 0.423,NS |
Table 8: Correlation of platelet indices with VLDL.
In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=--0.115, r=-0.109 and r=-0.140 respectively) with TG and they were statistically significant (p=0.0001, p=0.001 and p=0.0001 respectively). Thus the platelet indices decreased significantly with the increasing level of TG. The correlation is shown in Table 9.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘r’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | -0.115 | 0.0001,S |
| MPV | 9.25 | 5.70 | 1000 | -0.109 | 0.001,S |
| PDW | 14.18 | 5.63 | 1000 | -0.140 | 0.0001,S |
Table 9: Correlation of platelet indices with TG.
In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.725, r=-0.766 and r=- 0.731 respectively) with IHD and they were statistically significant (p=0.0001, p=.0001 and p=0.0001 respectively). The mean value of Platelet indices were significantly higher for the patients with IHD than that of the patients without IHD (p<0.001). The correlation is shown in Table 10.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘ρ’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | -0.725 | 0.0001,S |
| MPV | 9.25 | 5.70 | 1000 | -0.766 | 0.0001,S |
| PDW | 14.18 | 5.63 | 1000 | -0.731 | 0.0001,S |
Table 10: Correlation of platelet indices with IHD.
In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.796, r=-0.805 and r=- 0.785 respectively) with COPD and they were statistically significant (p=0.0001, p=.0001 and p=0.0001 respectively). All the mean value of the parameters related to Platelet indices were significantly higher for the patients with COPD than that of the patients without COPD (p<0.001). The correlation is shown in Table 11.
| Platelet indices | Mean | Std. Deviation | N | Correlation ‘ρ’ | p-value |
|---|---|---|---|---|---|
| Platelet Crit | 0.29 | 0.17 | 1000 | -0.796 | 0.0001,S |
| MPV | 9.25 | 5.70 | 1000 | -0.805 | 0.0001,S |
| PDW | 14.18 | 5.63 | 1000 | -0.785 | 0.0001,S |
Table 11: Correlation of platelet indices with COPD.
Discussion
In our study, there was an association of the Platelet indices like platelet distribution width (PDW), MPV, and platelet crit with clinical profile in elderly subjects.
We compared the platelet indices with fasting blood sugar. The mean value of FBS was 121.84 gm/dl. All the platelet indices (platelet crit, MPV and PDW) showed negative correlation with FBS. (r=-0.109, r=-0.105 and r=-0.128) respectively and it was statistically significant (p=0.001, p=0.0001 and p=0.0001) respectively. In a study by Zuberi B F et al. [18] the difference of MPV among the non-DM and DM groups was significant with p-value of 0.0001 and 95% CI of -1.03 and -0.38. The difference between the non-DM and IFG group was significant with p-value of 0.03 and 95% CI of -0.67 and -0.02. The difference in MPV was significant between IFG and DM groups with p-value of 0.26 and 95% CI of -0.68 and -0.03. In a study by Farah Jabeen et al. [19] the positive association between glycemic control determinant (FBG and HbAIc) and platelet indices indicate the clinical usefulness of HbA1c level and platelet indices hence surrogate markers in early detection of diabetic complications. Masanori Shimodaira et al. [20] showed MPV of the pre-diabetic group was higher than in other groups. MPV was independently and positively associated with FPG, in pre-diabetic subjects and also in normal FPG subjects (β=0.020 and β=0.006, respectively).
In our study the platelet indices (platelet crit, MPV and PDW) showed positive correlation with SBP (r=0.027, r=0.027 and r=0.036) respectively but it was statistically not significant (p<0.05). In a study by Xia Cao et al. [21] it showed that MPV is associated with prehypertension. After controlling for the main potential confounders (age, sex, and BMI), and for other potentially relevant variables (smoking and serum cholesterol), high levels of MPV were associated with greater odds of pre hypertension.
In our study the platelet indices (platelet crit, MPV and PDW) showed positive correlation with DBP (r=0.090, r=0.059 and r=0.084) respectively, it was statistically significant for all platelet indices (platelet crit and PDW) as p=0.004 and p=0.008 respectively but not for MPV (p=0.064).
In a study Kun Yang, et al. [22] MPV was negatively associated with DBP in male, PDW had a negative association with SBP. PLT was associated with male’s DBP.
All the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.007, r=-0.011 and r=-0.022 respectively) with total cholesterol and they were statistically not significant (p=0.632, p=0.825, p=.717 and p=0.491 respectively).
Contrasting results were found in a study Y.-L. Chang et al. [23] in which patients with higher platelet count had higher TC values (210 ± 40 mg/dl) while patients with lower platelet count showed lower TC values (193.9 ± 37.5 mg /dl). The study had no data for other platelet indices that we have examined like PCT, PDW, and MPV.
In our study all the platelet indices (platelet crit, MPV and PDW) had positive correlation (r=0.036, r=0.039 and r=0.035 respectively) with HDL and they were statistically not significant (p=0.251, p=.216 and p=0.265 respectively). Contrasting results were found in a study Y.-L. Chang et al. [23] which showed patients with higher platelet count had higher HDL values (46.6 ± 015.3 mg/dl) and patients with lower platelet count showed lower HDL values (45.4 ± 12.8 mg /dl).
In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.026, r=-0.028 and r=-0.041 respectively) with LDL and they were statistically not significant (p=0.408, p=.373 and p=0.193 respectively). Contrasting results were found in a study Y.-L. Chang et al. [23] which revealed patients with higher platelet count had higher LDL values (137.8 ± 35.7 mg/dl) and patients with lower platelet count showed lower LDL values (127 ± 33.2 mg /dl). In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.013, r=-0.025 and r=-0.025 respectively) with VLDL and they were statistically not significant (p=0.678, p=.434 and p=0.423 respectively). In our study, however, there was a negative correlation of VLDL with platelet indices and it was statistically not significant (p>0.05). In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=--0.115, r=-0.109 and r=-0.140 respectively) with TG and they were statistically significant (p=0.0001, p=0.001 and p=0.0001 respectively).
In our study all the platelet indices (platelet crit, MPV and PDW) had negative correlation (r=-0.725, r=-0.766 and r=-0.731 respectively) with IHD and they were statistically significant (p=0.0001, p=.0001 and p=0.0001 respectively).
In a study by Sravan K Reddy et al. [24] which showed significantly higher MPV in patients with STEMI (10.2 ± 2.8) as compared to controls (8.5 ± 6.9). PDW was also significantly higher in cases compared to controls (p<0.05). This difference could be due to the patient’s age group which was above 60 years in our study and also as in Sravan K Reddy et al. the enrolled patients were on an antiplatelet drug which could have altered the platelet indices whereas in our study we had excluded those individuals who were on antiplatelet drugs. Lippi G et al. [25] showed analysis of MPV values in 2304 adult patients admitted for provisional diagnosis of Acute Coronary Syndrome. They found all those patients, having cardiac troponin T levels of 0.03 ng/mL or greater and ischemic electrocardiographic changes, had higher MPV values than non-ACS patients who had normal cardiac troponin T levels.
In our study all the platelet indices (plateletcrit, MPV and PDW) had negative correlation (r=-0.796, r=-0.805 and r=-0.785 respectively) with COPD and they were statistically significant (p=0.0001, p=0.0001 and p=0.0001 respectively). In a study by Sevinc S. Ulasli et al. [26] they included 47 patients with COPD and showed MPV values were 9.3 ± 1.4 and 8.6 ± 1.0 fl during stable period and during acute exacerbation, respectively. The MPV values were significantly lower in patients during acute exacerbation than in those during the stable period of COPD and in control subjects (both, P<0.001). The results suggest that assessment of MPV in COPD exacerbation may indicate systemic inflammation. The results were similar to that in our study. In a study by Makhlouf et al. [27] different result was seen compared to our study. Mean Platelet volume (MPV), Platelet distribution width (PDW), Platelet crit (PCT) were significantly higher in COPD patients. There was no significant difference in the various laboratory data among different stages of COPD (P >0.05). In COPD patients, MPV was a significantly positively correlated with CRP and PDW (r=0.346, P<0.001; r=0.510, P<0.001 respectively) and negatively correlated with the platelet count (r=-0.294, P=0.002).
Some diets and nutrients have been shown to affect platelet function. Dark chocolate, foods with low glycemic index, garlic, ginger, omega-3 PUFA, onion, purple grape juice, tomato, and wine reduce platelet aggregation. Dark chocolate also reduces P-selectin expression, PAC-1 binding, and platelet microparticle formation. Berries inhibit platelet function (PFA-100 assay). Energy drinks have been shown to increase platelet aggregation and caffeine increases platelet microparticle formation. [28] Plant foods can provide α-linolenic acid but are devoid of the long-chain omega-3 fatty acids—eicosapentenoic acid and docosahexenoic acid. A significant rise in platelet linoleic acid concentration and a decline in platelet arachidonic acid (AA) concentration were observed in vegetarians. We could not found any article correlating diets and platelet indices. [28]
Conclusion
Among the clinical parameter, patients with higher FBS had decreased platelet crit, PDW, and MPV. Also patients with higher platelet indices had higher systolic and diastolic blood pressure. Patients with fasting lipid profile when compared with platelet indices showed no significant correlation except for triglyceride levels. All the platelet indices showed significant correlation with IHD and COPD, which were lower in patients with the respective diseases.
Conflict of Interest
I declare there is no conflict of interest
REFERENCES
- Kumar S. Frailty index - Assessment Tools in elderly: Feasibility in India. Annals of Geriatric Education and Medical Sciences 2017;4:45-49
- Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92-100.
- De Gonzalo-Calvo D, De Luxán-Delgado B, Rodríguez-González S, García-Macia M, Suárez FM, Solano JJ, et al. Interleukin 6, soluble tumor necrosis factor receptor I and red blood cell distribution width as biological markers of functional dependence in an elderly population: A translational approach. Cytokine. 2012;58:193-198.
- Stenholm S, Maggio M, Lauretani F, Bandinelli S, Ceda GP, Di Iorio A, et al. Anabolic and Catabolic Biomarkers As Predictors of Muscle Strength Decline: The In: CHIANTI Study. Rejuvenation Res. 2010;13:3-11.
- Caballero B, Rubio-González A, Potes Y, Martínez-Reig M, Sánchez-Jurado PM, Romero L, et al. Associations of the antioxidant capacity and hemoglobin levels with functional physical performance of the upper and lower body limbs. AGE. 2014;36:851-867.
- De Martinis M, Franceschi C, Monti D, Ginaldi L. Inflammation markers predicting frailty and mortality in the elderly. Exp Mol Pathol. 2006;80:219-227.
- Nishijima TF, Deal AM, Williams GR, Guerard EJ, Nyrop KA, Muss HB. Frailty and inflammatory markers in older adults with cancer. Aging (Albany NY). 2017;9:650-661.
- Leng SX, Hung W, Cappola AR, Yu Q, Xue Q-L, Fried LP. White blood cell counts, insulin like growth factor-1 levels, and frailty in community-dwelling older women. J Gerontol A Biol Sci Med Sci. 2009;64A:499-502.
- Patel KV, Semba RD, Ferrucci L, Newman AB, Fried LP, Wallace RB, et al. Red cell distribution width and mortality in older adults: A meta-analysis. J Gerontol A Biol Sci Med Sci. 2010;65A:258-265.
- Endler G, Klimesch A, Sunder-Plassmann H, Schillinger M, Exner M, Mannhalter C, et al. Mean platelet volume is an independent risk factor for myocardial infarction but not for coronary artery disease. Br J Haematol. 2002;117:399-404.
- Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, Konkle B, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:148-156.
- Leal-Santos FA, Silva SB, Crepaldi NP, Nery AF, Martin TO, Alves-Junior ER, et al. Altered platelet indices as potential markers of severe and complicated malaria caused by Plasmodium vivax: a cross-sectional descriptive study. Malar J. 2013;12:462.
- Pathansali R, Smith NM, Bath PMW. Prothrombotic megakaryocyte and platelet changes in hypertension are reversed following treatment: a pilot study. Platelets. 2001;12:144-149.
- Greisenegger S, Endler G, Hsieh K, Tentschert S, Mannhalter C, Lalouschek W. Is elevated mean platelet volume associated with a worse outcome in patients with acute ischemic cerebrovascular events? Stroke. 2004;35:1688-1691.
- Shah AR, Chaudhari SN, Shah MH. Role of platelet parameters in diagnosing various clinical conditions. National Journal Of Medical Research 2013;3:162-165.
- Wagner GS, Macfarlane P, Wellens H, Josephson M, Gorgels A, Mirvis DM, et al. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part VI: Acute Ischemia/Infarction: A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: Endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119:e262-e270.
- Wallace GMF, Winter JH, Winter JE, Taylor A, Taylor TW, Cameron RC. Chest X-rays in COPD screening: Are they worthwhile? Respir Med. 2009;103:1862-1865.
- Zuberi BF, Akhtar N, Afsar S. Comparison of mean platelet volume in patients with diabetes mellitus, impaired fasting glucose and non-diabetic subjects. Singapore Med J. 2008;49:114-116.
- Jabeen F, Fawwad A, Rizvi HA, Alvi F. Role of platelet indices, glycemic control and hs-CRP in pathogenesis of vascular complications in type-2 diabetic patients. Pakistan Journal of Medical Sciences. 2013;29:152-156.
- Shimodaira M, Niwa T, Nakajima K, Kobayashi M, Hanyu N, Nakayama T. Correlation between mean platelet volume and fasting plasma glucose levels in prediabetic and normoglycemic individuals. Cardiovasc Diabetol. 2013;12:14.
- Cao X, Xie X, Zhou J, Yang P, Wang Y, Chen Z. Increased platelet volume in a general population with prehypertension: a cross-sectional study of 80 545 participants from China. Hypertens Res. 2012;35:903-908.
- Yang K, Tao L, Mahara G, Yan Y, Cao K, Liu X, et al. An association of platelet indices with blood pressure in Beijing adults: Applying quadratic inference function for a longitudinal study. Medicine (Baltimore). 2016;95:e4964.
- Chang YL, Pei C, Pei D, Tang SH, Hsu CH, Chen YL, et al. Association Between Platelet Count and Components of Metabolic Syndrome in Geriatric Taiwanese Males. Int J Gerontol. 2012;6:215-219.
- Reddy SK, Shetty R, Marupuru S, Yedavalli N, Shetty K. Significance of platelet volume indices in STEMI patients: A case-control study. Journal of Clinical and Diagnostic Research : JCDR. 2017;11:LC05-LC07.
- Lippi G, Filippozzi L, Salvagno GL, Montagnana M, Franchini M, Guidi GC, et al. Increased mean platelet volume in patients with acute coronary syndromes. Arch Pathol Lab Med. 2009;133:1441-1443.
- Ulasli SS, Ozyurek BA, Yilmaz EB, Ulubay G. Mean platelet volume as an inflammatory marker in acute exacerbation of chronic obstructive pulmonary disease. Pol Arch Med Wewn. 2012;122:284-290.
- Makhlouf HA, Sadek SH, Nafady AA. Platelet function in diabetic and non-diabetic patients with chronic obstructive pulmonary disease: a case control study. The Clinical Respiratory Journal 2018;12:48-56.
- McEwen BJ. The influence of diet and nutrients on platelet function. Semin Thromb Hemost 2014;40:214-226.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.