Custom Made Pressure Appliance for Presurgical Sustained Compression of Auricular Keloid
- *Corresponding Author:
- Dr. Manu Rathee
Department of Prosthodontics, Post Graduate Institute of Dental Sciences, Pt. B.D. Sharma University of Health Sciences, Rohtak, Haryana, India.
E-mail: ratheemanu@gmail.com
Abstract
Keloid is dermal lesion characterized by nodular fibroblastic proliferation, which is considered an aberration of wound healing process. It is believed to be the confused scar that does not know when to stop growing. Pressure therapy using clips or splints is widely used for the treatment of keloids; however, it is often very difficult to control the amount and direction of pressure applied. Among the most common complications of this therapy is ulceration due to excessive pressure. A case of presurgical size reduction for a large ear keloid with a custom made pressure appliance is presented. This novel design of the appliance allows for better control over the amount and direction of the pressure applied on the scar tissue.
Keywords
Auricle, Hypertrophic scar, Keloid, Pressure therapy
Introduction
Keloid formation has been recognized for several 100 years. It was known as “cancroide” until a change of nomenclature was proposed by the French Dermatologist Jean Louis Alibert, who in 1814 suggested the word “cheloide,” or keloid.[1] It is a hypertrophic, cutaneous scar that may develop as a result of burns, surgical incisions, wounds, vaccinations, or other stimuli. Keloids usually occur in the young patients and some races are predisposed to their development.[2,3]
Many treatment modalities have been used for keloids. In the past, low-dose radiation was commonly used either alone or after surgical excision of the keloid.[4] Local injection of steroids has also been used with good results. A successful, conservative and innocuous form of treatment have been achieved by applying uniform and adjustable compression for prolonged periods before and after surgical removal of a keloid.[5] Devices capable of applying the necessary pressure have been developed in the form of clips, buttons, and earrings. Pressure therapy alone or in combination with surgery has shown beneficial results in the treatment of auricular keloids. It has been successful in resolving the keloid completely in smaller lesions or to a great extent in the larger lesions. In view of these effects of pressure therapy, a conservative treatment attempt was planned to reduce the size of lesion and to reduce the surgical burden. This article describes the fabrication of an inexpensive, custom made methyl methacrylate pressure appliance for presurgical sustained compression of a large ear keloid.
Case Report
Clinical case
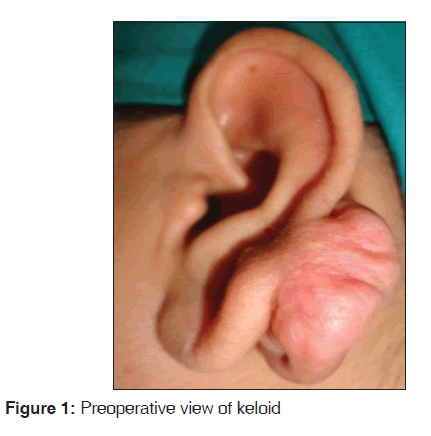
A 42-year-old female patient was referred from the Department of Plastic Surgery for the fabrication of ear pressure clip for the left auricular keloid. She complained of swelling on the left ear lobe since 2 years. There was a history of first ear piercing of the lobe of the ear at the age of 12 years without any swelling following piercing. Additional ear piercing was done at age of 38 years, which was 1 cm above the previous site. A very small swelling appeared on the posterior aspect of the pinna of the left ear after 1½ month at the second ear piercing site, which gradually increased in size. The lesion was excised surgically after 1 year. The swelling recurred after 1½ month of the surgery and increased progressively to a size larger than the previous one. Later, surgical excision was done after 1½ year again. Swelling recurred third time at the same site after 1 month of the second surgery and continued to grow until it reached the present size in 1½ year duration [Figure 1].
On examination, a firm, nontender, nonpedunculated, lobulated swelling with a smooth surface and irregular margins, measuring 37 mm superoinferiorly and 35 mm anteroposteriorly was present at the posterior aspect of the pinna of the left ear. There were no accompanying symptoms except it caused severe emotional stress due to impaired esthetics. A clinical diagnosis of keloid was given. A custom made methyl methacrylate pressure appliance was planned to reduce the presurgical size of the keloid.
Procedure followed for fabrication of appliance
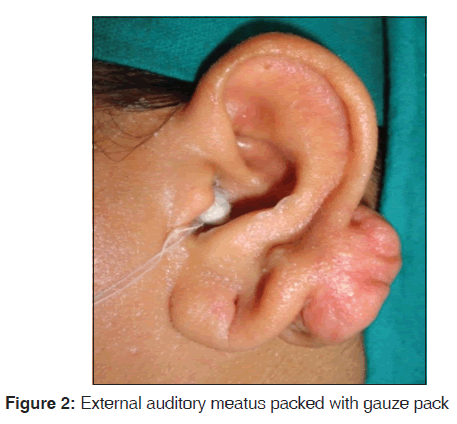
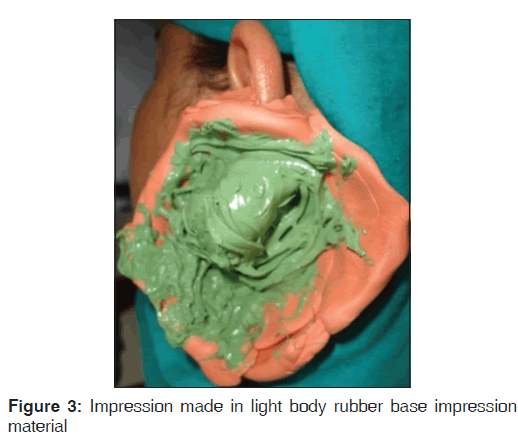
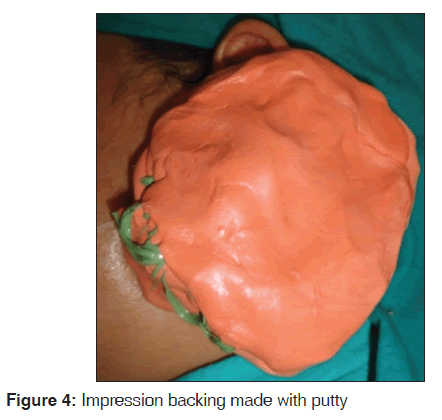
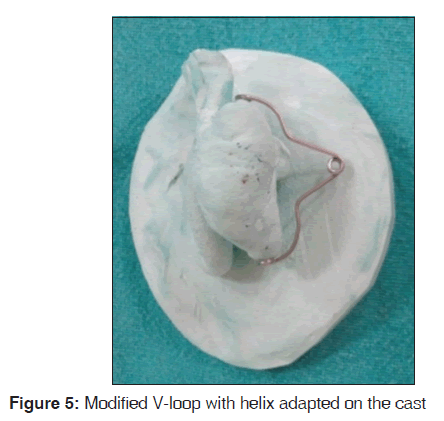
Patient’s skin over the ear and keloid was lubricated with petroleum jelly, and external auditory meatus was blocked with gauze pack tied with a thread [Figure 2]. Putty rubber base impression material was used to make beading for the confinement of the impression material. Impression was made using light body vinyl polysiloxane impression material (3M ESPE Express, VPS Impression Material, USA) with backing of putty addition silicone impression material [Figures 3 and 4]. Completed impression was retrieved after the impression materials were set. The impression was poured in dental stone (Kalstone, Kalabhai Karson Pvt. Ltd., Mumbai, India) with adequate land area to make the diagnostic cast. A modified configuration of the spring was planned using 21gauge stainless steel wire that was used to make a V-shaped loop with a helix at its apex and adapted over the swelling on the cast [Figure 5]. A custom made pressure appliance was fabricated incorporating this loop in clear methyl methacrylate and characterization was done to match the color of the appliance with that of the adjoining skin to make the appliance more esthetically acceptable and unnoticeable to others. Care was taken to ensure adequate space for acrylic resin between the wire loop and the skin to avoid direct contact of stainless steel wire with the skin and a wax spacer was used to provide this adequate space. The design of the appliance involved covering the whole of the surface of the swelling with the gap between the two almost equal halves to permit activation to ensure sustained pressure. With this design, there is no need for fabrication of a new appliance after reduction in size of the keloid as the gap between the two halves permits adjustment by closing the helix.
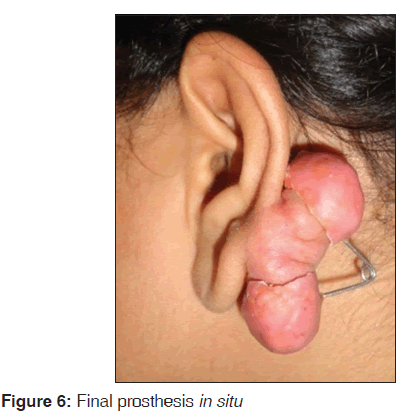
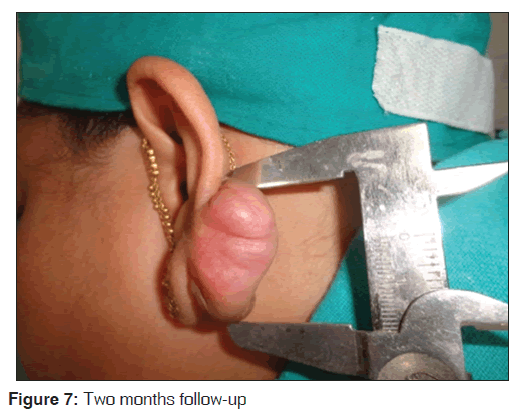
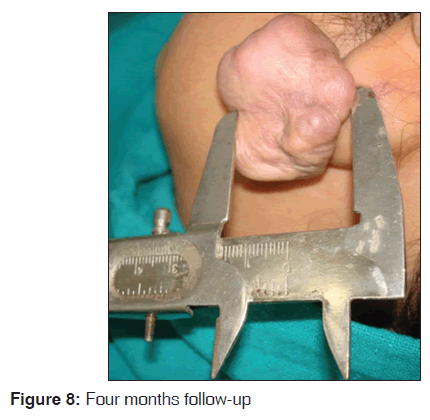
The appliance was finished, polished and adjusted to remove any sore spots [Figure 6]. It was delivered, and the patient was instructed to wear it 24 h a day 7 days a week. She was also instructed about use, maintenance of hygiene and regular follow-up for periodic activation of the appliance. During follow-up, a 2 mm reduction in all over size (Superioinferiorly and anteroposteriorly) of the keloid was achieved after 2 months [Figure 7] and more 2 mm reduction in superior-inferior dimension at 4 months follow-up [Figure 8]. The adjustment was done in prosthesis by gradual addition of acrylic encompassing the mass without relief. No complication was observed during treatment.
Discussion
Keloid is benign, persistent fibroproliferative mass of dermal connective tissue that develops at the site of cutaneous injury due to uncontrolled repair and healing process at distinctive anatomical locations with a predilection for highly pigmented ethenic group.[6,7] Though the pathophysiology of keloid formation remains obscure, and no single hypothesis explains its formation adequately, but it is generally believed that dysregulation during cutaneous healing results in excessive scarring where keloid and a hypertrophic scar present the opposite ends of a spectrum of wound healing behavior.[8,9]
Evidence indicate that there is prolonged inflammatory phase with immune cell infiltrate in the scar tissue of dermal injury resulting in exaggerated fibroblastic activity with an abundance of sustained extracellular matrix.[8] It is also believed that “tension free suture line” is the culprit for recurrence.[10]
Certain types of injuries show increased keloid incidence and burns carry the highest risk. Furthermore, highly pigmented ethnic groups show 15 times more prevalence than whites although no genetic loci have been identified for conferring risk of keloid formation.[11] Distinct anatomical site involvement is seen, often on chest, shoulders, upper back, back of the neck and more on ear lobes with specifically posterior aspect of ear lobes and rare on palms and soles. Keloid formation is common after small skin incisions and other procedures, including draining of auricular hematomas, repair of auricular trauma or secondary keloid formation after prior keloid excision. Surgical monotherapy results in high-incidence of recurrence (50-100%).[12]
Body piercing, acne, chicken pox, biopsy procedures, lacerations, vaccination especially Bacillus Calmette-Guerin have been found to be the risk factors for keloid formation. There is evidence in the literature supporting the fact that the risk of keloid is increased after 10 years of age, with each subsequent piercing and after each surgical excision. Hence, it is advised in the interest of the population to be educated against body piercing. Similarly, the chances of keloid formation are high in surgery. Clinically, the age of onset of keloid disorder has been observed between of 10 and 30 years. However, bilateral auricular keloid has been reported in a female patient at the age of 9 months.[13]
Various modalities have been used for the treatment of keloid including surgical excision, mechanical compression, intralesional steroid injection, cryotherapy, Laser, radiotherapy, silicone gel sheeting and topical anti-metabolites, though treatment remains short of ideal. Topical vitamin E and onion extract topical gel have been used for prevention. A combination of treatment modalities is used more commonly to avoid recurrence and to provide more conservative treatment.
Friedman proposed surgical excision and corticosteroids for small keloids, pressure therapy and a combination of surgery and steroid for moderately large scars and a combination of surgery and postoperative radiotherapy for very large, resistant scars.[14]
Surgical monotherapy of keloid is temporarily gratifying as it is almost invariably followed by even more aggressive regrowth of scar.[15] Thus, core excision and primary closure with minimal tension wound closure is preferred surgical treatment of the earlobe keloid. Intrascar excision with debulking procedure can esthetically remove the scars in a shorter duration without affecting the adjoining anatomic structures. Intralesional marginal surgical excision is recommended because total excision stimulates additional collagen synthesis promoting quick recurrence, even larger than previous one. Hence, the surgical therapy directs the intrascar incision in view of these facts. The same pattern of growth has been observed in the present case.
Pressure therapy with clips, buttons, earrings or form-pressure garments is an integral part of pinna keloid treatment though biomechanics by which pressure alters the collagen metabolism is unclear. This therapy is widely used, but it is difficult to provide sufficient, direct and continuous pressure with controlled amount and direction of pressure. Compression therapy with various devices or dressings that apply pressure exceeding the capillary pressure create a hypoxic microenvironment that results in fibroblast degradation and thence collagen degradation. The pressure exerted should be at least 24 mmHg that is, above the inherent capillary pressure, but this must not exceed 30 mm Hg, as it will cause tissue necrosis due to diminish peripheral blood circulation.[16,17]
It is evident that the curvy anatomy of the helical rim with its concave anterior and convex posterior surface is not easily pliable. The optimal alignment of the compression device and provision for adequate sustained pressure are significant due to the complex anatomy of the auricle. The custom made pressure appliance successfully delivers pressure on the tortuous helical rim. Ear pressure prostheses are used for maintaining pressure before and after surgical removal. The presurgical compression reduces the size of lesion prior to surgery while postsurgical compression prevents postsurgical recurrence of the ear keloid.
The design presented in this article includes incorporation of the V-loop component to the ear pressure appliance, which permits the adjustment in the amount and direction of pressure, unlike the conventional ear clips that do not have this adjustability. This design ensures adequate springiness and range while maintaining acceptable strength. The ear clips may cause excessive pressure and frequent bleeding with the increased possibility of infection or necrosis of the soft tissues. The conventional design may result in an inadequate pressure also. The presented design reduces the possible complications encountered due to excessive pressure ulceration, and this also eliminates the need to make new clips as the keloid scar reduces in size permitting sustained controlled pressure by closing the helix. This pressure appliance is comfortable, light weight, inexpensive, esthetic, easy to use, and clean. For a successful treatment outcome with compression therapy, the patient must be well-motivated as the duration of to use the appliance is long and need regular follow-ups.[18,19]
Conclusion
The pressure therapy is an adjunct for the early maturation of scar tissue and the prevention of recurrence of keloid with other therapies. Presurgical reduction in the size of the large keloid scar was achieved with the simple, custom fabricated pressure appliance in a short duration. It is advisable that patients should be educated to avoid body piercing and elective cosmetic procedures. Histopathology should be used as a prophylactic measure to avoid missing potentially malignant condition. The patients should be counseled about recurrence, palpable postoperative nodules and need for close monitoring. Overnight usage of the pressure device seems to be a safe and effective extension of established auricular keloid therapy with the potential for prophylaxis of recurrence. It generally takes 6-12 months of therapy to achieve best results, but the most patient compliance fades after several months. Hence, regular clinical follow-up to screen for the early recurring lesion is mandatory.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Slavkin HC. The body’s skin frontier and the challenges of wound healing: Keloids. J Am Dent Assoc 2000;131:362-5.
- Chalian VA, Bennett JE, Sayoc AM, Ghalichebaf M. Auricular compression stent. J Prosthet Dent 1985;54:560-3.
- Hurtado AJ, Crowther DS. Methyl methacrylate stent for prevention of postexcisional recurrent ear keloid. J Prosthet Dent 1985;54:245-50.
- Sela M, Taicher S. Prosthetic treatment of earlobe keloids. J Prosthet Dent 1984;52:417-8.
- Yüzbaşıoğlu E. Reverse activated hyrax pressure appliance for treatment of a keloid located at auricula helix. J Prosthodont 2013;22:509-12.
- Robles DT, Berg D. Abnormal wound healing: Keloids. Clin Dermatol 2007;25:26-32.
- Stucker FJ, Shaw GY. An approach to management of keloids. Arch Otolaryngol Head Neck Surg 1992;118:63-7.
- Butler PD, Longaker MT, Yang GP. Current progress in keloid research and treatment. J Am Coll Surg 2008;206:731-41.
- Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG. Hypertrophic scarring and keloids: Pathomechanisms and current and emerging treatment strategies. Mol Med 2011;17:113-25.
- Narakula GK, Shenoy RK. A prospective clinical review of “multi model” approach for treating ear keloids. Indian J Plast Surg 2008;41:2-7.
- Hunasgi S, Koneru A, Vanishree M, Shamala R. Keloid: A case report and review of pathophysiology and differences between keloid and hypertrophic scars. J Oral Maxillofac Pathol 2013;17:116-20.
- Al-Attar A, Mess S, Thomassen JM, Kauffman CL, Davison SP. Keloid pathogenesis and treatment. Plast Reconstr Surg 2006;117:286-300.
- Tirgan MH, Shutty CM, Park TH. Nine-month-old patient with bilateral earlobe keloids. Pediatrics 2013;131:e313-7.
- Friedman RM. Abnormal scars. Sel Read Plast Surg 1995;8:20-7.
- Rockwell WB, Cohen IK, Ehrlich HP. Keloids and hypertrophic scars: A comprehensive review. Plast Reconstr Surg 1989;84:827-37.
- Niessen FB, Spauwen PH, Schalkwijk J, Kon M. On the nature of hypertrophic scars and keloids: A review. Plast Reconstr Surg 1999;104:1435-58.
- Chrisostomidis C, Konofaos P, Chrisostomidis G, Vasilopoulou A, Dimitroulis D, Frangoulis M, et al. Management of external ear keloids using form-pressure therapy. Clin Exp Dermatol 2008;33:273-5.
- Kadouch DJ, van der Veer WM, Kerkdijk D, Mahdavian Delavary B, Niessen FB. Postoperative pressure therapy of ear keloids using a custom-made methyl methacrylate stent. Dermatol Surg 2010;36:383-5.
- Savion Y, Sela M. Prefabricated pressure earring for earlobe keloids. J Prosthet Dent 2008;99:406-7.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.