Developing and Organizing a Trauma System and Mass Casualty Management: Some Useful Observations from the Israeli Trauma Model
- *Corresponding Author:
- Dr. Bhaskar Borgohain,
Department of Orthopaedics, North-Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India
E-mail: bhaskarborg@gmail.com
Abstract
A trauma system is a chain of arrangements and preparedness to provide quality response to injured from the site of injury to the appropriate hospital for the full range of care. Israel has a unique trauma system developed from the experience gained in peace and in war. The system is designed to fit the state’s current health system, which is different from the European and American systems. An effective trauma system may potentially manage mass casualty incidence better. The aim of this paper is to discuss learning points to develop a trauma system based on the Israeli trauma model. After participating in a course on developing a trauma system organized by a top Israeli trauma center, a literature search on the topic on the Internet was done using relevant key words like trauma system and disaster management in Israel using the Google search engine in the pubmed, open access journals and websites of trauma organizations. Israel has a unique trauma system of organizing and managing an emergency event, characterized by a central national organization responsible for management, coordination and ongoing quality control. Because of its unique geopolitical situation, the armed forces has a significant role in the system. Investing adequate resources on continuous education, manpower training, motivation, team‑work and creation of public volunteers through advocacy is important for capacity building to develop a trauma system. Wisdom, motivation and pragmatism of the Israeli model may be useful to streamline work in skeletal trauma services of developing countries having fewer resources to bring consistency and acceptable standards in trauma care.
Keywords
Disaster preparedness, Israeli trauma model, Mass casualty incidents, Trauma center, Trauma system
Introduction
The primary objective of a trauma system is to diminish or eliminate the risk of death or permanent disability following traumatic events. Unfortunately, in many developing countries, a trauma system is non-existent or, at best, skeletal. It is therefore essential to create awareness in the society about the trauma system. Medical lessons learned from Vietnam and previous military conflicts led to the development of civilian trauma systems in the United States.[1] The true value of a trauma system is derived from the seamless transition between each phase of care, integrating existing resources to achieve improved patient outcomes. Success of a trauma system is largely determined by the degree to which it is supported by public policy.[2]
During most of its 50 years of existence, the State of Israel has been surrounded by proclaimed enemies, fought numerous wars for survival and has been threatened by terrorist attacks. Rambam hospital in Israel was exposed to an unprecedented experience during the Second Lebanon War in 2006, and, for more than 1 month, it was subjected to continuous rocket attacks, but it continued to provide emergency and routine medical services to the civilian population and also served the military personnel evacuated from the battlefront.[3] The function and quality of response of the hospital team during the war was smooth due to its preparedness for disasters and wartime conditions. Rambam’s Level I trauma center has an expertise, multidisciplinary team for peace-time medical practice with time-tested capabilities for war time contingencies, making it an ideal center for learning trauma and disaster management for health care professionals from other countries.[4] The Israeli government created and reinforced a strategy for dealing with a mass casualty incidence (MCI) on the national level as well as on the individual hospital level.[5,6] To create and implement these strategies, its Ministry of Health created the Board of Supreme Hospitalization Authority (SHA), whose main objective was to organize the national health system during a period of strife.[5,6] Because of its unique geopolitical situation, the armed forces has a significant role in the Israeli trauma model.
Materials and Methods
The first author had participated in a 2-week-long course on developing and organizing a trauma system and MCI management organized by Rambam Medical Centre, Haifa, Israel, which is a regular course offered by the hospital from time to time. It is the largest level-I trauma center in northern Israel. There were frontal lectures, video presentations, interactive question-answer sessions, table top drills and trauma workshops. There was also a special session on artistic reproduction/simulation of trauma victim for using them to simulate realistic drills. The main objectives of this course was:[4] (1) To understand the continuity of care of trauma patients in a trauma system, (2) to study the structures involved in the various phases of treatment of trauma, (3) to develop a model of a trauma system appropriate for the trainee’s country of origin and (4) understand Mass Casualty Scenario (MCS): Preparedness and response. The teaching programme also included guidelines and protocols for an MCS; both conventional as well as unconventional (chemical, radiological, biological) events. After the training, the authors have done literature search on the topic on the Internet using key words like trauma system Israel and disaster management Israel in the Pub med, Google search engine, open access journals and official websites of Israel trauma coalition, the US department of transportation national highway traffic safety administration, World Health Organization (publications on pre-hospital trauma care system), etc.
Review of the israeli trauma system training course: The learning points and brief discussion on the fundamental operational components of a trauma system
The trauma training emphasized that Israel has a unique national and local model of organizing and managing an emergency event, characterized by a central national organization that is responsible for emergency policy, management, coordination, quality control and ongoing improvement.[5,7] Preparedness for MCI in Israel is pragmatic and systematic possibly due to its unique geopolitical status, where the need for a high level of preparedness for an MCS is unquestionable. Compulsory military training for both sexes after school grade is an important social issue in Israel. But, this practice might have indirectly helped to get well-informed and better-trained volunteers in the Israeli trauma system that are cognizant of the effectiveness of team work and co-ordination. It is possible that one may adapt it further, for developing a newer local, regional or national trauma system in another geographic location depending on the ground realities.
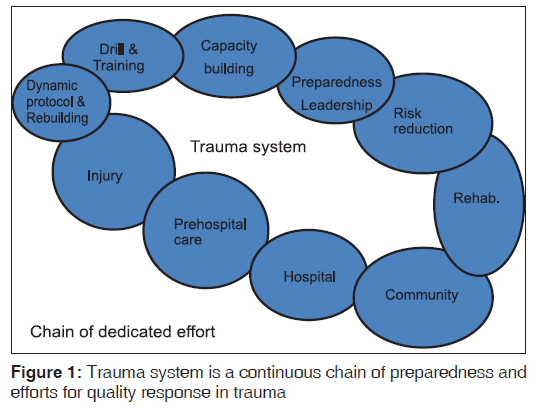
The training emphasized that a trauma system is nothing but a dynamic chain of arrangements and preparedness to provide quality response to the injured from the site of injury to the appropriate hospital for the full range of care [Figure 1]. The system involves an organized, coordinated effort in a defined geographic area that delivers the full range of care to all injured patients and is integrated with the local public health system. The aim of a trauma system is to save maximum lives through preparedness to achieve speed and efficiency in providing quality response in traumatic events. It ensures that all injured patients gain access to the appropriate level of care in a timely, coordinated and cost-effective manner. Philosophically, the trauma victim is an injured person who requires timely diagnosis and treatment of actual or potential injuries by a multidisciplinary team of health care professionals, supported by the appropriate resources, to diminish or eliminate the risk of death or permanent disability. The trauma course also emphasized that a modified ATLS protocol and save and run policy is employed by the trauma response team that is backed by an efficient high-tech ambulance rescue system and motivated and well-informed public volunteers in Israel. Pre-hospital care in a trauma system is nothing but the closest appropriate facility for immediate care for the victim’s injury. A trauma system must determine the appropriate level of care for each type of injury. Pre-hospital rescue is a weak link in trauma management in many developing countries. Sensitizing the society about trauma, both prevention and treatment, is essential.
Manpower training at every level or cadre of health worker, besides doctors, is needed to develop an efficient trauma system so that every person managing the trauma victim becomes a knowledge worker and can speak in the “same language” and wavelength. An infrastructure like the National Medical Simulation Centre is situated in Tel Aviv. It is a mannequin-based medical simulation center dedicated for virtual learning and medical education. As a part of trauma training, there was an on-camera drill followed by an action replay and debriefing session by experts to analyze trainees’ quality of response to the given clinical trauma scenario. The facility emphasized that medical simulation may be a potential tool to train all levels of health care professionals to enhance clinical techniques, speed, communication skills, managerial efficiency and team work. There are permanent actors employed by the government who can act as real trauma victims. For example, two actors came to disturb participants as patient’s attendants and demanded quicker resuscitation during such drills. Medical graduates of Israel have to pass the medical simulation practical exam. The Megan David Adom is the Centralized Ambulance and Rescue Organization of Israel. The Tel Aviv headquarter demonstrated how the Israeli ambulance and rescue services work coherently to maintain a high level of accuracy and speed in victim evacuation with a “save and run” policy rather than “scoop and run” policy. The headquarter can trace the entire movements of their ambulances in a real time manner (e.g., their exact location and distance from the hospital). Various categories of ambulances exist with different levels of capabilities for disasters. All persons of the ambulance, including the driver, are fully trained for pre-hospital rescue and care. There are large numbers of volunteers from different localities to support pre-hospital rescue with round the clock mobile connectivity. Conventional, chemical and radiological mass casualty management facilities at Rambam and other hospitals emphasized that low-cost equipments are often enough to set up such facilities. For example, designated warm running tap-water facility can be easily installed near the entrance of the hospital for immediate decontamination in such disasters. Protective gear is required by immediate care givers to deal with such unconventional events. For radiation disaster assessment, a few portable Guiger-Mullar counters are required in the emergency area. In all trauma centers, a dedicated Trauma Shock Room exists to effectively treat trauma victims in hypovolemic shock. The entire emergency drugs and materials are kept in transparent containers so that any of these items can be picked up by any caregiver without any extra effort or delay.
Mass casualty management strategy is closely linked to the existing trauma system. In fact, achieving excellence in the treatment of a single trauma victim in routine situations is the cornerstone of preparedness to a MCS in the Israeli model. Written protocols and guidelines for different disaster situations (updated from time to time) are prepared and used in every hospital to efficiently deal with MCI, because the right decision takes time, which is premium in disasters. These protocol books are to be opened and followed like a standing order once disaster is declared by the appropriate authority. Periodic drills are must for preparedness for MCI. External peer review by independent observer from another hospital during and after a drill enhances quality of response in real situations. The deficiencies and lacunae in the existing system are identified through such drills and protocols changed accordingly to remain dynamic for actions. Trauma co-ordinators and Triage officers should be identified for each hospital disaster management team. Sustaining a trauma system and managing an MCI is an interdisciplinary team effort, and it needs the highest level of support from the hospital administration. The preparedness, planning, manpower training, advocacy and periodic drills may have a major impact on the ability of a hospital’s team to respond to most of the challenges encountered in trauma and to continue to function in real time in disaster situations. Investing adequate resources on continuous education, manpower training, motivation, team-work, co-ordination and advocacy at all levels of workers, including creation of a large number of public volunteers, is required for capacity building to develop a trauma system for a region.
Planning, infrastructure development, information sharing system for co-ordination, human resource development and advocacy are the major groundwork required to formulate a local trauma system for capacity building. Triage means the process of classifying patients according to the severity of their injuries to determine how quickly they need care; a useful dictum in MCI in the pre-hospital or acute phase.[4] In MCI, a triage involves rapid primary survey and sorting of injured people for allocating them to treatment according to a system of priorities designed to maximize the number of survivors based on the urgency of their need to medical care and on perceived likelihood of benefit from immediate medical treatment in the light of limited resources available.
There are four fundamental operational components of a trauma care system,[2] and they are: (1) Injury prevention, (2) pre-hospital care, (3) acute care facilities and (4) post-hospital care: Rehabilitation begins early and continues when the patient returns to their local community. The benefits of successful implementation of this plan include: (1) A reduction in deaths caused by trauma, (2) a reduction in the number and severity of disabilities caused by trauma, (3) an increase in the number of productive working years seen in America through reduction of death and disability, (4) a decrease in the costs associated with initial treatment and continued rehabilitation of trauma victims, (5) a reduced burden on local communities as well as the government in support of disabled trauma victims and (6) a decrease in the impact of the disease on “second trauma” victims–families. The vision of developing a trauma system should have eight key fundamental infrastructure support components for a comprehensive trauma care system to evolve.[2] They are:
Leadership
By definition, leadership is the process of social influence in which one person or a group can enlist the aid and support of others in the accomplishment of a common task; in our case, for the cause of trauma management and prevention. There may be leaders at every level of work. It is important to identify them to bring dynamism to the system.
Professional resources
To create a trauma system, there is need of knowledge-workers in every level of work. There shall be a distributed network of acute care facilities implemented across the region or the country. Most facilities, whether small community hospitals or large tertiary care centers, shall have a designated role to play in the trauma system and the capacity to manage injured patients to one degree or another. Each participating facility’s available resources shall be catalogued and capabilities defined to facilitate patient management/ movement decisions. Patients transferred between facilities should receive care using established guidelines based on patient condition.
Education and advocacy
Advocacy is nothing but speaking or writing for support of the cause, the cause of trauma to educate everybody in the chain of management: Beneficiaries, stakeholders and the society. Advocacy is basically to educate the 3 Ps’: (1) Population, (2) providers and (3) policymakers. Educating and even lobbying effort in the public and the legislature to increase awareness of creating capabilities and implementing a trauma system.
Information management
Accurate and reliable information on injuries from a statewide perspective is the necessary foundation to guide performance and injury prevention activities. Mandatory and systematic data collection can identify trends and lead to novel and better interventions, and can help develop, implement and maintain a State Trauma Registry. All injury care providers should be a part of the system and provide data to a system-wide database. Trauma care shall be monitored. All facilities that participate in the trauma system should contribute to the national trauma database (Trauma Registry), and there shall be a mechanism to fund such a trauma database at the state and national levels.
Finances
The appropriate match of resources should be identified for injured patients with special needs, such as the elderly, remote rural or pediatric patients. Both generation and sustainability of funds is pivotal. Authentic statistics and research can help generate public and legislative support for more funds.
Research
Research shall be conducted to determine the effectiveness of the current practices, guidelines, resource allocations and system capabilities. Mandatory and systematic data collection can identify trends and lead to new interventions. Studies should target specific local issues and focus efforts to areas where they can make a difference. The need is to identify high-risk groups through data analysis research. For example, the appropriate volume of patients with specific injuries that need the highest level of care should be studied and clearly identified so that research and treatment options can be continually explored.
Technology
The trauma system should be linked on a regional basis through databases and technology to ensure efficient and effective patient care region/nationwide. Innovative treatment methods should be explored, e.g., utilization of mobile trauma units, telemedicine for rural areas. There should be consistent standards for rural and urban trauma services, with the goal of every community having access to a consistent level of trauma care. For example, e-medicine or telemedicine and e-information for public can enhance information and communication for advocacy in urban areas. Appropriate feedback obtained from the community can give valuable input for quality improvement measures.
Disaster preparedness and response
Such facilities in the trauma system shall have multi-casualty capabilities. The preparedness, planning and periodic drills enhance the ability of a hospital’s team to respond to most of the challenges encountered in trauma and to continue to function in disasters. Written protocols and guidelines for different disaster situations (updated from time to time) are needed for every hospital to efficiently deal with MCI, because the right decision takes time, which is premium in disasters.
An ideal trauma system should be inclusive in nature, which means that the trauma care system will: (1) Address the needs of all injured patients requiring hospitalization for injury and (2) utilize all qualified medical resources.[8,9] Injured patients should be delivered in a timely manner to the nearest appropriate facility. Inherent in the transfer of any trauma patient is feedback from the receiving to the transferring facility. Some useful dictums may be as follows: (1) The trauma system should ensure that inter-facility transfers occur in a timely fashion commensurate with patient’s clinical needs, (2) the trauma system should establish standards for the mode of transportation and qualifications of transport personnel, (3) the trauma system should have a model transfer agreement and (4) the trauma system should ensure that all inter-facility transfers are based on patient needs and are in the best interest of the patient.[8]
The goal of treatment in an MCI is to deliver an acceptable quality of care while preserving as many lives as is possible.[6] Theoretically, the capacity of the hospital is its ability to manage a load of patients in the range of 20% of the hospital bed capacity. Planning and drilling are the ways to minimize deviations from the guidelines and to avoid management mistakes. Quality assurance in trauma care delivery involves development of standards in care, identifying authority to change policies (including all procedures and protocols that address trauma care services), monitoring compliance with the set standards, process of internal peer reviewing, process of analyzing, evaluating and correcting deficiencies, etc., Quality assurance shall reflect and demonstrate a process of continuous self-criticism for quality improvement, consistent with the written standard of trauma care. An oversight monitoring agency responsible for ensuring consistency in training, certification or guidelines for response and coordination of services is needed.
In summary, it may be commented that developing an efficient regional or national-level trauma system may be a time-consuming process, taking many years. The wisdom of the Israeli model may be useful to improve and streamline many important aspects of the management of trauma victims in other countries,[9] e.g., one can reorganize themselves better by (1) investing more energy in education and manpower training, (2) advocacy at all levels of workers including the public volunteers, (3) by concentrating on cost-effective management of existing facilities, (4) focusing on better preparedness and planning for trauma management, (5) periodic drills, (6) bringing practicality (pragmatism into practice), (7) high level of motivation in the workforce, (8) proactive policies and a sense of urgency from the government agencies like police and the armed forces to create capacity-building measures for disaster preparedness and (8) highest level of support from the administration. The authors feel that the wisdom and pragmatism of the Israeli model can be useful to improve important lacunae in a hitherto inefficient local or regional trauma system or to streamline work in skeletal trauma services of developing countries having fewer resources to bring consistency and acceptable standards in the field of trauma care.[9]. Exposure to the Israeli trauma system model can motivate health caregivers and others to develop interest and insight about their role in a trauma center and MCI and, finally, a future trauma system for a region or a country.
Acknowledgment
The authors would like to acknowledge Dr RK Sarma, Former Director, NEIGRIHMS, Shillong, India, and Dr A Santa Singh, Director, NEIGRIHMS, Shillong, India.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Eastridge BJ, Jenkins D, Flaherty S, Schiller H, Holcomb JB. Trauma system development in a theater of war: Experiences from operation Iraqi freedom and operation enduring freedom. J Trauma 2006;61:1366-72.
- Executive summary: Trauma system agenda for the future. The official website of the US department of transportation national highway traffic safety administration. Available from: http://www.nhtsa.gov/people/injury/ems/ emstraumasystem03/exesummary.htm. [Last accessed on 2012 Mar 22].
- Bar-El Y, Michaelson M, Hyames G, Skorecki K, Reisner SA, Beyar R. An academic medical center under prolonged rocket attack-organizational, medical, and financial considerations. Acad Med 2009;84:1203-10.
- Prehospital trauma care system. Publications of the World Health Organization. 20 Avenue Appia, 1211 Geneva 27, Switzerland: WHO Press, World Health Organization; 2005. Available from: http://www.who.int/violence_ injury_prevention/publications/services/39162_oms_new.
- Michaelson M. Rambam Trauma care manual. Unpublished manuscript. Teaching Center for Trauma, Emergency and MCS, Rambam Health Care Campus. Haifa. Israel; 2008.
- Levi L, Michaelson M, Admi H, Bregman D, Bar-Nahor R. National strategy for mass casualty situations and its effects on the hospital. Prehosp Disaster Med 2002;17:12-16. Available from: http://pdm.medicine.wisc.edu. [Last accessed on 2011 Dec].
- Shapira S, Shemer J. Managing a mass casualty incident within the hospital. Harefuah 1997;132:296-300.
- American College of Surgeons Committee on Trauma. Trauma System Consultation: The State of North Carolina August 1st–4th, 2004. Copyright 2004. The Associated Press. Available from: http://www.ncdhhs.gov/dhsr/EMS/trauma/pdf/ cotdec 04.pdf. [Last accessed 2012 Feb 12].
- Admi H, Eilon Y, Hyams G, Utitz L. Management of mass casualty events: The Israeli experience. J Nurs Scholarsh 2011;43:211-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.