Diagnostic Accuracy of a Drop Hydrogen Peroxide Test to Differentiate Between Exudative and Transudative Pleural Effusion
Citation: Bharati Taksande. Diagnostic Accuracy of a Drop Hydrogen Peroxide Test to Differentiate Between Exudative and Transudative Pleural Effusion. Ann Med Health Sci Res. 2017; 7:242-245
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The differentiation of pleural effusions as being either transudate or exudate is the first step in the diagnostic workup of the biofluid. It has been shown that physicians are not very accurate to differentiate exudate from transudate. Routinely we use Light’s criteria to differentiate between exudate and transudate pleural fluid, however, it takes about 24 hours to get the results, hence we want to use the bedside test which gives us the result within 1 minute of thoracocentesis. The aim of our study is to determine the Diagnostic accuracy of Bedside test - A drop Hydrogen peroxide test to differentiate between exudative and transudative pleural fluid in comparison with Light’s criteria. Methods: We screened 1024 patients in outpatient department and included 172 patients in the study who had clinical and radiological evidence of pleural effusion. These patients underwent aseptic thoracocentesis. A drop of 30% hydrogen peroxide was added to 2 ml of pleural fluid which was tapped bedside and we looked for presence of bubbles. Rest of the pleural fluid was simultaneously sent for Light’s criteria analysis to laboratory and the results were then compared. Result: There were 172 patients who had pleural effusion, 150 (87.21%) of them had exudative pleural effusion and 22 (12.79%) had transudative pleural effusion by Light’s criteria and 125 (72.67%) of them had exudative pleural effusion and 47 (27.33%) had transudative pleural effusion by A drop hydrogen peroxide test. 121 were the true Positives and 18 were true negatives. 4 samples were false positive and 29 samples were false negative. Sensitivity of A drop Hydrogen peroxide test was 80.7%, Specificity was 81.8%, PPV was 96.8%, and NPV was 38.3% and Diagnostic Accuracy was 80.8%. Conclusion: This Bedside Test allows for more rapid determination of the nature of pleural effusions and can be rapidly characterized as an exudate or transudate.
Keywords
Pleural effusion; Light’s criteria; A drop hydrogen peroxide test; Diagnostic accuracy
Introduction
The differentiation of pleural effusions as being either transudate or exudate is the first step in the diagnostic workup of the biofluid. Such categorization assists diagnostic and therapeutic decisions. It has been shown that physicians are not very accurate to differentiate exudate from transudate on the basis of clinical history, physical examination and radiographic findings.
Since long, pleural fluid protein level is used to separate transudate from exudate, with exudative pleural effusions characterized by a protein level above 3.0 g/dl. Use of this only protein criterion as a diagnostic biomarker for the purpose led to the misclassification of approximately 10% of the pleural effusions. Subsequently, it is demonstrated that with the use of simultaneously obtained serum and pleural fluid protein and LDH value, 99% of pleural effusions could be correctly classified as either transudate or exudate [1]. This is the basis of currently most popular diagnostic criteria (Light’s criteria) for such differentiation [2]. Transudative and exudative pleural effusions are distinguished by measuring LDH, and protein levels. Exudative pleural effusions meet at least one of the criteria whereas transudative pleural effusion meets none.
There have been many studies in the past to increase the specificity of Light’s criteria for differentiation of pleural fluid as exudate and transudate; most of us still prescribe Light’s criteria as the differentiation criteria of the pleural biofluid.
A handful of biochemical parameters like: pleural fluid to serum cholinesterase ratio, pleural fluid viscosity pleural fluid cholesterol level, pleural fluid to serum bilirubin ratio, modern radiological investigations like computed tomography, Cellfree DNA assay, capillary electrophoresis study, oxidative stress panel analysis of the pleural fluid are attempted for the purpose to differentiate exudate and transudate in recent years [3]. The results of all these tests are time consuming requiring nearly 24 hrs.
Therefore other bedside tests to differentiate transudate and exudate pleural effusion have been developed. These are:
1. Pleural pH [4].
2. Pleural glucose [5].
3. A drop Hydrogen peroxide test [6].
The basis of Hydrogen peroxide test is that the level of catalase activity within the fluid can be used to characterize the type of fluid. A unique characteristic of the exudative fluid is increased catalase activity. Catalase speeds the decomposition of hydrogen peroxide to water and oxygen hence a simple bedside test can be done to verify the presence of catalase. If profuse bubbling occurs within one minute of the addition of hydrogen peroxide, it signifies exudative fluid. The bubbling occurs as a result of the decomposition reaction. When hydrogen peroxide is added to transudative fluid, bubbling is not observed.
Sarkar et al. [6] stated that the Sensitivity and specificity of a drop hydrogen peroxide test is equivalent to Light’s criteria and the pre-analytical error can be definitely reduced if the test is performed at the site of sample collection.
Why this study?
Routinely we use Light’s criteria to differentiate between exudate and transudate pleural fluid, however, it takes about 24 hours to get the results, hence we want to use the bedside test which gives us the result within 1 minute of thoracocentesis.
Aim
To determine the diagnostic accuracy of A Drop hydrogen peroxide test in comparison to light’s criteria.
Objectives
To determine the sensitivity, specificity, positive and negative predictive values and diagnostic accuracy of a drop hydrogen peroxide test in comparison to Light’s criteria to differentiate between exudative and transudative pleural effusion.
Materials and Methods
Study design
Diagnostic accuracy study
Study setting
Study was conducted in the Medicine department of rural hospital in central India.
Study population
All the consecutive patients of pleural effusion admitted in Medicine Ward from October 2014 to September 2016 were included.
Inclusion criteria
All patients of pleural effusion more than 13 years of age willing to give consent for thoracocentesis
Exclusion criteria
Unwilling for thoracocentesis
Methodology
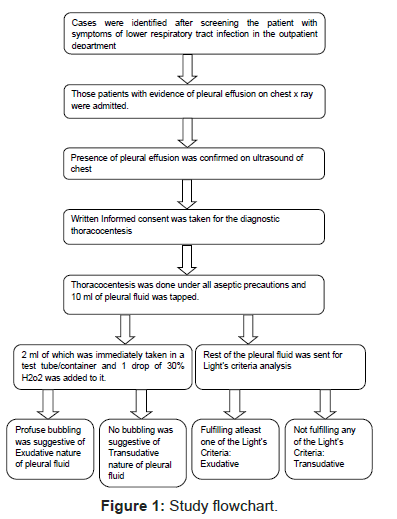
The study was conducted in the department of Medicine of a rural hospital in Central India. A total of 1024 patients were screened in an outpatient department who had symptoms of lower respiratory tract infection that are fever, cough, and breathlessness. Those who had clinical signs of pleural effusion underwent radiological investigation like chest X-Ray and ultrasound for the confirmation as shown below in study flowchart in Figure 1. Those 172 with pleural effusion were admitted. Patients who gave consent underwent thoracocentesis and approximately 10 ml pleural fluid was tapped under all aseptic precautions. 2 ml of this pleural fluid was taken in a test tube and a drop of 30% hydrogen peroxide was added to it bedside to see for the presence of bubbles. The presence of profuse bubbling signified exudative and its absence signified transudative pleural fluid. The rest of the pleural fluid was simultaneously sent to the lab for routine biochemical tests which included analysis of Light’s criteria.
Results
A total of 1024 patients were screened in the outpatient department who had symptoms of lower respiratory tract infection such as fever, cough, and breathlessness. Those who had evidence of pleural effusion clinical and radiological were admitted and some underwent ultrasound chest for confirmation. The baseline features of the study population are given below in Table 1.
| Character | Number (n=172) |
|---|---|
| Male | 117 |
| Female | 55 |
| Fever | 121 |
| Cough | 118 |
| Breathlessness | 133 |
| Loss of appetite | 84 |
| Weight loss | 50 |
| Right sided pleural effusion | 73 |
| Left sided pleural effusion | 81 |
| Bilateral pleural effusion | 18 |
Table 1: Baseline characteristics of the study population.
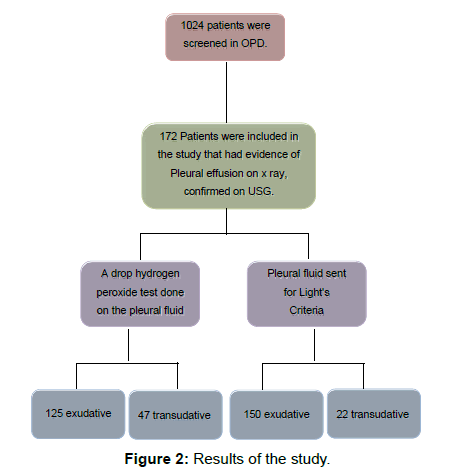
172 of those had confirmed pleural effusion written consent was taken for thoracocentesis and under all aseptic precautions about 10 ml of pleural fluid was tapped, 2 ml of that fluid a drop of 10% H2O2 was added bedside and we looked for presence of profuse bubbling and the rest of the pleural fluid was immediately sent to the laboratory for investigations for Light’s criteria and cytology.150 (87.21%) of them had exudative pleural effusion and 22 (12.79%) had transudative pleural effusion by Light’s criteria. Out of 172 samples, 150 of them were exudative and 22 transudative by Lights criteria and 125 exudative and 47 were transudative by Hydrogen peroxide test as shown in below Figure 2.
The nature of the pleural fluid diagnosed by both the reference and index tests is given below in Table 2. 121 were diagnosed as exudative by both A Drop Hydrogen Peroxide Test as well as by Light’s criteria that is they were the true positives.18 were true negatives that is transudate by both the tests.4 samples were false positive that is exudate by H2O2 test but transudate by Light’s criteria and 29 samples were false negative that is exudate by Light’s criteria but transudate by H2O2 tests.
Hydrogen peroxide test (Index Test) |
Light’s criteria (Reference Test) | ||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 121 (True Positive) | 4 (False positive) | 125 |
| Negative | 29 (False negative) | 18 (True Negative) | 47 |
| Total | 150 | 22 | 172 |
Table 2: Result of the nature of the pleural fluid by both a drop hydrogen peroxide test and light’s criteria.
The sensitivity and specificity of A drop hydrogen peroxide test is 80.7% and 81.8% respectively, PPV (Positive predictive value) of 96.8% and NPV (Negative predictive value) of 38.3%. The diagnostic accuracy of A drop hydrogen peroxide test is 80.8%.
Discussion
Investigating pleural effusion which is evident on chest radiographs should follow a stepwise approach to diagnosis.
Diagnosis should always begin with the clinical history, physical examination, chest radiography and followed by thoracocentesis. The next step is to differentiate the pleural fluid into transudate and exudates. Analysis of the pleural fluid can narrow the differential diagnosis. Establishment of diagnosis with the analysis of pleural effusion can be done in approximately 75 percent. The gross appearance of the fluid and biochemical parameters can be key to a direct diagnosis or can be process indicating the next step. If underlying cause can be sought with the help of biochemical tests treatment should be started. If not CT, pleural biopsy (radiologically or medical thoracoscopy) or further invasive investigations can be warranted.
There is no biochemical marker that allows a complete differentiation between transudates and exudates.
Over many years down, various tests have developed to diagnose the nature of the pleural fluid with varying sensitivity and specificity. Out of all, Lights criteria developed by Light et al. [2] has found to have maximum sensitivity and specificity of 100% and 83% respectively and is considered gold standard for analyzing the nature of pleural fluid and differentiating it into exudates and transudates.
In last two decades many bedside test are developed which would shorten the time between the thoracocentesis and the diagnosis so that rapidly treatment could begin. The rapid bedside tests are portable, inexpensive, easy to use, and can analyze pleural fluid in a short span of time requiring less than 24 hrs. Pleural pH, Pleural glucose and Hydrogen peroxide test are the ones which are used bedside.
In our study in a sample of 172 cases of pleural effusion 121(True positive) pleural effusion was diagnosed exudative by both Lights criteria as well as By Hydrogen peroxide test and 18(True negative) transudative by both the tests. A drop hydrogen peroxide test showed sensitivity of 80.7% and specificity of 81.8%, PPV (Positive predictive value) of 96.8% and NPV (negative predictive value) of 38.3% which is slightly lower than the previous study done by Sarkar et al. The diagnostic accuracy of A Drop hydrogen peroxide test in our study is 80.8% to differentiate the nature of pleural fluid into exudative and transudative.
Sarkar et al. [6] in his study with the sample size of 52, observed that all the exudative pleural fluids which were considered for the study showed profuse bubble formation after addition of hydrogen peroxide . Whereas transudative pleural fluids which are considered for the study showed no bubble formation after addition of hydrogen peroxide but addition of catalase or blood in transudate showed profuse bubble formation after addition of H2O2. The bubble formation in blood mixed or catalase mixed transudate was also inhibited by supplementation of sodium cyanide or sodium azide prior addition of H2O2. The bubble formation in the exudate was definitely due to its increased catalase activity which was significantly less in transudate. They concluded blood uncontaminated pleural fluid sample this newly developed protocol’s sensitivity and specificity will be equivalent to Light’s criteria probably with more advantage as by this procedure transport of the sample to the clinical laboratory is not required due to its inherent simplicity. Performance of the test at the site of sample collection will definitely reduce preanalytical error.
Bryan Jepson and his team in the review concluded that the level of catalase activity within the fluid can be used to characterize the type of fluid [7]. Increased catalase activity is the unique characteristic of exudative fluid. A simple bedside test using hydrogen peroxide to verify the presence of catalase can be done, due to the ability of catalase to speed the decomposition of hydrogen peroxide to water and oxygen. And the fluid can be classified as transudative or exudative. If profuse bubbling occurs within one minute of the addition of hydrogen peroxide to fluid, it signifies exudative fluid. The bubbling occurs as a result of the decomposition reaction. If hydrogen peroxide is added to transudative fluid, bubbling does not occur. The sensitivity and specificity of this test is believed to be equivalent to the widely used Light’s criteria that is 98% and 91.3% respectively. Whereas the other bedside tests mentioned like Pleural fluid pH and pleural glucose has low sensitivity and specificity as compared to catalase test.
Lesho EP et al. in his study of 42 samples concluded that the determination of pleural fluid pH using pH paper is unreliable and should not be considered an acceptable alternative with very low sensitivity of 36% [4]. In patients of parapneumonic and malignant effusions a low pleural fluid pH has diagnostic, prognostic, and therapeutic implications.
Strengths
Sample size was larger in our study as compared to the other study done by Sarkar et al. Wide range of variety in aetiology of pleural effusion was used in the study like tuberculosis, heart failure, pancreatitis, chronic kidney disease, cirrhosis, malignancy etc.
Limitations
The traumatic and the hemorrhagic effusions were not excluded in our study, probably that would have led to large number of exudative pleural effusion.
Conclusion
This bedside test allows for more rapid determination of the nature of pleural effusions and can be rapidly characterized as an exudate or transudate.
Firstly, this will shorten the diagnostic time and allow for treatment options to be considered with less delay by eliminating the need for lab work that may require several hours. Secondly, the low price of the test will make it more acceptable in the limited lab resource facility. Additional tests can be incorporated to increase the accuracy and the diagnostic ability of the test. These tests may serve to determine the cause of the effusion once the exudative or transudative nature has been verified by the hydrogen Peroxide test. For example, testing for amylase concentration in the pleural fluid would allow the physician to know if the effusion is due to pancreatic dysfunction. Detecting leukocyte concentration may help to diagnose an infectious exudative effusion. With its sensitivity and specificity equivalent to that of Lights Criteria, not only will this test decrease diagnostic time, but it will also benefit hospitals and clinics in India that may be less equipped to conduct standard diagnostic tests.
Acknowledgements
The authors would like to acknowledge Dr Prashanti Eachempati, Dr Jyotsna S Dr Medha Joshi and Dr Arunita Jagzape for valuable inputs in designing the ECE module. We thank Dr Dayanand Huddar and Rohit Ishwar Dhole for help in carrying the study.
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
- Costa M, Quiroga T, Cruz E. Measurement of pleural fluid cholesterol and lactate dehydrogenase: A simple and accurate set of indicators for separating exudates from transudates. Chest. 1995;108:1260-1263.
- Light RW. Pleural effusions. Vol. 95, Medical Clinics of North America. 2011. p. 1055-1070.
- Porcel JM. Pleural fluid biomarkers: Beyond the light criteria. Vol. 34, Clinics in Chest Medicine. 2013. p. 27-37.
- Lesho EP, Roth BJ. Is pH paper an acceptable, low-cost alternative to the blood gas analyzer for determining pleural fluid pH? Chest. 1997;112:1291-1292.
- Rahman NM, Mishra EK, Davies HE, et al. Clinically important factors influencing the diagnostic measurement of pleural fluid pH and glucose. Am J Respir Crit Care Med. 2008;178:483-490
- Sarker, S. et al. A drop of hydrogen peroxide can differentiate exudative pleural effusion from transudate – Development of a bedside screening test. Clinica Chimica Acta. 2009: 83-86.
- Yale S, Brace C. Characterisation of pleural effusion using the multivariate bedside test. 2010.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.