Effectiveness of Hip Muscles Strengthening with Kegels Exercise in Treatment of Stress Urinary Incontinence among Postmenopausal Women: A Randomized Controlled Trial
Received: 29-Nov-2023, Manuscript No. AMHSR-23-121596; Editor assigned: 01-Dec-2023, Pre QC No. AMHSR-23-121596 (PQ); Reviewed: 15-Dec-2023 QC No. AMHSR-23-121596 ; Revised: 02-Jan-2025, Manuscript No. AMHSR-23-121596 (R); Published: 13-Feb-2025
Citation: Diksha G, et al. Effectiveness of hip muscles strengthening with kegels exercise in treatment of stress urinary incontinence among postmenopausal women: A Randomized Controlled Trial. Ann Med Health Sci Res. 2025;15:1-22
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose: Urinary incontinence is a debilitating condition with hygiene, social, and psychological consequences that greatly affect quality of life. However, there's a lack of research in the current literature on the combined effect of Kegel exercises and hip muscle strengthening as physiotherapy intervention for treating stress urinary incontinence in postmenopausal women.
Relevance: In recent decades, aging population has surpassed the younger generation due to improved resources and technology. Unfortunately, the significant issue of stress urinary incontinence in postmenopausal women has been overlooked, leading to growing global health burden and impacting numerous lives.
Participants: 70 females who attained menopause and were diagnosed with stress urinary incontinence in the age of 45-70 years.
Methods: In this randomized control trial conducted in tertiary hospitals and outreach programs, group A received a combination of hip muscle strengthening and Kegel exercises, while group B received Kegel exercises alone, following ACSM guidelines for 8 weeks. Their perfect scores were assessed before, after, and at a 1-month follow-up. Analysis: Data analyzed using SPSS 27.0, Student’s paired and unpaired t-test and repeated measures one-way ANOVA were used.
Results: Majority of group A was 15.85, which increased to 25.81 post-treatment and was 36.85 at follow-up, group B was 15.46, which was increased to 23.28 post-treatment and 33 at follow-up, which indicated that the group A score was better than group B and was extremely significant statistically (P=0.0001).
Conclusion: Combining kegel exercises in different positions with hip muscle strengthening for postmenopausal women suffering from stress urinary incontinence significantly improved perfect score. Clinical implications: Strengthening hip muscles, including gluteus and hip adductor exercises, is recommended for managing stress urinary incontinence, alleviating symptoms and improving the perfect score.
Keywords
Kegels exercise; Hip muscles strengthening; Stress urinary incontinence; Postmenopausal women
Introduction
India has a growing population of people aged 45 years and above. Due to this, women’s health of this group is an important global concern in the light of long-term effects of both chronological and ovarian ageing [1]. With an increase in chronological age, a decline in the number, quality and hormonal activity of ovarian follicles that results in menopause. Menopausal symptoms (vasomotor, vaginal and urinary incontinence) are often attributed to hormonal changes and pose health problems, in which stress urinary incontinence is more distressing hampering their lives [2]. According to Indian studies, the prevalence of stress urinary incontinence in post-menopausal women is 21.8% [3]. Apparently, 50% of postmenopausal women will acquire urogenital signs and symptoms which are underreported most of the time [4]. Only 20%–25% of symptomatic women seek medical help or discuss their symptoms due to embarrassment, misconceptions that it is a natural part of aging, and lack of awareness about available treatments.
Despite the high prevalence and diversity of urogenital symptoms; most women avoid complaining about vaginal and urinary symptoms during their postmenopausal years, which may be attributable to that the urogenital symptoms can be relieved rapidly after local estrogenic administration [5]. While these symptoms may not directly endanger one's life, they do adversely affect quality of life. They lead to personal distress and discomfort, create a misconception that suitable treatments are unavailable, clash with cultural norms, and promote the belief that these symptoms are a natural part of the aging process [6, 7].
Managing stress urinary incontinence becomes a significant challenge for postmenopausal women who have to juggle various responsibilities, including household chores and, for some, professional obligations. The fatigue and weakening of muscles that occur due to decreased estrogen production in the postmenopausal period worsen the challenges of handling everyday tasks. This has a negative effect on both physical and mental health. Instances of urine leakage when coughing, sneezing, laughing, or lifting heavy objects result in emotions of embarrassment, remorse, and unease. These feelings contribute to social seclusion and a tendency to avoid engaging with others.
In Stress Urinary Incontinence (SUI), there is involuntary release of urine during physical activities that raise abdominal pressure, such as coughing, sneezing, laughing, or exercising. Among women, the most common type of urinary incontinence is SUI. The underlying causes of SUI can be multifactorial, including weakened pelvic tissues and muscles that support the bladder and urethra, as well as a weakened sphincter muscle controlling the urethra. Contributing factors such as pregnancy, childbirth, prior pelvic surgery, aging, chronic cough or straining, obesity, and smoking may also play a role in the development of SUI [8].
Due to reduced circulating estrogen levels and aging certain anatomic and physiologic changes in the vagina associated with menopause are seen. The vagina, vestibule, and trigone of the bladder modulate cellular proliferation and maturation which consists of a high concentration of estrogen receptors. This imbalance results in physiological, biological, and clinical changes in the urogenital tissues which include less collagen content and hyalinization, decreased elastin, thinning of the epithelium, enhanced density of connective tissue, modified visual and operational characteristics of smooth muscle cells, and reduced blood vessels. As a result, labia minora becomes thinner and experiences regression and retraction. The hymenal carunculae also go through involution and lose flexibility, resulting in notable dyspareunia. The opening of the urethra undergoes an increase in noticeable change in comparison to the vaginal introitus and is at a higher risk of experiencing physical irritation and trauma. Physiologic changes result in a reduction in vaginal blood flow, lubrication, flexibility, vaginal tissue strength and elasticity of the vaginal vault, and increased vaginal pH (11–13) that leads to epithelial damage [4].
The developmental origins of the female genital tract and lower urinary tract are shared, originating from the urogenital sinus during embryonic development. As a result of this common origin, both these tracts are susceptible to the effects of estrogen deficiency following menopause. Estrogen receptors, encompassing both the α and β types, are present within the lower urogenital tract. However, their quantities decline with the onset of menopause, a decrease that can potentially be reversed through estrogen therapy. The scarcity of estrogen in post-menopause results in a decrease in collagen, hyaluronic acid, and elastin levels. This leads to the thinning of the epithelium, changes in the functioning of smooth muscle cells, and an increase in the density of connective tissue along with a reduction in the number of blood vessels. These changes reduce elasticity of the vagina, increase increases incontinence issues [9].
Various treatment options are available as pharmacologically treating condition with hormone replacement therapy and nonpharmacological intervention which includes physiotherapy, behavioural therapy and various other approaches have been explored. Yet, when considering conservative treatments, it's reasonable to inquire if incorporating exercises could enhance the effectiveness of pelvic floor rehabilitation, taking into account anatomical and biomechanical factors.
Dr. Arnold Kegel first reported successful outcomes in women with SUI symptoms using pelvic floor muscle exercises, several physiotherapy methods have been used (biofeedback, electrostimulation, vaginal cones, vaginal ball, individual or group therapy) in the treatment of UI, with different success rates. In the literature, most PMFT programmes have been performed under regular control of a physiotherapist in physiotherapy centres, which may not be cost-effective and is time-consuming [10]. In a recent review, Pelvic Floor Muscle Training (PMFT) has been found to improve UI symptoms in all types of incontinence [11].
Kegels prevent urinary incontinence in postpartum women and they are effective, one of the safest behavioural therapies without side effects and complications. It is more advantageous than receiving no treatment in the care of women with stress urinary incontinence. This approach reduces the occurrence of urinary incontinence and provides relief from its symptoms [12].
Magnetic resonance imaging and electromyography have revealed a connection between the levator ani, fossa ischioanalis, and gluteus maximus muscles regarding both their structure and function. These studies suggest that the contraction of hip adductor and gluteus muscles aids in the coordinated contraction of pelvic floor muscles and the striated muscle in the urethral wall [13].
Numerous studies have explored pelvic floor dysfunction and the effectiveness of kegel exercises in treating stress urinary incontinence. However, the specific application of hip muscle strengthening alongside kegel exercises to treat stress urinary incontinence among postmenopausal women remains an underexplored area of research.
The lack of research specifically targeting postmenopausal women with stress urinary incontinence is concerning due to several reasons. Firstly, women may feel reluctant to discuss their condition despite its impact on daily life, psychology, and social interactions. Secondly, many women mistakenly believe that SUI is an inevitable consequence of aging and therefore, do not consider it a problem worth addressing. Lastly, even among those who recognize SUI as an issue, the lack of knowledge about whom to consult or what treatment options are available further impedes seeking help.
Addressing this gap in the literature is crucial not only for the affected individual’s well-being but also for the overall public health. As the global population ages, the number of postmenopausal women with stress urinary incontinence is likely to increase, leading to a growing burden of disease if left unaddressed.
Need of the study
- Urinary Incontinence is a debilitating and distressing condition with hygiene, social, and psychological implications with a negative impact on QOL.
- There is a lack of existing studies with follow-up treatment after hip muscles strengthening combined with pelvic floor muscles strengthening and long-term effect on SUI.
- Within the current body of literature, there is a shortage of research examining the impact of Kegel exercises and strengthening of hip muscles as a form of physical therapy intervention for addressing Stress Urinary Incontinence (SUI) in postmenopausal women.
Due to this major reasons, it is not only mandatory to focus on this issue it must be taken into consideration as from last few decades the number of aging population is exceeding the young population due to better resources and advanced technology but somewhere this huge area of postmenopausal women suffering from stress urinary incontinence is being neglected, due to which its increasing the global burden of disease and affecting huge amount of lives.
By investigating the effectiveness of hip muscle strengthening with kegel exercises in treating stress urinary incontinence among postmenopausal women, this study aims to fill the existing gap in the literature and contribute valuable insights to the field of women's health and urology.
Research question
What is the effect of hip muscles strengthening with kegels exercise in treatment of stress urinary incontinence among postmenopausal women?
Aim and objectives
Aim: To determine the effectiveness of hip muscles strengthening with kegels exercise in treatment of stress urinary incontinence among postmenopausal women
Objectives
- To determine the effectiveness of kegels exercises on frequency, strength and QOL in stress urinary incontinence among postmenopausal women
- To determine the effectiveness of kegels exercises combined with hip muscles strengthening on frequency, strength and QOL in treatment of stress urinary incontinence among postmenopausal women
- To compare the effectiveness of hip muscles strengthening with kegels exercise on frequency, strength and QOL in treatment of stress urinary incontinence among postmenopausal women.
Hypothesis
Alternate hypothesis: There is positive effect of hip muscles strengthening with Kegel exercise in treatment of stress urinary incontinence among postmenopausal women.
Null hypothesis: There is no significant effect of hip muscles strengthening with Kegel exercise in treatment of stress urinary incontinence among postmenopausal women.
Operational definition
Stress Urinary Incontinence (SUI) is a prevalent condition characterized by leakage of urine during moments of physical activity that increases abdominal pressure, such as coughing, sneezing, laughing, or exercise.
Literature Review
Traub ML, et al. conducted a study titled "reproductive aging and its effects on general health," conducted by Traub ML and Santoro N in 2010, it was found that reproductive aging is accompanied by non-reproductive endocrine changes leading to hypergonadotropic hypogonadism and amenorrhea. These changes are biochemically detectable irrespective of clinical signs. Alterations in the hypothalamic-pituitary-ovarian axis also influence other hormonal axes like adrenal androgen and somatotropic axis. Existing literature suggests a decline in the somatotropic axis during reproductive aging. The interplay between reproductive aging and adrenal androgen axis changes is intricate, further complicated by age-related adrenal axis declines early in reproductive years. These shifts could significantly impact overall health. Efforts to counteract hormonal declines using exogenous hormone therapy have yielded mixed outcomes. The timing and speed of changes during reproductive aging appear to influence metabolism, cardiovascular risk, cognition, bone density, and mortality.
Deecher DC, et al. conducted a study on “physiology and thermoregulatory dysfunction and current approaches to the treatment of vasomotor symptoms” delved into Vasomotor Symptoms (VMS) associated with menopause, including hot flushes and night sweats. While the physiology of hot flushes isn't fully understood, comprehending the intricate thermoregulatory circuitry underlying VMS is crucial for innovative treatments. This circuitry comprises core body temperature, neurochemical signaling, and peripheral vasculature. Multiple physiological systems, including the neuroendocrine system, contribute to thermoregulation. The declining levels of ovarian steroids are well-established causative factors in initiating thermoregulatory dysfunction. The paper reviews the physiology behind this dysfunction causing VMS and its connection to present and future treatment options.
Uma Singh, et al. conducted a study on “Prevalence and risk factors of urinary incontinence in Indian women” observed 21.8% (656 out of 3000) women being incontinent in a hospital-based cross-sectional study. Stress incontinence was predominant (73.8%), followed by mixed (16.8%) and urge incontinence (9.5%). Factors like age over 40, multiparity, postmenopausal status, BMI over 25, diabetes, asthma, and habits like tea, tobacco, pan, and betel were linked to higher urinary incontinence prevalence in univariate analysis. Multivariate analysis established significant associations between overall incontinence and age over 40, multiparity, vaginal delivery, hysterectomy, menopause, tea and tobacco use, and asthma. Stress incontinence, however, wasn't specifically connected to menopause.
Portman DJ, et al. conducted a study on “Genitourinary syndrome of menopause” In 2012, the International Society for the Study of Women's Sexual Health (ISSWSH) and The North American Menopause Society (NAMS) recognized the necessity to revise terminology concerning genitourinary symptoms linked to menopause. The term "Genitourinary Syndrome of Menopause" (GSM) was introduced, considered medically accurate and comprehensive compared to "vulvovaginal atrophy." GSM encompasses symptoms and signs due to estrogen and other sex steroid decline, affecting labia, clitoris, vestibule, vagina, urethra, and bladder. This may include genital dryness, irritation; burning, sexual discomfort, pain, dysfunction; and urinary urgency, dysuria, and recurrent infections.
Sturdee, et al. in his study on “Recommendations for the management of postmenopausal vaginal atrophy” The key recommendations from the International Menopause Society Writing Group are as follows: It is essential that health-care attendants routinely engage in open and sensitive discussion with postmenopausal women about their urogenital health to ensure that symptomatic atrophy is detected early and appropriately managed. Treatment should be started early and before irrevocable atrophic changes have occurred. Treatment needs to be continued to maintain the benefits. All local estrogen preparations are effective and patient preference will usually determine the treatment used. Additional progestogen is not indicated when appropriate low-dose, local estrogen is used, although long-term data (more than 1 year) are lacking. If estrogen is ineffective or undesired, vaginal lubricants and moisturizers can relieve symptoms due to dryness.
Bozkurt N, et al. conducted a study on “Urogenital symptoms of postmenopausal women in Turkey”; The objective of this study was to collect data on the prevalence and risk factors of urogenital symptoms in postmenopausal women in Turkey. It concluded that Urogenital symptoms observed in our population were found to be fewer than reported previously. Symptoms that appear in the postmenopausal period may be related to several factors such as age, number of births, time elapsed since menopause, presence of diabetes mellitus, and use of hormone therapy.
Huang AJ, et al. in his study “The dayâ??toâ??day impact of urogenital aging: Perspectives from racially/ethnically diverse women”; Urogenital symptoms affect up to half of women after menopause, but their impact on women's day-to-day functioning and wellbeing is poorly understood. Postmenopausal women aged 45 to 80 years reporting urogenital dryness, soreness, itching, or pain during sex were recruited to participate in in-depth focus groups to discuss the impact of their symptoms. Urogenital symptoms can have a marked impact on sexual functioning, everyday activities, emotional wellbeing, body image, and interpersonal relations after menopause. Clinicians may need to question women actively about these symptoms, as many are reluctant to seek help for this problem.
Doyel Dasgupta, et al. in his study “Vasomotor and urogenital problems at midlife” states that during transition to menopause, women experience symptoms which vary widely. This variation is attributed not only to the hormonal change, but also to the effect of socio-demographic and reproductive factors. This study aimed to (a) Find out the rural–urban difference in experiencing menopausal problems at peri-menopausal and post-menopausal stages and (b) To identify the factors associated with these problems. Bivariate analysis finds a rural–urban difference for vasomotor, urinary and vaginal problems (p<0.05). Multivariate analysis revealed socio-demographic and reproductive factors were significantly (p<0.005) associated with vasomotor (age at menarche, menopausal and residential status, duration of breastfeeding, menstrual discharge type, use of OCP, sterilization and BMI), urinary (ages at menarche and marriage, menstrual bleeding length, use of OCP, menopausal status, monthly household expenditure and BMI) and vaginal (type of menstrual discharge, menopausal status, educational level, monthly household expenditure and BMI) problems for this study group.
Patni R. et al. in his study “Genitourinary syndrome of menopause”. The primary aim of treatment of GSM is relief of symptoms. Affecting nearly 50% of postmenopausal women, GSM also occurs in other lowâ??estrogen states, such as postpartum, during lactation, and with certain medications, such as Aromatase Inhibitors (AIs).
Janssen CC, et al. In his study titled “The effects of physiotherapy for female urinary incontinence: individual compared with group treatment randomized trial,” showing the effects of individual and group physiotherapy for urinary incontinence in women referred by their General Practitioner (GP). After individual treatment the severity of incontinence improved in 60% of the patients and the mean (95% confidence interval, CI) frequency of urine loss decreased by 8.7 times/week. After group therapy continence improved in 57%. Individual and group physiotherapy are equally effective for at least 9 months in improving incontinence in women.
Dumoulin C, et al. conducted a systemic review on “Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women.” The study's findings suggested that Pelvic Floor Muscle Training (PFMT) has the potential to either cure or enhance symptoms associated with Stress Urinary Incontinence (SUI) as well as various other types of Urinary Incontinence (UI). This intervention showed promise in reducing the frequency of leakage episodes, decreasing the amount of leakage measured through short pad tests during clinical assessments, and alleviating symptoms as measured by UI-specific symptom questionnaires. Furthermore, a separate economic evaluation included in the Brief Economic Commentary indicated that PFMT's cost-effectiveness seems favorable, warranting its consideration for inclusion in primary conservative management programs for women dealing with UI.
Verghese T, Latthe et al. conducted a systemic review on “Recent status of the treatment of stress urinary incontinence.” The aim of the study was to evaluate the impacts of Pelvic Floor Muscle Training (PFMT) for women experiencing Urinary Incontinence (UI), in contrast to no treatment, placebo or sham treatments, or other inactive control approaches. The study's conclusion indicated that PFMT has the potential to effectively alleviate or ameliorate symptoms associated with Stress Urinary Incontinence (SUI) as well as other forms of UI. The findings suggested that PFMT might lead to a reduction in the frequency of leakage episodes, decreased leakage volume measured through short pad tests during clinical assessments, and improvements in symptoms as indicated by specialized UI symptom questionnaires.
McLean L, et al. conducted a systemic review titled “Effects of PFMT for women with Urinary Incontinence (UI) in comparison to no treatment, placebo or sham treatments, or other inactive control treatments.” The review concluded that Pelvic Floor Muscle Training (PFMT) can lead to the resolution or improvement of symptoms associated with Stress Urinary Incontinence (SUI) and other forms of UI. PFMT is shown to reduce the frequency of leakage episodes, the amount of leakage as measured by short pad tests during clinic visits, and UI-related symptoms on dedicated questionnaires.
Soljanik I, Janssen, et al, conducted a study on “Functional interactions between the fossa ischioanalis, levator ani and gluteus maximus muscles of the female pelvic floor: A prospective study in nulliparous women”; This study aimed to assess the functional relationships among the Levator Ani (LA), Gluteus Maximus muscles (GM), and Fossa Ischioanalis (FI) in the pelvic floor of healthy nulliparous (never given birth) female volunteers. The study included twenty-three participants. Electromyography (EMG) readings of LA and GM were taken during voluntary pelvic floor muscle contractions (KGM) and at rest in six different body positions. MRI was used to evaluate the surface areas of LA (LAA), FI (FIA), and GM (GMA). The study found that simultaneous contractions of LA and GM were consistently observed regardless of body position in 97.2% of cases. MRI scans revealed synchronized movement of these structures, with LAA decreasing by 7.4%, GMA increasing by 6.8%, and FIA changing significantly by 3.4%. The study suggests that the morphological and functional connections between LA, FI, and GM should be regarded as the "LFG-Complex." This complex is crucial for the functional integration of the pelvic floor and has potential implications for understanding urinary continence mechanisms as well as post-surgery and obstetrical trauma related to pelvic floor disorders.
Seong-Hi Park, et al. conducted a comprehensive review of Randomized Controlled Trials (RCTs) with the aim of assessing the impact of Kegel exercises on reducing symptoms of urinary incontinence among women with stress urinary incontinence. The researchers selected RCTs involving women who practiced Kegel exercises and met specific criteria, published between 1966 and 2012. They retrieved articles from various databases and used Cochrane's risk of bias method to assess trial quality. All 11 trials contributed data to primary and secondary outcomes, revealing that Kegel exercises significantly alleviated urinary incontinence symptoms in women with stress urinary incontinence. The studies exhibited minimal variation except for the standardized bladder volumes in the pad test. The study concludes that Kegel exercises might be effective in managing stress urinary incontinence.
Linda McLean, et al. conducted a study to investigate the impact of a 12-week Pelvic Floor Muscle (PFM) training program on the structure and mobility of the urethra in women with Stress Urinary Incontinence (SUI). They randomly assigned forty SUI-afflicted women to two groups: The treatment group received physiotherapy sessions teaching proper PFM contraction and a home exercise program, while the control group received no intervention. Ultrasound imaging measured bladder neck position and mobility during coughing and Valsalva maneuver in various postures. Secondary measures included bladder diary, pad test, and questionnaires. The treatment group showed improved urethral structure and reduced bladder neck mobility during coughing. These changes weren't observed in the control group. Moreover, the treatment group exhibited better improvements in bladder diary and quality of life measures than the control group. The study concludes that supervised PFM training can enhance urethral function and reduce bladder neck motion during coughing in SUI-affected women.
Underwood D, et al. conducted a case-control study to explore potential differences in hip muscle strength between women with and without Stress Urinary Incontinence (SUI), given the possible link to musculoskeletal dysfunction. The study encompassed 48 women, 23 with SUI and 25 controls. Isometric hip strength and pelvic floor muscle performance were assessed. Hip strength was lower in the abductors and external rotators among women with SUI, though no direct correlation with symptom severity was found. Notably, the ability to rapidly contract pelvic floor muscles correlated with SUI symptom magnitude. The study suggests that hip strength might not be a significant factor in SUI interventions, while rapid pelvic floor muscle contractions seem to relate to symptom severity.
P A Norton, et al. aimed to evaluate the effectiveness of posture changes in reducing urine leakage in women with stress urinary incontinence. The study involved 65 women diagnosed with stress incontinence, who underwent standing cough stress tests in different postures. The mean fluid loss significantly reduced when participants crossed their legs or combined leg-crossing with bending forward. Forward bending alone didn't reduce fluid loss. The most effective posture led to a significant reduction in fluid loss. About 73% of subjects achieved continence through postural adjustments. The study suggests that posture changes can effectively manage stress urinary incontinence.
Sakineh Hajebrahimi, et al. conducted a study on the validity and reliability of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) and its correlation with urodynamic findings. They translated and tested the Persian version of the questionnaire on 123 patients with urinary incontinence. The questionnaire demonstrated high reliability and validity, with a strong correlation between ICIQ-UI SF scores and urodynamic parameters. The study concludes that the Persian version of ICIQ-UI SF is a reliable tool for evaluating patients with urinary incontinence and their urodynamic findings.
Margolis, et al. sought to establish the content validity of the King's Health Questionnaire (KHQ) in individuals with Overactive Bladder (OAB) in the US. They conducted interviews with 24 participants diagnosed with OAB who provided feedback on the KHQ. Overall, participants found that the KHQ comprehensively covered the impacts of OAB on their daily lives. While most items and response options were acceptable, some minor issues were noted, such as certain items being perceived as redundant or intense. The study concludes that the KHQ holds content validity and is a relevant tool for assessing the impact of OAB on the quality of life in both men and women in the US.
Allen Hosker, et al. conducted a study on the impact of childbirth on pelvic floor damage. The research involved 96 women who had not given birth before, and aimed to determine if childbirth led to damage in the pelvic floor muscles and nerves. The study utilized techniques such as concentric needle Electromyography (EMG), pudendal nerve conduction tests, and perineometer-based assessment of pelvic floor contraction. The findings indicated EMG evidence of re-innervation in pelvic floor muscles after vaginal delivery in 80% of the participants. Women with longer active second stages of labor and heavier babies exhibited more EMG evidence of nerve damage. Forceps delivery and perineal tears did not significantly affect the degree of nerve damage observed. The study concluded that vaginal delivery often causes partial denervation of the pelvic floor muscles, followed by re-innervation. In some cases, severe denervation is linked to urinary and fecal incontinence.
Zanetti MR, et al. conducted a study to evaluate the impact of supervised physiotherapeutic pelvic floor exercises on treating female stress urinary incontinence. The study randomized 44 women with stress urinary incontinence into two groups: One receiving supervised pelvic floor exercises for three months and the other without supervision. The participants were evaluated before and after treatment using quality-of-life questionnaires, pad tests, micturition diaries, and subjective assessments. The results demonstrated that the supervised group showed more significant improvement in various measures, including the pad test, micturition diary, and quality of life. Additionally, a higher percentage of participants in the supervised group expressed satisfaction with their treatment. The study concluded that supervised pelvic floor muscle exercises yielded better results in both objective and subjective evaluations compared to unsupervised exercises.
Kashanian M, et al. conducted a study randomized trial involving 91 women with urinary incontinence. They evaluated the effects of pelvic floor muscle training (PFMT or Kegel exercises) and assisted PFMT using a resistance device (Kegelmaster device) on urinary incontinence. The participants were divided into two groups: one utilizing the resistance device and the other performing standard PFMT exercises. Both groups showed significant improvement in measures such as quality of life, pelvic floor muscle strength, social activities participation, severity of urinary incontinence, and number of involuntary urine passages after 1 and 3 months of intervention. The study concluded that both PFMT methods were effective for improving urinary incontinence in women.
Sar D, et al. conducted a study on the effect of pelvic floor muscle training on stress and mixed urinary incontinence and quality of life. The study recruited consecutive instances of women experiencing stress or mixed Urinary Incontinence (UI) from outpatient urology clinics linked to both a county hospital and a university hospital in Izmir, Turkey. After initial assessments, 41 women were randomly divided into two groups: The Pelvic Floor Muscle (PFM) training group and the control group. The PFM training involved daily sessions of both fast and slow contractions in various positions, alongside teaching participants the "knack" technique. This intervention spanned 8 weeks, during which the exercise group received weekly motivational phone calls. The untreated control group had no contact during this period. The outcomes were assessed using the Incontinence Quality of Life (I-QOL) Questionnaire, episodes of leakage through a 3-day bladder diary, a 1-hour pad test, and PFM strength measurements. Thirty-four women completed the trial. The average age was 41.82 years in the exercise group and 44.64 years in the control group. Both groups were statistically comparable in terms of key demographic and clinical attributes. After 8 weeks, notable differences were observed between the PFM training group and the control group in terms of the 1-hour pad test, episodes of leakage in the 3-day bladder diary, PFM strength, and I-QOL scores (P=.01). The study concluded that an 8-week PFM training regimen substantially increased PFM strength, enhanced quality of life, and reduced the frequency of urinary incontinence episodes.
Jahromi M, et al. conducted a study on to evaluate the effect of pelvic muscle exercises on urinary incontinence and self-esteem in elderly females with stress urinary incontinence. Fifty elderly females aged 60-74 years participated in the study. They underwent training sessions and were assessed before and after the intervention using questionnaires. The results revealed that pelvic muscle exercises led to a significant reduction in urinary incontinence (based on ICIQ scores) and an improvement in self-esteem. The study suggested that such exercise programs could positively impact the quality of life and self-esteem of elderly women with urinary incontinence.
Bø K, et al. conducted a study on pelvic floor muscle exercise for treating female stress urinary incontinence. The study assessed the validity of vaginal pressure measurements for pelvic floor muscle strength and the need for supplemental methods to control correct muscle contraction. Vaginal pressure rise occurred regardless of whether the pelvic floor muscles were contracted correctly or not, indicating that vaginal pressure wasn't specific to pelvic floor muscle contraction. Correct contraction was marked by an inward movement of the vaginal catheter during elevation, a unique characteristic of pelvic floor muscle contraction. The study concluded that measuring vaginal pressure for pelvic floor muscle strength is valid when coupled with observing the catheter's movement. Vaginal pressure due to other muscle contractions wasn't significantly different from that due to intended pelvic floor muscle contraction. The study also addressed EMG activity of lower abdominal muscles during pelvic floor muscle contractions, suggesting that EMG rise occurred even when attempting to relax the abdominal muscles.
Materials and Methods
Study design: Randomized control trial.
Study setting: Tertiary hospitals, Outreach programs, PHC.
Study population: Post-menopausal women.
Study duration: Dec 2022 to June 2023.
Sampling method: Simple random sampling.
Sampling technique: Convenient sampling.
Sample size: 70 (35 in each group).
The estimation of sample size was calculated using G* Power software.
Allocation method: Randomization was done by chit method.
Concealment: SNOSE (sequentially numbered opaque sealed envelope) once the computer software allocates the list of numbers, the numbers were written on the paper and then folded and inserted in an opaque envelope.
Blinding: The researcher was blinded until the randomization.
Ethical clearance: Approval from ethical committee was be obtained before commencing the study.
Inclusion criteria
• Female patients with medical diagnosis of stress urinary incontinence among postmenopausal women.
• Age 45-70 years.
• LMP atleast 12 months ago.
Exclusion criteria
• Anti-incontinence or pelvic organ prolapse surgery history.
• Active urinary tract or vaginal infection.
• Post-partum incontinence issues till 1 year.
• Pregnancy, post-void residual volume >100 ml.
• Pelvic organ prolapses >grade 2.
• Presence of comorbidities that affect the lower urinary tract, such as neurological disease, diabetes mellitus, psychiatric disease or renal failure.
• Current hormone replacement therapy.
• Malignancy.
• Athletes/under specific training.
• MSK/Neurological deficits.
• Recent injuries, fractures in lower limb.
Material used
• Consent forms
• Data collection sheet
• Frequency diary
• ICIQ-SF
• King’s health questionnaire
Procedure
Setting and participants: Subjects were included in the study considering the inclusion and exclusion criteria. The samples were collected from community settings through outreach activities and tertiary hospital. Females who attained menopause and has been diagnosed with stress urinary incontinence in the age of 45-70 years of age participated in the study.
Ethical approval: Ethical approval was obtained from institutional ethics committee. The administration was conducted within a group environment. Participation in the study was voluntary and the participants were not provided with any incentives. The sessions were free of cost.
Before collection of the data, informed written and verbal consent was taken from all the participants (Figure 1).
The subjects were interviewed and the information gathered about their demographic data of patients including name, age, gender, occupation, any history of systemic diseases and medications was documented. Demographic data was collected and 2 evaluations carried out, 1 at the beginning of the treatment and the other after 16 sessions of physical therapy intervention. Also after 1 month till 20th session, follow up was taken.
Treatment protocol
The sessions were conducted individually for each participant in a private room at the outpatient physical therapy department. In the first session, participants were given verbal instructions about the kegels, which should be in the cranial direction and performed without contracting adjacent muscles such as the abdominal muscles, hip adductors, or gluteal muscles.
In both groups, throughout the first few sessions the physical therapist kept 2 fingers inside the participant’s vagina while she performed the exercises for the Kegels Group (KG), to ensure that the contraction is performed correctly.
Participants in both groups were treated twice a week for 8 weeks, and 4 sessions in last month, performing exercises on her own making 20 sessions of physical therapy in total.
Each session lasted approximately 20-30 minutes for the KG group and 30-50 minutes for the Kegels Hip Group (KHG).
The duration of the KG exercises were equal for both groups because they both performed the same sequence of exercises, only additional time was required for KHG.
Control group
Participants were given Kegel’s only in group B. The exercises for strengthening the pelvic floor muscles were given 10 contractions of 5 seconds, 15 contractions of 3 seconds, 20 contractions of 2 seconds, 20 contractions of 1 second (equal rest time between contractions), and 5 repetitions of maximum contractions while coughing (1-minute interval).
The level of difficulty of the exercises throughout the 20 sessions were determined by the patient’s position, starting in a supine position, then progressing to a sitting position and, finally, to a standing position.
These changes in posture were executed partially in five sessions, that is, some of the exercises were done in a new position and the remaining ones in the previous posture.
Changes in posture affect the difficulty of the exercises: The vertical action of gravity on the pelvic floor is absent in the supine position, present in the PFM with weight load partially reduced in the sitting position, and present with total weight load in the standing position. All the patients followed the same protocol (Table 1 and Figures 2-4).
| 1st-5th session | Supine position: 10 contractions of 5 seconds, 15 contractions of 3 seconds, 20 contractions of 2 seconds, 20 contractions of 1 second, 5 contractions while coughing |
| 6th-10th session | Supine position: 10 contractions of 5 seconds, 15 contractions of 3 seconds Sitting position: 20 contractions of 2 seconds, 20 contractions of 1 second, 5 contractions while coughing |
| 11th-15th session | Sitting position: 10 contractions of 5 seconds, 15 contractions of 3 seconds 20 contractions of 2 seconds, 20 contractions of 1 second, 5 contractions while coughing |
| 16th-20th session | Standing position: 10 contractions of 5 seconds, 15 contractions of 3 seconds, 20 contractions of 2 seconds, 20 contractions of 1 second, 5 contractions while coughing |
Table 1: The sequence of exercises for Kegels in relation to change of posture.
Intervention group
Participants were given Hip muscles strengthening along with Kegel’s in group A. The same exercises as those described for the conventional treatment group (Kegels exercises) were performed during the first 20 minutes. After that, the KHG group performed exercises for strengthening hip adductor, gluteus medius and maximus muscles for approximately 20 minutes, completing 40 minutes of session
The exercises for the hip muscles were completely isolated from the Kegels exercises and followed a protocol based on recommendations by the American college of sports medicine, with modifications implemented to suit the profile of the women participating in this study.
In each session, the exercises were only for the hip adductor muscles or only for the gluteal muscles. In the isometric phase of the treatment, only 1 exercise was done for each muscle group.
Four strengthening exercises were selected-2 for the adductor muscles of the hip and 2 for the gluteal muscles:
Gluteus medius exercise. The participant positioned in lateral decubitus, with internal hip rotation, and carried out hip abduction with 90° knee flexion.
Gluteus medius and gluteus maximus exercise. The participant was standing on 1 leg, with the foot on the edge of a 10-inch-high step, and squatted slowly to lower the heel of the other foot toward the floor.
Hip adductor muscles, first exercise. The participant was in lateral decubitus and perform hip adduction movement, maintaining the hip and knee in an extended position.
Hip adductor muscles, second exercise. The participant was in a standing position and perform hip adduction movement to the midline of the body (Figure 5).
In the concentric phase of the treatment, the load for hip exercises was increased every 5 sessions over 4 phases: Isometric exercise without load (20 seconds of contraction, interval of 20 seconds, and ten repetitions), concentric exercise (3 sets of 10 repetitions, 1-minute break between sets) with 1 kg, with 2 kg, and with 3 kg.
In the first session only Kegels were performed because participants learnt how to perform Kegels correctly. All participants followed the same protocol.
This protocol was carried out for 8 weeks till 16th session, after that patient carried out same protocol till 1 month and after that follow up is done (Figures 6-9).
Outcome measures
Symptom and QoL evaluation: Frequency of urinary leakage was assessed by a 3-day voiding diary, which records the number of episodes of UI. For the initial and final assessments, participants were instructed to keep a record for 3 consecutive days. At the beginning of each session, from the first until the last, the data regarding the number of urinary incontinence episodes that has occurred since the previous session and which patients registered in a follow-up voiding diary were collected.
Evaluation of pelvic floor function and muscle strength: Assessment was carried out by bidigital examination (index and middle fingers), according to 2 classifications: The functional evaluation of the pelvic floor (Ortiz scale), which grades the ability of the muscles to contract from 0 to 4, and the perfect scheme (Oxford scale), which quantifies the intensity and number of fast and slow contractions and the duration of sustained contractions.
To evaluate the muscle strength of the pelvic floor, the participant is in supine position with knees bent and feet flat, with legs abducted and externally rotated.
Quality of life was assessed by 2 questionnaires: The International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF) and the King’s Health Questionnaire (KHQ). Both questionnaires were applied in interview format, with the questions read out by the assessor.
The ICIQ-SF evaluates the degree of severity of urinary incontinence. It was developed by Avery et al. and translated and validated.
• It is a self-reported questionnaire and reliable screening tool for urinary incontinence. Out of a total of 6 items, 4 key items inquire about symptom ratings over the past 4 weeks.
• The last item is a self-diagnostic query that does not contribute to the score.
• The first two items (questions) are demographic in nature, collecting information about date of birth and gender. The scores for items 3, 4, and 5 are added up to determine the overall score on the ICIQ-UI SF.
• The scoring scale ranges from 0 to 21, with a lower score indicating less impairment and a higher score indicating more pronounced impairment from incontinence.
The King's Health Questionnaire is utilized to assess the existence of urinary incontinence symptoms and their combined as well as individual influence on an individual's quality of life. The instrument was originally developed by Kelleher et al. KHQ is a valid and reliable instrument for the assessment of quality of life in women with urinary incontinence.
• Useful for the rapid appraisal and follow-up in many clinical trials involving new treatments for urinary incontinence.
• The King's Health Questionnaire is a self-administered self-report tool that comprises three parts, incorporating a total of 21 items.
• Part 1 contains general health perception and incontinence impact (one item each).
• Part 2 contains role limitations, physical limitations, social limitations (two items each), personal relationships, emotions (three items each) and sleep/energy (two items), severity measures (four items).
• In part 3 of the questionnaire, which is treated as a single item, respondents provide ten responses related to various aspects including frequency, nocturia, urgency, urge, stress, incontinence during intercourse, nocturnal enuresis, infections, pain, and challenges with voiding.
The responses in KHQ have four-point rating system. The eight subscales (“domains”) scored between 0 (best) and 100 (worst). The symptom severity scale is scored from 0 (best) to 30 (worst).
• 3 points for the symptom severity scale and 5 points for all other KHQ domains. It is interesting to note that lower scores indicate patient wellbeing and higher scores mean that the person is severely affected by the disease condition.
Statistical analysis
• Data was entered in Microsoft Excel and analyzed using SPSS version 27.0 and GraphPad Prism 7.0 version.
• Mean and SD were calculated for quantitative variables and proportions were calculated for categorical variables.
• For the demographic data, basic descriptive data analysis and interferential statistics using the Chi-Square test, Wilcoxon signed rank test, Mann Whitney U test, student’s paired and unpaired t-test and repeated measures one-way ANOVA were used.
• To evaluate the outcome variable data within groups, a paired t test was utilized and to compare the outcome variable data between the groups, an unpaired t test was utilized,
• Data was represented in the form of visual impressions like bar-diagram etc.
• P value of <0.05 is considered statistically significant.
Results
The present study was conducted to investigate effectiveness of hip muscle strengthening with kegel exercises in treating stress urinary incontinence among postmenopausal women. Figure 1 shows the flow of participants throughout the study. 137 participants were screened for the eligibility out of which 74 participants had to be excluded (not meeting inclusion criteria (n=56), declined to participate (n=9), others (n=08), resulting in 63 participants agreed to participate in this study. They randomized and allocated into two groups (EG n=32); (CG n=31).
During the course of study, total seven participants dropped out from the trail. Four participants could not adhere to the protocol, two participants discontinued due to HRT treatment, one participant met with an accident. At the end of the study period, 63 participants (EG=32 and CG=31) completed the study (Tables 2-5 and Figure 10).
| Age group (yr) | Group A (n=27) | Group B (n=28) | X2 value |
|---|---|---|---|
| 45-54 yrs | 8 (29.63%) | 11 (39.29%) | 0.57 P=0.75, NS |
| 55-64 yrs | 11 (40.74%) | 10 (35.71%) | |
| 65-74 yrs | 8 (29.63%) | 7 (25%) | |
| Total | 27 (100%) | 28 (100%) | |
| Mean ± SD | 58.33 ± 7.92 | 56.89 ± 8 | |
| Range | 45-71 yrs | 45-70 yrs |
Table 2: Distribution of patients in two groups according to their age in year.
| Source | Type III sum of squares | df | Mean square | F | p-value |
|---|---|---|---|---|---|
| Repeated measures ANOVA for group A | |||||
| Intercept | 529 | 1 | 529 | 542.92 | 0.0001,S |
| Error | 25.33 | 26 | 0.97 | ||
| Repeated measures ANOVA for group B | |||||
| Intercept | 893.76 | 1 | 893.76 | 631.08 | 0.0001,S |
| Error | 38.23 | 27 | 1.41 | ||
Table 3: Comparison of frequency in two groups at post treatment and at follow up.
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 6.7 | 27 | 0.86 | 0.16 | - | - |
| Post-test | 0.85 | 27 | 0.86 | 0.16 | 5.85 ± 0.71 | 42.34 |
| P=0.0001, S | ||||||
| Follow up | 0.11 | 27 | 0.32 | 0.06 | 6.59 ± 0.88 | 38.56 |
| P=0.0001, S |
Table 4: Wilcoxon signed rank test for group A.
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 6.71 | 28 | 0.85 | 0.16 | - | - |
| Post-test | 1.85 | 28 | 0.89 | 0.16 | 4.85 ± 0.70 | 36.44, P=0.0001, S |
| Follow up | 1.21 | 28 | 0.62 | 0.11 | 5.50 ± 0.83 | 34.69, P=0.0001, S |
Table 5: Wilcoxon signed rank test for group B.
The final statistical analysis was done with the data obtained from the 63 participants.
This Figure 11 illustrates the comparison of the mean pre, post and follow up test scores obtained from the bladder diary which was used to assess frequency of urine leakage by participants in the experimental group. The mean scores obtained from group A were 6.7, which was reduced to 0.85 post-treatment and was negligible as 0.11 at follow-up, which indicated that the frequency reduced and was extremely significant statistically (P=0.0001) (Tables 4 and 5).
Figure 12 illustrates the comparison of the mean pre, post and follow up test scores obtained from the bladder diary which was used to assess frequency of urine leakage by participants in the control group. The mean scores obtained from group B were 6.71, which was reduced to 1.85 posttreatment and was 1.21 at follow-up, which indicated that the frequency reduced and was extremely significant statistically (P=0.0001) (Table 6).
| Group A | Group B | z-value | |
|---|---|---|---|
| Post-test | 5.85 ± 0.71 | 4.85 ± 0.70 | 5.18, p=0.0001, S |
| Follow up | 6.59 ± 0.88 | 5.50 ± 0.8 | 4.69, p=0.0001, S |
Table 6: Student’s paired t test for group B. Comparison of mean difference in frequency at post-test and at follow up in two groups (Mann Whitney U test).
Figure 13 compares the mean post-test and follow up test scores obtained from both the groups for the frequency of urine leakage. The mean scores obtained from both group were decreased to post-treatment and was further decreased at follow-up, which means that frequency of leakage got reduced significantly. Thus indicated that the group A showed better improvement than group B and was extremely significant statistically (P=0.0001) (Table 7).
| Repeated measures ANOVA for group A | |||||
|---|---|---|---|---|---|
| Source | Type III sum of squares | df | Mean square | F | p-value |
| Intercept | 55486.4 | 1 | 55486.4 | 2819.98 | 0.0001, S |
| Error | 511.58 | 26 | 19.67 | ||
| Repeated measures ANOVA for group B | |||||
| Intercept | 48048.6 | 1 | 48048.6 | 11609.1 | 0.0001, S |
| Error | 111.75 | 27 | 4.13 | ||
Table 7: Comparison of perfect in two groups at post-treatment and at follow up.
Figure 14 illustrates the comparison of the mean pre, post and follow up test scores obtained from the perfect score of participants in the experimental group. The mean scores obtained from group A were 15.85, which was increased to 25.81 post-treatment and was 36.85 at follow-up, which indicated that the score was improved and was extremely significant statistically (P=0.0001) (Tables 8 and 9).
| Mean | N | Std. deviation | Std. error mean | Mean difference | t-value | |
|---|---|---|---|---|---|---|
| Pre-test | 15.85 | 27 | 1.56 | 0.3 | - | - |
| Post-test | 25.81 | 27 | 3.86 | 0.74 | 9.96 ± 3.36 | 15.37, P=0.0001, S |
| Follow up | 36.85 | 27 | 5.24 | 1 | 21 ± 4.84 | 22.52, P=0.0001, S |
Table 8: Student’s paired t test for group A
| Mean | N | Std. deviation | Std. error mean | Mean difference | t-value | |
|---|---|---|---|---|---|---|
| Pre-test | 15.46 | 28 | 1.55 | 0.29 | - | - |
| Post-test | 23.28 | 28 | 1.84 | 0.34 | 7.82 ± 2.07 | 19.95, P=0.0001, S |
| Follow up | 33 | 28 | 2 | 0.37 | 17.53 ± 2.65 | 34.89, P=0.0001, S |
Table 9: Student’s paired t test for group B.
Figure 15 illustrates the comparison of the mean pre, post and follow up test scores obtained from the perfect score of participants in the experimental group. The mean scores obtained from group B were 15.46, which was increased to 23.28 post-treatment and was 33 at follow-up, which indicated that the score was improved and was extremely significant statistically (P=0.0001) as well (Table 10).
| Group A | Group B | t-value | |
|---|---|---|---|
| Post-test | 9.96 ± 3.36 | 7.82 ± 2.07 | 2.85, p=0.006, S |
| Follow up | 21 ± 4.84 | 17.53±2.65 | 3.30, p=0.002, S |
Table 10: Comparison of mean difference in perfect score at post-test and at follow up in two groups (Student’s unpaired t test).
Figure 16 illustrates the comparison of the mean pre, post and follow up test scores obtained from the perfect score of participants in the experimental group. The mean scores obtained from group B were 15.46, which was increased to 23.28 post-treatment and was 33 at follow-up, which indicated that the score was improved and was extremely significant statistically (P=0.0001) as well (Table 11).
| Repeated measures ANOVA for group A | Source | Type III sum of squares | df | Mean square | F | p-value |
|---|---|---|---|---|---|---|
| Intercept | 1081.67 | 1 | 1081.67 | 2059.68 | 0.0001, S | |
| Error | 13.65 | 26 | 0.52 | |||
| Repeated measures ANOVA for group B | ||||||
| Intercept | 1029 | 1 | 1029 | 2525.27 | 0.0001, S | |
| Error | 11 | 27 | 0.4 | |||
Table 11: Comparison of PF Strength in two groups at post treatment and at follow up.
Figure 17 illustrates the comparison of the mean pre, post and follow up test scores obtained from the pelvic floor strength of participants in the experimental group. The mean scores obtained from group A were 2.55, which was increased to 3.74 post-treatment and was 4.6 at follow-up, which indicated that the score was improved and was extremely significant statistically (P=0.0001) (Tables 11 and 12).
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 2.55 | 27 | 0.5 | 0.09 | - | - |
| Post-test | 3.74 | 27 | 0.44 | 0.08 | 1.18 ± 0.39 | 15.55, P=0.0001, S |
| Follow up | 4.66 | 27 | 0.48 | 0.09 | 2.11 ± 0.50 | 21.66, P=0.0001, S |
Table 12: Wilcoxon signed rank test for group A.
Figure 18 illustrates the comparison of the mean pre, post and follow up test scores obtained from the pelvic floor strength of participants in the control group. The mean scores obtained from group B were 2.67, which was increased to 3.67 post-treatment and was 4.14 at follow-up, which indicated that the score was improved and was extremely significant statistically (P=0.0001) as well (Table 13).
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 2.67 | 28 | 0.47 | 0.08 | - | - |
| Post-test | 3.67 | 28 | 0.47 | 0.08 | - | - |
| Follow up | 4.14 | 28 | 0.35 | 0.06 | 1.46 ± 0.50 | 15.25, P=0.0001, S |
Table 13: Wilcoxon signed rank test for group B.
Figure 19 illustrates the mean scores obtained from both group were increased to post-treatment and was further increased at follow-up, which indicated that the group A score was better than group B and was extremely significant statistically (P=0.0001) (Table 14).
| Group A | Group B | z-value | |
|---|---|---|---|
| Post-test | 1.18 ± 0.39 | 1 ± 0 | 2.47, p=0.017, S |
| Follow up | 2.11 ± 0.50 | 1.46 ± 0.50 | 4.72, p=0.0001, S |
Table 14: Comparison of mean difference in PF strength at post-test and at follow up in two groups (Mann Whitney U Test).
Figure 20 illustrates the comparison of the mean pre, post and follow up test scores obtained from the KHQ Score of participants in the experimental group. The mean scores obtained from group A were 52.22, which was reduced to 28.81 post-treatment and was 17.11 at follow-up, which indicated that the score was reduced and quality of life was improved and was extremely significant statistically (P=0.0001) (Tables 15 and 16).
| Repeated measures ANOVA for group A | |||||
|---|---|---|---|---|---|
| Source | Type III sum of squares | df | Mean square | F | p-value |
| Intercept | 86697.5 | 1 | 866.97.53 | 1600.41 | 0.0001, S |
| Error | 1408.46 | 26 | 54.17 | ||
| Repeated measures ANOVA for group B | |||||
| Intercept | 102760 | 1 | 102760 | 321.27 | 0.0001, S |
| Error | 8635.95 | 27 | 319.85 | ||
Table 15: Comparison of KHQ score in two groups at post-treatment and at follow up.
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 52.22 | 27 | 7.57 | 1.45 | - | - |
| Post-test | 28.81 | 27 | 4.62 | 0.89 | 23.40 ± 8.17 | 14.88, P=0.0001, S |
| Follow up | 17.11 | 27 | 5.76 | 1.1 | 35.11 ± 9.43 | 19.33, P=0.0001, S |
Table 16: Student’s paired t test for group A.
Figure 21 illustrates the comparison of the mean pre, post and follow up test scores obtained from the KHQ score of participants in the experimental group. The mean scores obtained from group A were 50.06, which was reduced to 32.28 post-treatment and was 22.03 at follow-up, which indicated that the score was reduced and quality of life was improved and was extremely significant statistically (P=0.0001) as well (Table 17).
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 50.6 | 28 | 11.46 | 2.16 | - | - |
| Post-test | 32.28 | 28 | 11.64 | 2.2 | 18.32 ± 9.14 | 10.60, P=0.0001, S |
| Follow up | 22.03 | 28 | 10.91 | 2.06 | 28.57 ± 9.80 | 15.41, P=0.0001, S |
Table 17: Student’s paired t test for group B.
Figure 22 illustrates the comparison of the mean post and follow up test scores obtained from the KHQ score of participants when compared to each other. The mean scores obtained from both group were increased to post-treatment and was further increased at follow-up, which indicated that the group A score was better than group B and was extremely significant statistically (P=0.0001) (Table 18).
| Group A | Group B | z-value | |
|---|---|---|---|
| Post-test | 23.40 ± 8.17 | 18.32 ± 9.14 | 2.17, p=0.034, S |
| Follow up | 35.11 ± 9.43 | 28.57 ± 9.80 | 2.51, p=0.015, S |
Table 18: Comparison of mean difference in KHQ at post-test and at follow up in two groups (Student’s unpaired t test).
Figure 23 illustrates the comparison of the mean pre, post and follow up test scores obtained from the ICIQSF score of participants in the experimental group. The mean scores obtained from group A were 13.48, which was reduced to 6.03 post-treatment and 2.07 at follow-up, which indicated that the score was reduced and severity of symptoms was reduced and was extremely significant statistically (P=0.0001) (Tables 19 and 20).
| Repeated measures ANOVA for group A | |||||
|---|---|---|---|---|---|
| Source | Type III sum of squares | df | Mean square | F | p-value |
| Intercept | 4196.16 | 1 | 4196.16 | 146.73 | 0.0001, S |
| Error | 743.5 | 26 | 28.59 | ||
| Repeated measures ANOVA for group B | |||||
| Intercept | 7619.04 | 1 | 7619.04 | 261.85 | 0.0001, S |
| Error | 785.61 | 27 | 29.09 | ||
Table 19: Comparison of ICIQSF score in two groups at post treatment and at follow up
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 13.48 | 27 | 4.74 | 0.91 | - | - |
| Post-test | 6.03 | 27 | 3.7 | 0.71 | 7.44 ± 2.50 | 15.46, P=0.0001, S |
| Follow up | 2.07 | 27 | 1.49 | 0.28 | 11.40 ± 3.97 | 14.91, P=0.0001, S |
Table 20: Student’s paired t test for group A
Figure 24 illustrates the comparison of the mean pre, post and follow up test scores obtained from the ICIQSF score of participants in the experimental group. The mean scores obtained from group B were 17, which was reduced to 7.57 post-treatment and 4 at follow-up, which indicated that the score was reduced and severity of symptoms was reduced and was extremely significant statistically (P=0.0001) as well (Table 21).
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 17 | 28 | 3.43 | 0.64 | - | - |
| Post-test | 7.57 | 28 | 4.38 | 0.82 | 9.42 ± 4.55 | 10.96, P=0.0001, S |
| Follow up | 4 | 28 | 3.5 | 0.66 | 13 ± 4.28 | 16.05, P=0.0001, S |
Table 21: Student’s paired t test for group B
Figure 25 illustrates the comparison of the mean post and follow up test scores obtained from the ICIQSF score of participants when compared to each other. The mean scores obtained from both group were increased to post-treatment and was further increased at follow-up, which indicated that the group A score was better than group B and was extremely significant statistically (P=0.0001) (Table 22).
| Mean | N | Std. deviation | Std. error mean | Mean difference | z-value | |
|---|---|---|---|---|---|---|
| Pre-test | 17 | 28 | 3.43 | 0.64 | - | - |
| Post-test | 7.57 | 28 | 4.38 | 0.82 | 9.42 ± 4.55 | 10.96, P=0.0001, S |
| Follow up | 4 | 28 | 3.5 | 0.66 | 13 ± 4.28 | 16.05, P=0.0001, S |
Table 22: Comparison of mean difference in ICIQSF score at post-test and at follow up in two groups (student’s unpaired t test).
So to conclude there was improvement is disease severity as frequency of urine leakage was reduced and went till negligible, strength of pelvic floor muscles was increased along with perfect score. ICIQ SF was taken to see the impact of incontinence which was reduced along with KHQ score which means that quality of life got better in course of time.
Discussion
The current investigation aimed to explore the effectiveness of Kegel exercises in combination with hip muscle strengthening for alleviating Stress Urinary Incontinence (SUI) among postmenopausal women. The findings of the present study demonstrated that a structured regimen of hip muscle strengthening coupled with Kegel exercises, conducted over an 8-week period, effectively enhanced various aspects of SUI, such as frequency of urine leakage, pelvic floor muscle strength, perfect score, Quality of Life (QOL), and incontinence severity. The female pelvic floor serves multiple functions, which makes it susceptible to physiological changes over time that could compromise its structure. These changes might involve damaged fascias, ligaments, peripheral nerves, and impaired Pelvic Floor Muscle (PFM) function. Pelvic floor exercises, a common treatment for SUI, are often employed either alone or in conjunction with therapies like electrotherapy, vaginal cones, biofeedback, or bladder training.
Treatment options encompass pharmacological approaches like hormone replacement therapy and non-pharmacological interventions such as physiotherapy and behavioral therapy. The integration of exercises within conservative therapy prompts contemplation regarding their potential optimization of pelvic floor rehabilitation, considering anatomical and biomechanical considerations. The process of maintaining urinary continence relies on the harmonious coordination among the bladder, urethra, Pelvic Floor Muscles (PFM), and the nervous system [12]. Dysfunctions in this mechanism, intrinsic sphincter deficiency, or defects in PFM, connective tissue, or neural structures can lead to SUI. PFM training is strongly recommended as the primary conservative therapy for SUI [14].
Kegel exercises, a prevalent method for strengthening pelvic floor muscles, represent a noninvasive approach that doesn't involve using vaginal weights or cones. Research generally supports the progressive strengthening effect of Kegel exercises on pelvic muscles. Elders practicing Kegel exercises exhibited enhanced sphincter control and bladder mastery, reduced urine loss during travel to the restroom, and improved muscle functionality for activities like "squeezing" during coughing or sneezing. These exercises aid in tightening the muscles used to interrupt urination, enhancing urethral sphincter control, coordinating bladder continence, and reducing involuntary urine leakage [15, 16].
Women with SUI typically display weaker abductor and external rotator muscles of the hip [17]. While hip muscle synergism could alleviate SUI symptoms, this connection appears linked to postural adjustments like leg crossing rather than a formal rehabilitation program [18]. Hypothetically, hip muscle deficiency could disrupt the normal function of the continence mechanism. Muscles in the urethral wall contract during gluteal and hip adductor muscle contraction, facilitating intrapelvic muscle synergy. Given the involvement of gluteal and hip muscles in daily activities like walking, these muscles stimulate the internal urethral wall's striated muscle.
Studies show that during voluntary PFM contraction, accessory muscles are activated, with abdominal muscle activity often accompanying maximal PFM contraction. Co-activation of Gluteus Muscles (GM) and PFM during striated urethral wall activity has been recorded. While Levator Ani Activation (LAA) reduces during contraction, GM movement is synchronous, influenced by the functional impact of the pelvic floor. The synergistic function of LA and GM is supported by anatomical findings, with multiple connective tissue septa connecting them within the Fossa Ischioanalis (FI).
Conscious contraction of the Pelvic Floor Muscles (PFM) was observed to coincide with simultaneous movement of the Gluteus Maximus (GM) muscles as indicated by functional MRI. This contraction resulted in a decrease in Levator Ani Activation (LAA), a phenomenon similarly noted by Dumoulin, et al. Despite the reduction in LAA while the GM activity increased during this voluntary PFM contraction, the synchronicity of movement in both muscles is due to the functional influence of the Fossa Ischioanalis (FI). These findings support those reported by Christensen, et al., who showed that the GM has also moved markedly in the same direction as the LA by voluntary PFM contraction. The differences in co-activation in MRI versus s-EMG may occur due to image selection with a small muscle area on it. 3-D real-time sequences of the PFM would be an asset for the future [19]. Studying anatomical sections De Block et al showed the existence of multiple connective tissue septa within the Fossa Ischioanalis (FI) connecting the LA and GM.
Moreover, our functional results support these anatomical findings showing synergistic LA and GM function which occurred simultaneously with synchronous changes of the FIA. Furthermore, our findings indicate that isolated contraction of the LA does not occur in assumed physiological voluntary pelvic floor contraction in healthy female volunteers. Conversely, the additional simultaneous co-contraction of the Gluteus Maximus (GM) appears to be a natural component of voluntary Pelvic Floor Muscle (PFM) contraction, due to the LA and GM interaction with functional and morphological connections via the FI. Co-contraction of the GM is a result of direct functional and morphological connections to the LA via the FI. This different mechanism of GM co-contraction needs to be further evaluated concerning the clinical outcome of additional GM activities for PFM training.
The study suggests that isolated LA contraction doesn't occur in typical physiological voluntary pelvic floor contraction, contrary to the synchronous co-contraction of GM. Marques et al in a particular study combined the strengthening of Pelvic Floor Muscles (PFM) with the simultaneous strengthening of hip synergistic muscles led to improved outcomes in terms of the frequency of daily urine loss across the sessions, although there was no accompanying superiority in the improvement of strength, perineometer, or QoL over the group that performed only PFM strengthening exercises.
Chow, et al. demonstrated that anxiety and depression in affected women stemmed from stress urinary incontinence. Furthermore, the severity of stress urinary incontinence symptoms correlated with a more pronounced negative impact on both physical and mental dimensions of health-related quality of life. Their analyses also indicated that stress urinary incontinence tended to detrimentally influence work productivity. Despite these adverse effects, a significant number of women with stress urinary incontinence do not actively seek behavioural counselling or medical interventions that could potentially improve their condition, particularly concerning role limitation and physical/social restrictions. Combined training involving Pelvic Floor Muscles (PFM) and the synergistic muscle, as well as isolated PFM exercises, exhibit the ability to enhance the quality of life for women with Stress Urinary Incontinence (SUI).
The pelvic floor has a crucial role within the body's core structure. Additionally, it engages the underlying abdominal and back muscles. Consequently, this group of muscles collaboratively offers assistance, vigor, and steadiness to both the spine and the inner organs while the body is in motion. When the core muscles are reinforced or made robust, they contribute to sustaining the pelvic organs and aiding in the management of potential leaks. This action has the potential to decrease or remove Urinary Incontinence (UI). Enhancing the strength of the core muscles can lead to a reduction in UI, facilitating the control of any leakage.
As a result of this, all the outcomes related to stress urinary incontinence are displaying favourable results, leading to an improved perfect score [20, 21]. The perfect score assesses the intensity and quantity of both rapid and slow contractions, along with the duration of sustained contractions. Enhancing the Pelvic Floor Muscles (PFM) in conjunction with the synergic muscles of the hips yielded more positive outcomes concerning the frequency of daily urine leakage throughout the sessions. There was improvement in both groups, however, there was no accompanying superiority observed in terms of strength improvement, perineometry (measurement of pelvic floor muscle strength), or quality of life when compared to the group exclusively focusing on PFM strengthening exercises.
The present study illustrates that following a routine of exercises targeting both the pelvic floor and hip muscles can alleviate the severity of symptoms, decrease the frequency of stress urinary incontinence episodes, improve pelvic floor function, and augment the strength of both pelvic and hip muscles. This approach proves to be more effective than the group that only engaged in graded Kegel exercises in various positions. Ultimately, this intervention contributes to heightened muscular strength, an improved quality of life for postmenopausal women managing stress urinary incontinence, and the potential to prevent further deterioration.
Summary
The current study aimed to determine the effect of hip muscles strengthening with Kegels exercise in treatment of stress urinary incontinence among postmenopausal women. 63 participants participated in this study, they were randomized and allocated into two groups (EG n=32); (CG n=31).
Group A which was the intervention group was given structured hip muscles strengthening exercises and Kegels and group B was given only structured Kegels exercises. Demographic data was collected and 3 evaluations carried out, 1 at the beginning of the treatment and the other after 16 sessions of physical therapy intervention. Also after 1 month till 20th session, follow-up was taken. The outcome measures were frequency of urinary leakage, the strength of pelvic floor muscles, perfect score, incontinence impact was seen with ICIQ SF and quality of life was assessed with King’s health questionnaire. Both scales were valid and reliable assessment tool.
Participation in structured hip muscles strengthening exercises with Kegels in postmenopausal women experiencing stress urinary incontinence witnessed noteworthy enhancements through the intervention. These enhancements exceeded the outcomes attained by solely practicing Kegel exercises. They encompassed various aspects including leakage frequency, pelvic floor strength, perfect score, symptom severity, and quality of life. Additionally, the effects were observed to be long-lasting.
Conclusion
The results of the present study indicated that combining Kegel exercises in different positions with hip muscle strengthening for postmenopausal women suffering from stress urinary incontinence led to significant improvements. These improvements surpassed those achieved by Kegel exercises alone and encompassed factors such as frequency of leakage, pelvic floor strength, perfect score, symptom severity, and quality of life and has long term effect.
This combined approach not only aids in decreasing the impact of incontinence but also plays a role in preventing the progression of the condition over time. As the quality of life improves, it concurrently enhances the confidence of these women. This is particularly significant for individuals who previously dealt with feelings of awkwardness, anxiety, and discomfort, all of which previously had negative effects on their psychological and social well-being.
Limitations
- The patient’s daily physical activities or at-home rehabilitation was not monitored
- No objective assessments such as the measurement of pelvic floor muscle strength, pad test, perineal ultrasound, or urodynamic study.
- Another limitation was the participants' activity levels, as some were homemakers with a relatively more sedentary lifestyle than others who were working earlier and had mild to moderate physical activity.
Future Scope of Study
- Conducting the study with a larger sample size could provide more comprehensive insights.
- The study could be extended to women with higher BMIs to assess its applicability across different body types.
- Incorporating a multimodal evaluation, where EMG and MRI can be included and other factors such as perception of symptoms and psychosocial characteristics, would enhance the study's depth.
- Exploring females from various socioeconomic statuses with distinct aging consequences due to occupational factors could yield valuable information.
- A comparative study on housewives and in working women can be done.
- The study could explore the combination of different physiotherapeutic approaches, electrotherapy modalities, or aids for a more holistic treatment approach.
Clinical Implications
- Scientific evidence gives the importance of isolated Pelvic Floor Muscle (PFM) contractions and emphasizes the significance of specific exercises for hip muscles. Strengthening hip muscles ensures proper coordination with PFM, crucial for functionality and urinary continence. Including gluteus and hip adductor exercises in physical therapy is advisable for managing stress urinary incontinence.
- When hip muscles strengthening exercises are performed along with pelvic floor exercises in progression for 8 weeks it reduces the symptoms of stress urinary incontinence which reduces the frequency of urine leakage, improves their pelvic floor muscles strength along with their perfect score, the impact of SUI in their life is reduced and hence their QOL has improved with lasting effects till 1 month.
References
- Traub ML, Santoro N. Reproductive aging and its consequences for general health. Ann N Y Acad Sci. 2010;1204:179-187.
[Crossref] [Google Scholar] [PubMed]
- Deecher DC. Physiology of thermoregulatory dysfunction and current approaches to the treatment of vasomotor symptoms. Expert Opin Investig Drugs. 2005;14:435-448.
[Crossref] [Google Scholar] [PubMed]
- Singh U, Agarwal P, Verma ML, Dalela D, Singh N, et al. Prevalence and risk factors of urinary incontinence in Indian women: A hospital-based survey. Indian J Urol. 2013;29:31-36.
[Crossref] [Google Scholar] [PubMed]
- Portman DJ, Gass ML. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and the North American Menopause Society. J Sex Med. 2014;11:2865-2872.
[Crossref] [Google Scholar] [PubMed]
- Sturdee DW, Panay NA. Recommendations for the management of postmenopausal vaginal atrophy. Climacteric. 2010;13:509-522.
[Crossref] [Google Scholar] [PubMed]
- Bozkurt N, Ozkan S, Korucuoglu U, Onan A, Aksakal N, et al. Urogenital symptoms of postmenopausal women in Turkey. Menopause. 2007;14:150-156.
[Crossref] [Google Scholar] [PubMed]
- Huang AJ, Luft J, Grady D, Kuppermann M. The day-to-day impact of urogenital aging: Perspectives from racially/ethnically diverse women. J Gen Intern Med. 2010;25:45-51.
[Crossref] [Google Scholar] [PubMed]
- Dasgupta D, Ray S. Vasomotor and urogenital problems at midlife: A study on rural and urban women in India. Ann Hum Biol. 2015;42:270-277.
[Crossref] [Google Scholar] [PubMed]
- Patni R. Genitourinary syndrome of menopause. J Mid-life Health. 2019;10:111-113.
- Janssen CC, Lagroâ?Janssen AL, Felling AJ. The effects of physiotherapy for female urinary incontinence: Individual compared with group treatment. BJU Int. 2001;87:201-206.
[Crossref] [Google Scholar] [PubMed]
- Dumoulin C, Hayâ?Smith J, Habéeâ?Séguin GM, Mercier J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane systematic review with metaâ?analysis. Neurourol Urodyn. 2015;34:300-308.
[Crossref] [Google Scholar] [PubMed]
- Verghese T, Latthe P. Recent status of the treatment of stress urinary incontinence. Int J Urol. 2014;21:25-31.
[Crossref] [Google Scholar] [PubMed]
- Bo K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol urodyn. 1994;13:35-41.
[Crossref] [Google Scholar] [PubMed]
- Soljanik I, Janssen U, May F, Fritsch H, Stief CG, et al. Functional interactions between the fossa ischioanalis, levator ani and gluteus maximus muscles of the female pelvic floor: A prospective study in nulliparous women. Arch Gynecol Obstet. 2012;286:931-938.
[Crossref] [Google Scholar] [PubMed]
- Park SH, Kang CB. Effect of Kegel exercises on the management of female stress urinary incontinence: A systematic review of randomized controlled trials. Adv Nurs. 2014;2014:1-10.
- McLean L, Varette K, Gentilcoreâ?Saulnier E, Harvey MA, Baker K, et al. Pelvic floor muscle training in women with stress urinary incontinence causes hypertrophy of the urethral sphincters and reduces bladder neck mobility during coughing. Neurourol Urodyn. 2013;32:1096-1102.
[Crossref] [Google Scholar] [PubMed]
- Underwood D, Calteaux T, Cranston A, Novotny S, Hollman J. An examination of isometric hip muscle strength in women with and without stress urinary incontinence: A case-control study. Int Urogynecol J. 2011;22(suppl 2):S964.
- Norton PA, Baker JE. Postural changes can reduce leakage in women with stress urinary incontinence. Obstet Gynecol. 1994;84:770-774.
[Google Scholar] [PubMed]
- Hajebrahimi S, Nourizadeh D, Hamedani R, Pezeshki MZ. Validity and reliability of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form and its correlation with urodynamic findings. Urology J. 2012;9:685-690.
[Crossref] [Google Scholar] [PubMed]
- Margolis MK, Vats V, Coyne KS, Kelleher C. Establishing the content validity of the King’s Health Questionnaire in men and women with overactive bladder in the US. Patient. 2011;4:177-187.
[Crossref] [Google Scholar] [PubMed]
- Allen RE, Hosker GL, Smith AR, Warrell DW. Pelvic floor damage and childbirth: A neurophysiological study. Br J Obstet Gynaecol. 1990;97:770-779.

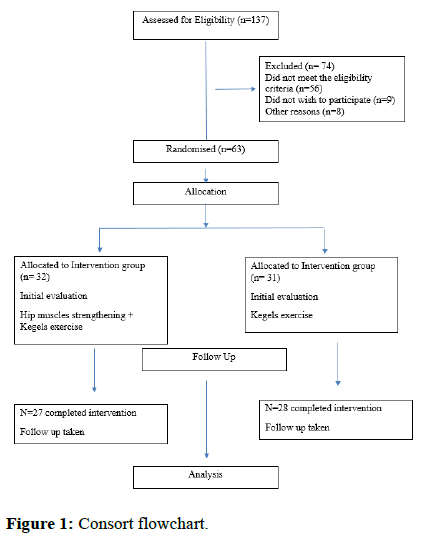
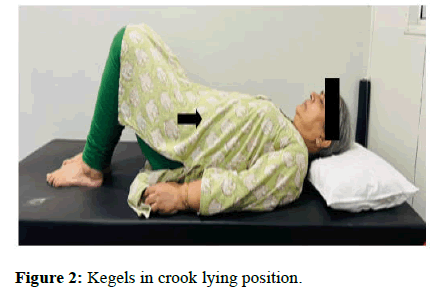

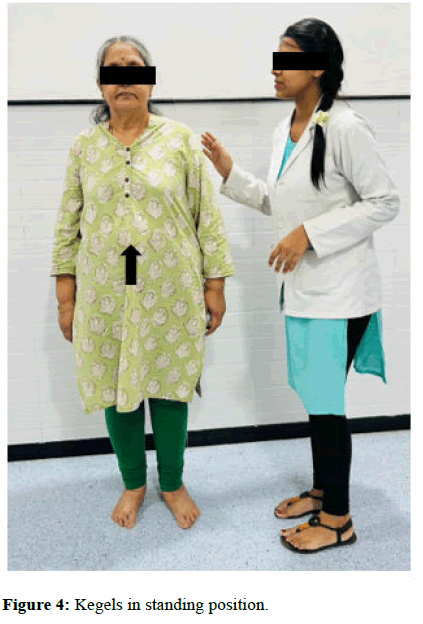
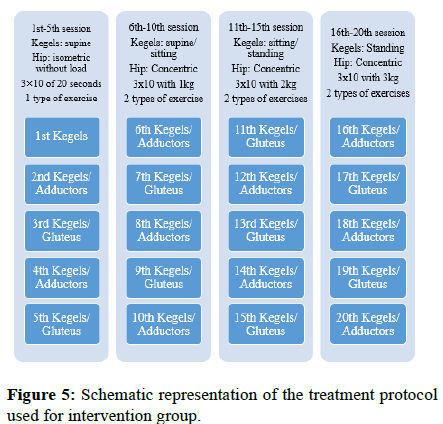
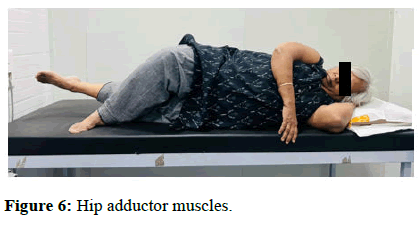

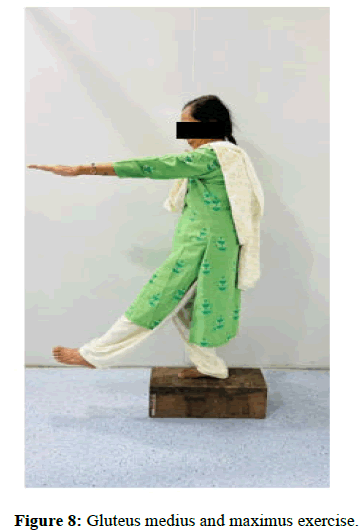
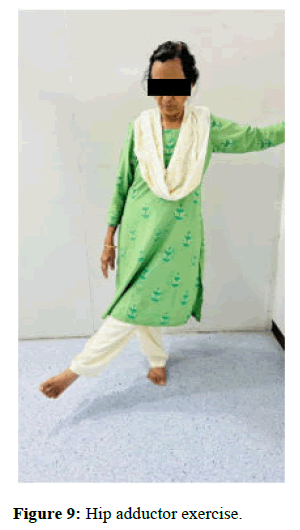

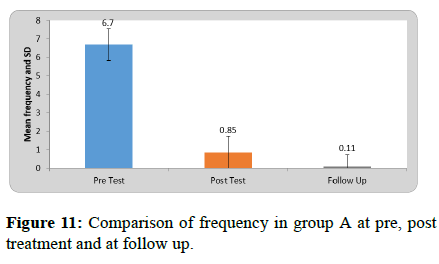
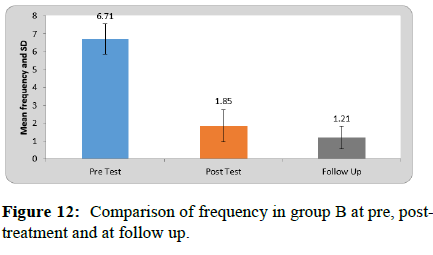
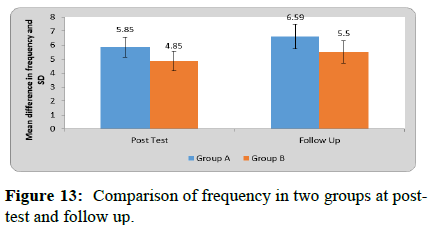

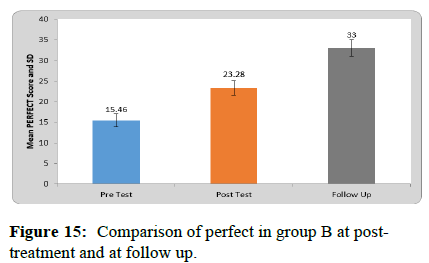
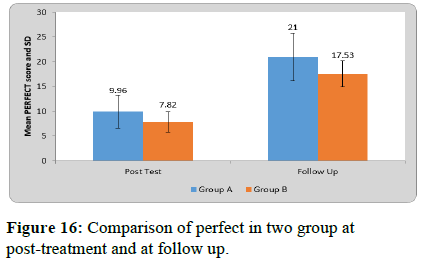
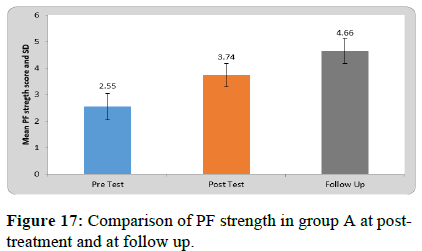
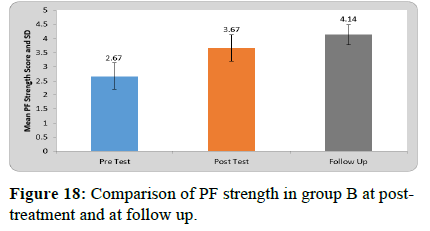
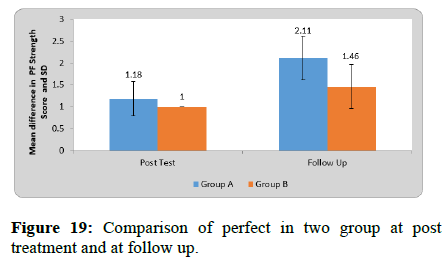
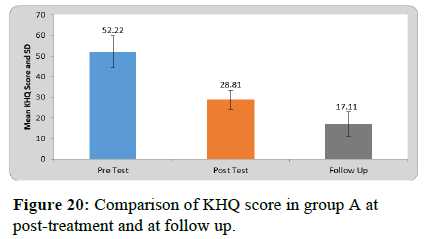

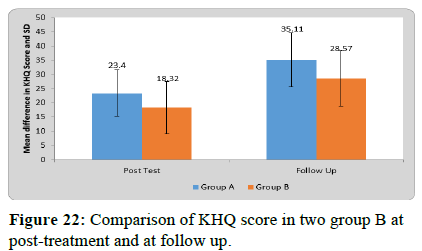
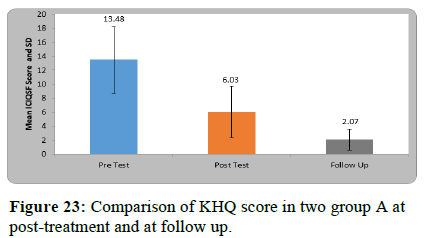
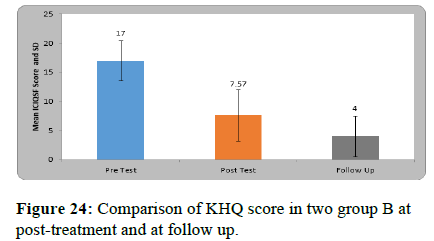
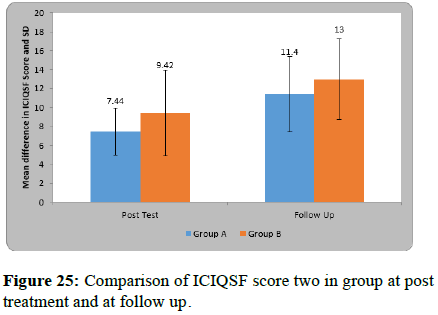



 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.