Al-Anoud Farraj Al Al-Shaikh1*, Abdullah Dakhel Al-Rashod2, Dhafer Ali Al-Amri2, Omar Mohammed Al-Ghamdi2, Othman Mohammed Al-Shahrani2, Fawzia Saeed Al-Asmari3, Reem Rizqallah Al-Johani1, Shoaa Khal-Id Al-Dhahri4, Abdullah Mohammed Hakami1 and Wafaa Mohammed Al-Elyani1
1Department of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
2Department of Medicine, Imam Abulrahman Bin Faisal University, Dammam, Saudi Arabia
3Department of Medicine, King Khalid University, Abha, Saudi Arabia
4Resident at Ministry of Health, Jeddah, Saudi Arabia
- *Corresponding Author:
- Al-Anoud Farraj Al Al-Shaikh
Department of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
Tel: (++381)-21-450-188
Fax: (++381)-21-450-199
E-mail: Dr.alanoud.f.s@gmail.com
Citation: Al Al-Shaikh AF, et al. Efficacy of Oral Anticoagulants (Warfarin) in End-Stage Renal Disease Patients with Atrial Fibrillation: Systematic Review and Meta-analysis.
Ann Med Health Sci Res. 2020;10 954-958.
Abstract
Background: Warfarin stays a commonly used anticoagulant in the setting of EndStage Renal Disease (ESRD) and Atrial Fibrillation (AF). Research has investigated the effectiveness of warfarin in preventing ischemic strokes in ESRD and AF. They found that no randomized clinical trials have tested the function of warfarin, and periodically performed meta-analyses provided irrelevant results. Aim: This work aims to determine the efficacy of oral anticoagulants (Warfarin) in End-Stage Renal Disease (ESRD) patients with Atrial Fibrillation (AF). Materials and Methods: A systematic search was performed over different medical databases to identify Internal Medicine studies, which studied the outcome of Patients receiving Warfarin versus Patients not receiving Warfarin of ESRD patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on, the incidence of ischemic strokes, and incidence of hemorrhagic stroke (as primary outcomes), and incidence of major bleeding and mortality rate (as secondary outcomes). Results: Six studies were identified involving 48737 patients, 16255 patients receiving Warfarin, and 32482 patients not receiving Warfarin. The meta-analysis process revealed that all outcome measures (ischemic and hemorrhagic strokes, major bleeding, along with mortality rates), exhibited non-significant differences if Warfarin administered or not (p>0.05 respectively). Conclusion: To conclude, Warfarin use appears to have been associated with no change in the incidence of ischemic stroke in patients with atrial fibrillation and end-stage renal disease. However, from the studies reviewed, it does appear to be associated with a significantly higher risk of hemorrhagic stroke, with no significant difference in the risk of major bleeding, and with no change in mortality.
Keywords
Oral anticoagulants; Warfarin; Atrial fibrillation; Dialysis
Introduction
Atrial fibrillation is the commonest cardiac form of arrhythmia
and is related to a heightened hazard of ischemic stroke. In
comparison with the general population, patients who acquire
maintenance dialysis have a 6-fold higher hazard of atrial
fibrillation, and a 5- to 10-fold higher hazard of ischemic
stroke. This results from uremia-related cardiovascular risk
factors for cerebral thrombosis that are highly prevalent in
dialysis patients. Nonetheless, there is a paucity of evidence on
strategies for stroke prevention between dialysis recipients with
atrial fibrillation. [1]
The prevalence of AF in adults with an ESRD is 11.6%,
approximately 11-times higher than the prevalence of AF in
the general person population. Between patients with ESRD
and AF, the stroke incidence is 5.2/100 person-years and the
mortality prevalence is 26.9/100 person-years. Those incidences
are higher than stroke prevalence (1.9 per a hundred person-years) and the prevalence of mortality (13.4 per 100 personyears)
in patients with ESRD who do not have AF. [2]
In general, warfarin use has been observed to be rather low in
hemodialysis patients with AF. In a study of old hemodialysis
sufferers with AF, only 1 quarter had a Warfarin prescription in
a 45-day interval. 26% of American hemodialysis patients with
AF were on warfarin therapy. They did not specify the indication
for warfarin use (AF or other, e.g., vascular occlusion) or the
level of anticoagulation achieved. Of 1671 patients who had
preexisting AF and initiated hemodialysis with a big national dialysis provider 45% had been reported to have acquired
warfarin at dialysis initiation. [3]
Warfarin stays a commonly used anticoagulant in the setting of
ESRD. Research has investigated the effectiveness of warfarin
in preventing ischemic strokes in ESRD and AF. They found
that no randomized clinical trials have tested the function of
warfarin in ESRD and AF, and periodically performed metaanalyses
provided irrelevant results. This inconsistency has
even prevailed in the recommendations from various societies.
where the American coronary heart association/American
College of Cardiology guideline recommends anticoagulation
in patients with ESRD and AF, the European Cardiovascular
Society guideline emphasizes the lack of proof for such a
recommendation, and the Kidney disease: improving worldwide
Outcomes guideline recommends against the usage of warfarin
in such conditions. [4] This work aims to determine the efficacy
of oral anticoagulants (Warfarin) in End-Stage Renal Disease
(ESRD) patients with Atrial Fibrillation (AF).
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published
article, and a human study describing ESRD patients with AF
patients. The excluded studies were non-English, or animal
studies or describing ESRD patients, without AF, or not on
dialysis program.
Study identification
Basic searching was done over the PubMed, Cochrane library,
and Google scholar using the following keywords: Oral
Anticoagulants, Warfarin, Atrial Fibrillation, and Dialysis.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of Patients receiving Warfarin versus Patients not
receiving Warfarin of ESRD patients with AF patients, will
be reviewed. Outcome measures included the incidence of
ischemic strokes, and the incidence of hemorrhagic stroke (as
primary outcomes), and the incidence of major bleeding and
mortality rate (as secondary outcomes).
Study selection
We found 244 records, 195 excluded based on title and abstract
review; 49 articles are searched for eligibility by full-text
review; 13 articles cannot be accessed; 10 studies were reviews
and case reports; 11 were not describing our outcomes; the
desired anticoagulant not administered in 9 studies leaving 6
studies that met all inclusion criteria.
Statistical methodology
The pooling of data, odds ratios (ORs), with 95% confidence
intervals (CI) were done, using MedCalc ver. 18.11.3 (MedCalc,
Belgium). According to heterogeneity across trials using the I2-
statistics; a fixed-effects model or random-effects model were
used in the meta-analysis process.
Results
The included studies published between 2011 and 2020.
Regarding the type of included studies, all 6 studies were
retrospective [Table 1]. Regarding patients’ characteristics, the
total number of patients in all the included studies was 48737
patients, 16255 patients receiving Warfarin and 32482 patients
not receiving Warfarin, while their average follow-up time was
(2.8 years), and mean age of all patients was (69.6 years) [Table
1]. [6-11]
| Table 1: Patients and study characteristics. |
| N |
Author |
Type of study |
Total |
Number of patients |
Age (average years) |
Follow-up time (average years) |
| Patients receiving Warfarin |
Patients not receiving Warfarin |
| 1 |
Winkelmayer et al. [6] |
Retrospective |
2313 |
249 |
2064 |
69 |
1.76 |
| 2 |
Shen et al. [7] |
Retrospective |
12284 |
1838 |
10446 |
61 |
- |
| 3 |
Kai et al. [8] |
Retrospective |
4286 |
989 |
3297 |
68 |
2.1 |
| 4 |
Lee et al. [9] |
Retrospective |
2356 |
589 |
1767 |
70 |
2 |
| 5 |
Tan et al. [10] |
Retrospective |
5765 |
1651 |
4114 |
74 |
5 |
| 6 |
Makani et al. [11] |
Retrospective |
21733 |
10939 |
10794 |
75.5 |
3.4 |
A meta-analysis study was done on 6 studies that described and
compared the 2 different groups of patients: with an overall
number of patients (N=48737) [Table 2]. [6-11]
| Table 2: Summary of outcome measures in all studies. |
| N |
Author |
Primary outcomes |
Secondary outcomes |
| Ischemic stroke |
Hemorrhagic stroke |
Major bleeding |
Mortality |
| Warfarin |
Control |
Warfarin |
Control |
Warfarin |
Control |
Warfarin |
Control |
| 1 |
Winkelmayer et al. [6] |
29 |
135 |
11 |
46 |
48 |
215 |
181 |
750 |
| 2 |
Shen et al. [7] |
62 |
501 |
29 |
188 |
153 |
888 |
831 |
4596 |
| 3 |
Kai et al. [8] |
67 |
304 |
2 |
45 |
126 |
368 |
495 |
1813 |
| 4 |
Lee et al. [9] |
48 |
51 |
6 |
35 |
- |
- |
340 |
1050 |
| 5 |
Tan et al. [10] |
93 |
644 |
- |
- |
407 |
1559 |
476 |
3349 |
| 6 |
Makani et al. [11] |
1640 |
1720 |
98 |
78 |
1295 |
1512 |
613 |
133 |
Each outcome was measured by:
• Odds Ratio (OR) for:
a) Incidence of ischemic strokes.
b) Incidence of hemorrhagic strokes.
c) Incidence of major bleeding.
d) Mortality rate.
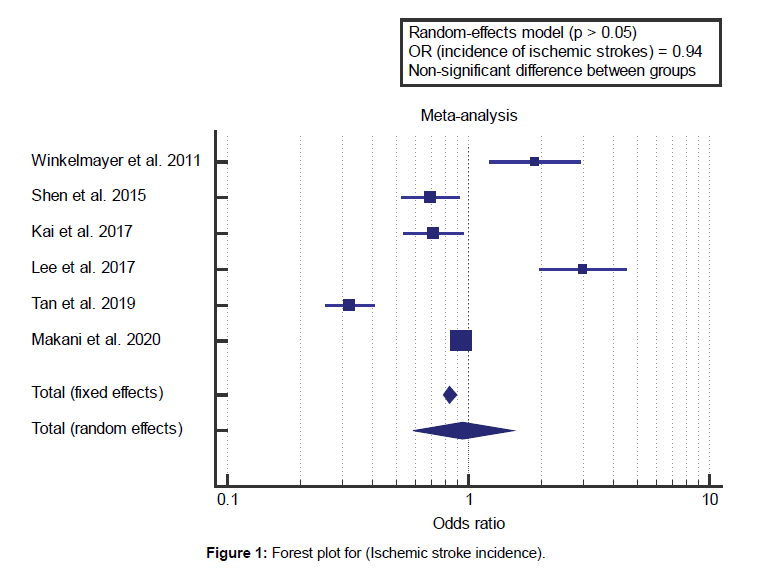
Concerning the primary outcome measures, we found 6 studies
reported the incidence of ischemic strokes with a total number
of patients (N=48737). I2 (inconsistency) was 96% with highly
significant Q test for heterogeneity (p<0.0001), so randomeffects
model was carried out; with overall OR=0.94 (95% CI
0.588 to 1.527).
Using the random-effects model, the meta-analysis process
revealed a non-significant difference in the incidence of
ischemic strokes in Patients receiving Warfarin compared to
Patients not receiving Warfarin (p=0.825) [Figure 1]. We found
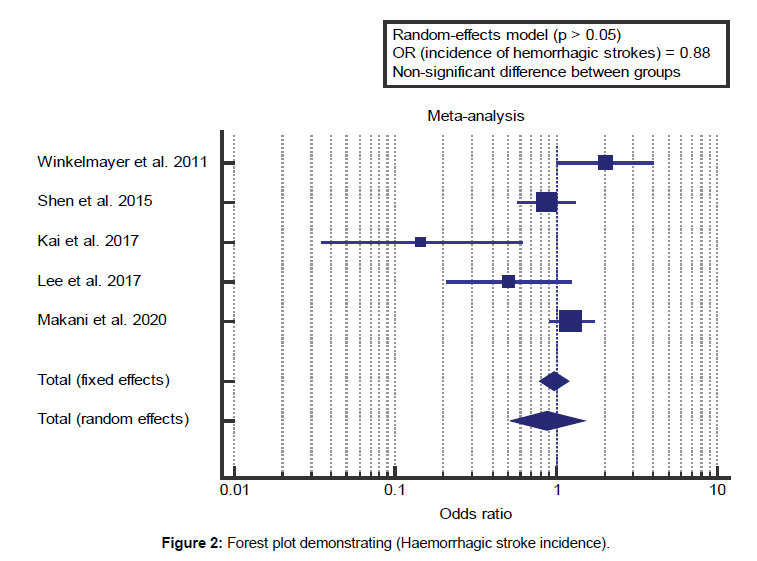
5 studies reported the incidence of hemorrhagic strokes with a
total number of patients (N=42972).
I2 (inconsistency) was 75% with highly significant Q test for
heterogeneity (p=0.0025), so random-effects model was carried
out; with overall OR=0.88 (95% CI 0.522 to 1.493). Using
the random-effects model, the meta-analysis process revealed
a non-significant difference in the incidence of hemorrhagic
strokes in Patients receiving Warfarin compared to Patients not
receiving Warfarin (p=0.642) [Figure 2].
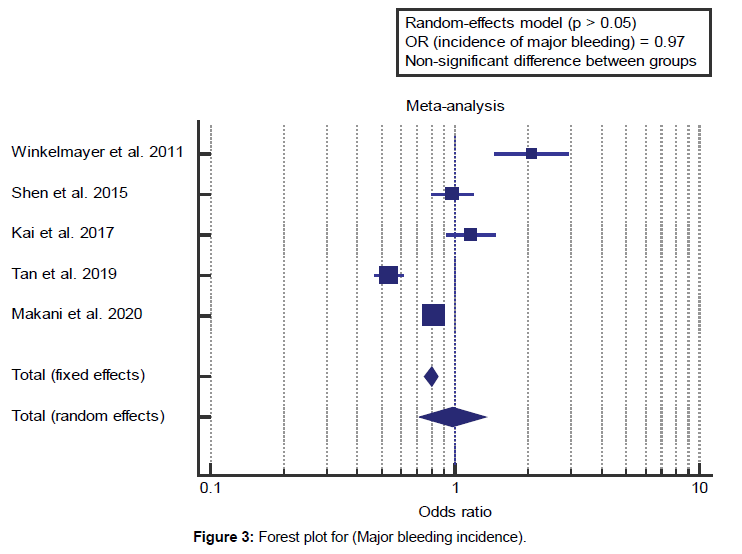
Concerning the secondary outcome measures, we found 5
studies reported the incidence of major bleeding with a total number of patients (N=46381). I2 (inconsistency) was 95%
with highly significant Q test for heterogeneity (p<0.0001), so
random-effects model was carried out; with overall OR=0.97
(95% CI 0.712 to 1.340). Using the random-effects model, the
meta-analysis process revealed a non-significant difference
in the incidence of major bleeding in Patients receiving
Warfarin compared to Patients not receiving Warfarin
(p=0.886) [Figure 3].
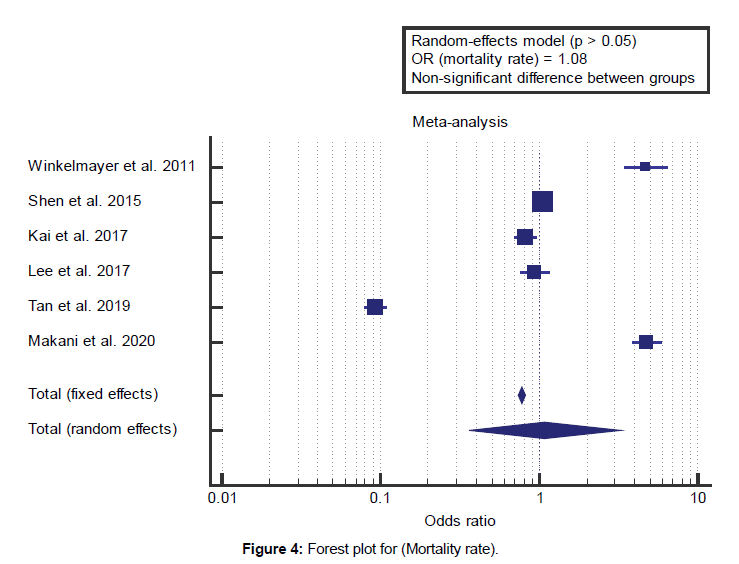
We found 6 studies reported mortality rates with a total
number of patients (N=48737). I2 (inconsistency) was 99.6%
with highly significant Q test for heterogeneity (p<0.0001), so
random-effects model was carried out; with overall OR=1.08
(95% CI 0.361 to 3.256). Using the random-effects model, the
meta-analysis process revealed a non-significant difference
in mortality rate in Patients receiving Warfarin compared to
Patients not receiving Warfarin (p=0.886) [Figure 4].
Discussion
This work aims to determine the efficacy of oral anticoagulants
(Warfarin) in End-Stage Renal Disease (ESRD) patients
with Atrial Fibrillation (AF). The included studies published
between 2011 and 2020. Regarding the type of included
studies, all 6 studies were retrospective. Regarding patients’
characteristics, the total number of patients in all the included
studies was 48737 patients, 16255 patients receiving Warfarin,
and 32482 patients not receiving Warfarin, while their average
follow-up time was (2.8 years), and mean age of all patients
was (69.6 years). A meta-analysis study was done on 6 studies
that described and compared the 2 different groups of patients:
with an overall number of patients (N=48737). Concerning the
primary outcome measures, we found 6 studies reported the incidence of ischemic strokes with a total number of patients
(N=48737).
The meta-analysis process revealed a non-significant difference
in the incidence of ischemic strokes in patients receiving Warfarin
compared to patients not receiving Warfarin (p=0.825). We
found 5 studies reported the incidence of hemorrhagic strokes with a total number of patients (N=42972). The meta-analysis
process revealed a non-significant difference in the incidence of
hemorrhagic strokes in Patients receiving Warfarin compared
to Patients not receiving Warfarin (p=0.642), which came in
agreement with Harel et al. [1] Randhawa et al. [4] Belley-Cote
and Eikelboom [12] and Sarratt, Nesbit, and Moye. [13]
Harel et al. reported that all research (n=20,398 members)
mentioned at the outcome of ischemic stroke or systemic
thromboembolism. Warfarin was not associated with ischemic
stroke or thromboembolism (HR, 0.77). In four research
comprised of 15,726 members, hemorrhagic stroke/intracranial
hemorrhage was not associated with warfarin (HR, 1.93). In
the three studies (n=14,693) that mentioned the outcome of
gastrointestinal bleeding, warfarin was not associated with a
higher risk of gastrointestinal bleeding. [1]
Randhawa et al. reported that (22%) of patients were taking
warfarin, with a mean (SD) follow-up period of 2.6 (1.4) years.
Warfarin use was related to no great alternate for the hazard of
ischemic stroke (HR, 0.96), with a significantly higher hazard
of hemorrhagic stroke (HR, 1.49), with no significant difference
in the hazard of major bleeding (HR, 1.20). [4] Belley-Cote and
Eikelboom reported that, the outcomes of an up to date metaanalysis
of 15 observational research reporting the outcomes of
47 480 patients with atrial fibrillation (AF) and end-level renal
disorder (ESRD) according to whether or not or not they have
been treated with warfarin. Patients treated with warfarin (10
445 [22.0%]), compared with those not treated with warfarin,
had similar rates of ischemic stroke (7.7% vs. 7.1%; risk ratio
[HR], 0.96), major bleeding (16.1% vs. 15%; HR, 1.20). [12]
Sarratt, Nesbit, and Moye reported that a total of 160 patients
(warfarin group, n=120; apixaban group, n=40). There have been
7 major bleeding events in the warfarin group in comparison
with 0 in the apixaban group (p=0.34). There had been similar
rates of clinically relevant non major bleeding activities (12.5%
vs. 5.8%, p=0.17) and minor bleeding (2.5% vs. 2.5%, p=0.74)
events in patients receiving apixaban and warfarin. [13]
Our result came in disagreement with Pilote. [14] Pilote conducted
a study on 1,626 dialysis patients and 204,210 non-dialysis
patients. Amongst dialysis patients, 46% had been prescribed
warfarin. Between dialysis patients, warfarin users had more
congestive coronary heart failure and diabetes however much
less prior bleeding event as compared to controls. Warfarin use
was not associated with a decrease hazard for stroke (HR: 1.14)
but became associated with a 44% higher risk for bleeding (HR:
1.44) after adjusting for potential confounders. [14]
Concerning the secondary outcome measures, we found 5
studies reported the incidence of major bleeding with a total
number of patients (N=46381). The meta-analysis process
revealed a non-significant difference in mortality rate in Patients
receiving Warfarin compared to Patients not receiving Warfarin
(p=0.886), which came in agreement with Belley-Cote and
Eikelboom, [12] Randhawa et al. [4] Wang et al. [15] Winkelmayer
et al. [6] and Harel et al. [1] Belley-Cote and Eikelboom reported
that they believe that the net harm should discourage the
warfarin use. Different sobering findings revealed that patients
with ESRD have a high rates of major bleeding (about 15%),
which, even in the absence of warfarin therapy, had been double
those of ischemic stroke, and mortality rates of 40% to 50%. [12]
Randhawa et al. 2020 reported that, among 29623 patients,
6090 patients (20.6%) who received Warfarin. The mortality
rate was 43.4% for warfarin users and 52.5% for warfarin nonusers,
with an overall HR of 0.95. This recommends that overall
mortality does not appear to be associated with anticoagulation
for those patients. [4]
Wang et al. reported that there have been 141 out of 774 (18.2%)
dialysis patients with AF followed-up for 4.4 ± 2.5 years, and 41.8% (59) have been on warfarin. Incidence of all embolic
events, ischemic stroke, and all bleeding and an intracranial
bleed have been four.1, 3.1, 9.6, and 0.82/100 person-years,
respectively. Warfarin anticoagulation was associated with
an increased hazard of intracranial bleed (hazards ratio=11.1,
p=0.038), however now not total embolic, bleeding events, or
mortality during follow-up (p=0.317-0.980). [15]
Harel et al. reported that, overall, 1490 citations met the search
criteria. After excluding 279 duplicate citations, 1211 citations
were evaluated, of which 32 were reviewed in detail. They
subsequently excluded 17 research due to the fact they consisted
of systematic or narrative reviews (n=5), did not contain
information on our outcomes of interest (n=4), contained
missing information that could not be obtained from the authors
(n=6), or constituted case collection (n=2). All-cause mortality
(reported in 7 studies; n=16,172) was not associated with
receipt of warfarin (HR, 0.89; I2=79%. [1] Our result came in
disagreement with Shen et al. [7]
Shen et al. reported that, in their study of a large cohort of
patients on hemodialysis therapy with newly diagnosed AF, they
observed that only 15% of patients initiated warfarin use within
30 days of the index AF event; only 11% of patients without an
initially filled warfarin prescription initiated treatment among
30 days and 1, 12 months. Even though null in ITT analyses, in
all as-treated analyses, warfarin use versus non-use showed a
statistically significant trend toward decreased hazard of death.
It is far possible that the reduced threat for all-cause mortality
for warfarin users within the as-treated analyses is because of
the drug lowering the hazard of other fatal thromboembolic
events. [7]
Conclusion
To conclude, Warfarin use appears to have been associated
with no change in the incidence of ischemic stroke in patients
with atrial fibrillation and end-stage renal disease. However,
from the studies reviewed, it does appear to be associated
with a significantly higher risk of hemorrhagic stroke, with no
significant difference in the risk of major bleeding, and with no
change in mortality.
Competing Interests
The authors declare that they have no competing interests. All
the listed authors contributed significantly to the conception and
design of study, acquisition, analysis, and interpretation of data
and drafting of the manuscript, to justify authorship.
References
- Harel Z, Chertow GM, Shah PS, Harel S, Dorian P, Yan AT, et al. Warfarin and the risk of stroke and bleeding in patients with atrial fibrillation receiving dialysis: A systematic review and meta-analysis. Can J Cardiol. 2017;33:737-746.
- Tan J, Liu S, Segal JB, Alexander GC, McAdams-DeMarco M. Warfarin use and stroke, bleeding and mortality risk in patients with end stage renal disease and atrial fibrillation: A systematic review and meta-analysis. BMC Nephrol. 2016;17:157.
- Shen JI, Turakhia MP, Winkelmayer WC. Anticoagulation for atrial fibrillation in patients on dialysis: Are the benefits worth the risks?. Curr Opin Nephrol Hypertens. 2012;21:600.
- Randhawa MS, Vishwanath R, Rai MP, Wang L, Randhawa AK, Abela G, et al. Association between use of warfarin for atrial fibrillation and outcomes among patients with end-stage renal disease: A systematic review and meta-analysis. JAMA Netw Open. 2020;3:e202175.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 2009;62:e1-e34.
- Winkelmayer WC, Liu J, Setoguchi S, Choudhry NK. Effectiveness and safety of warfarin initiation in older hemodialysis patients with incident atrial fibrillation. Clin J Am Soc Nephrol. 2011;6:2662-2668.
- Shen JI, Montez-Rath ME, Lenihan CR, Turakhia MP, Chang TI, Winkelmayer WC. Outcomes after warfarin initiation in a cohort of hemodialysis patients with newly diagnosed atrial fibrillation. Am J Kidney Dis. 2015;66:677-688.
- Kai B, Bogorad Y, Nguyen LA, Yang SJ, Chen W, Spencer HT, et al. Warfarin use and the risk of mortality, stroke, and bleeding in hemodialysis patients with atrial fibrillation. Heart Rhythm. 2017;14:645-651.
- Lee KH, Li SY, Liu JS, Huang CT, Chen YY, Lin YP, et al. Association of warfarin with congestive heart failure and peripheral artery occlusive disease in hemodialysis patients with atrial fibrillation. J Chin Med Assoc. 2017;80:277-282.
- Tan J, Bae S, Segal JB, Zhu J, Alexander GC, Segev DL, et al. Warfarin use and the risk of stroke, bleeding, and mortality in older adults on dialysis with incident atrial fibrillation. Nephrology. 2019;24:234-244.
- Makani A, Saba S, Jain SK, Bhonsale A, Sharbaugh MS, Thoma F, et al. Safety and efficacy of direct oral anticoagulants versus warfarin in patients with chronic kidney disease and atrial fibrillation. Am J Cardiol. 2020;125:210-214.
- Belley-Cote EP, Eikelboom JW. Anticoagulation for stroke prevention in patients with atrial fibrillation and end-stage renal disease-first, do no harm. JAMA Netw Open. 2020;3:e202237.
- Sarratt SC, Nesbit R, Moye R. Safety outcomes of apixaban compared with warfarin in patients with end-stage renal disease. Ann Pharmacother. 2017;51:445-450.
- Shah M, Avgil Tsadok M, Jackevicius CA, Essebag V, Eisenberg MJ, Rahme E, et al. Warfarin use and the risk for stroke and bleeding in patients with atrial fibrillation undergoing dialysis. Circulation. 2014;129:1196-1203.
- Wang TK, Sathananthan J, Marshall M, Kerr A, Hood C. Relationships between anticoagulation, risk scores and adverse outcomes in dialysis patients with atrial fibrillation. Heart Lung Circ. 2016;25:243-249.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.