Enhancing the esthetics by using soft tissue graft before the placement of E max crowns: Case report
Received: 31-Jan-2025, Manuscript No. Amhsr-25-164165; Editor assigned: 03-Feb-2025, Pre QC No. Amhsr-25-164165 (PQ); Reviewed: 17-Feb-2025 QC No. Amhsr-25-164165 (Q); Revised: 17-Feb-2025, Manuscript No. Amhsr-25-164165 (R); Published: 03-Mar-2025
Citation: Alsubaiy EF. Enhancing the Esthetics by Using Soft Tissue Graft before the Placement of Emax Crowns: Case Report. Ann Med Health Sci Res. 2025; 1107-1109
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A 30-year-old male with a high smile line was diagnosed with a recession in his anterior crowns. The periodontist decided to cover the exposed portions with a soft tissue graft to maintain a good proportion of the length of the crowns. A comprehensive treatment plan was developed, focusing on the condition and level of the gingival tissue. The patient's teeth were restorable, except for three teeth that required dental implants. The treatment plan involved removing old crowns, fabricating provisional crowns, placing implants, and placing soft tissue grafts in the teeth. A home maintenance regimen was followed, and the final restorations were created. The patient's smile was improved by treating the teeth and surrounding gingiva, maximizing symmetry and shape. The patient's smile looked more cohesive and natural, with the soft tissue and crowns contributing to a well-balanced appearance. This case highlights the importance of a holistic approach to dental aesthetics over a purely tooth-centered approach.
Keywords
Dental procedures; Gastrostomy; Fixed Partial Dentures (FPDs); E-max;
Introduction
Gastrostomy Modern society places a high value on aesthetics in dentistry since a beautiful smile is linked to intelligence, popularity, kindness, and social standing [1]. Dental procedures have aesthetic value that goes beyond simply restoring teeth; they have a significant impact on a patient's quality of life, social interactions, and sense of self. Among the critical elements that contribute to a beautiful smile, the soft tissues surrounding the teeth specifically the gingiva play an indispensable role.
Gingival tissue, which frames teeth and influences smile symmetry, is often overlooked in dental restorations. Issues like gingival recession, asymmetry, or discolored tissues can impair the aesthetic result of restorations, even for meticulously restored teeth. Soft tissue grafting addresses these issues and creates an optimal crown foundation, ensuring better adhesion and longevity of the restoration [2].
Case Presentation
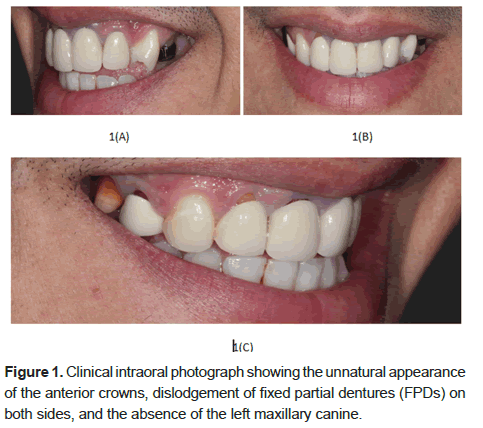
A 30 year old male reported to our institution with a chief complaint of the unnatural appearance of the anterior crowns, fallen of two Fixed Partial Dentures (FPDs) on both sides and the absence of the left upper canine (Figure 1). Clinical examination revealed the patient has a recession in the teeth #11 and #12. Moreover, teeth #24 is in the site of #23. The patient has a high smile line. Since the patient has a high smile line, we need to think about more than just replacing the anterior teeth to achieve satisfactory results.
During the diagnosis, it was clear that the length of the two crowns of #11 and #12 was acceptable. So, if we prepared the two teeth and put the finish lines more sub gingival to cover the exposed portions of the teeth, the two crowns would be too long. So, a consultation was done with the periodontist regarding the treatment of the recession to keep a good proportion in the length of the anterior crowns. The decision was made with the periodontist about the possibility of covering the exposed portions with a soft tissue graft.
First, a diagnostic wax-up was made according to the ideal length of the central incisors after the esthetics and phonetics evaluation. Moreover, tooth #24 was reshaped to look like a canine.
In this case, a comprehensive treatment plan was developed with a specific focus on the condition and level of the gingival tissue, recognizing its essential role in creating an aesthetically pleasing smile. The treatment plan was an interdisciplinary approach involving the improvement of periodontium before applying a fixed prosthesis. After explaining all the steps of the treatment plan to the patient, a consent form was signed by the patient.
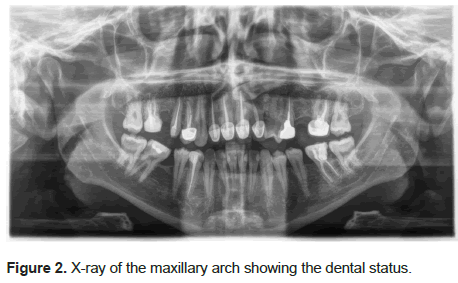
After careful evaluation of the maxillary arch, we conclude that all teeth are restorable except #17, #25 and #27 (Figure 2) X-ray, which require dental implants. So, we begin by removing old crowns and previous restorations of the remaining teeth in the upper arch. This is followed by the wax-up model for the fabrication of splinted provisional crowns.
The goal of the treatment was the fabrication of fixed prostheses that included fixed partial dentures supported by the implants in sites #25 and #27, the fabrication of implant-supported crowns in site #17 and the fabrication of E-max crowns for the remaining natural teeth.
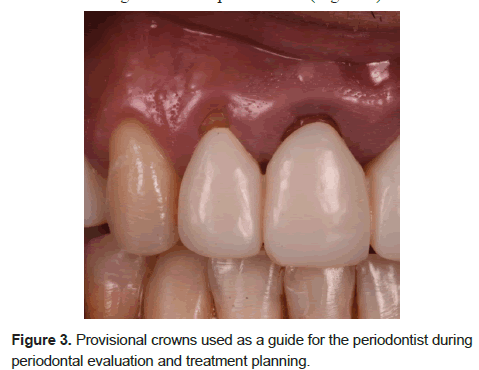
The second step of the treatment plan was the placement of implants in sites #17, #25, and #27 and the placement of soft tissue grafts in teeth #11 and #12. The provisional crowns had been used as a guide for the periodontist (Figure 3).
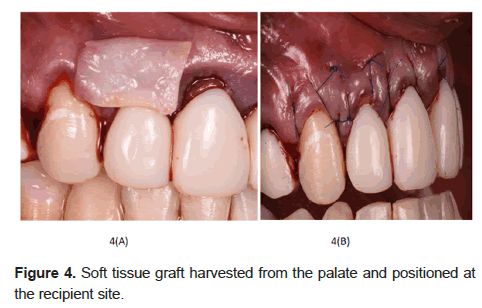
The soft tissue graft was taken from the palate and placed (Figure 4). Following surgery, a home maintenance regimen included a soft diet, thorough site cleaning with a soft bristle brush, and twice-daily mouth rinses with 0.12% Chlorhexidine Gluconate for seven days. Forty-eight hours, two weeks, and one month following surgery, the operative sites were reassessed. Clinical observations at this point showed acceptable healing with full re-epithelization of the donor site and satisfactory root coverage.
After four months, the healing was uneventful, and now we can proceed with the final restorations (Figure 5).
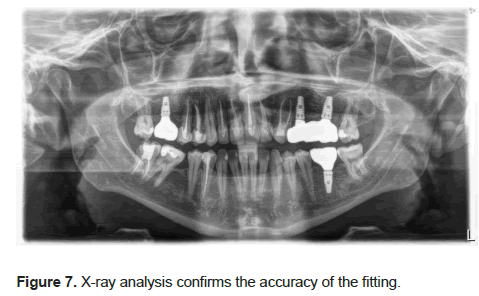
A custom tray was used for the final impression, and GC resin was used to splint the impression copings. The final impression was made using a light body and monophase (Zhermack). After the try-in of the final restorations (E-max) for the natural teeth and (zirconia with facial layering) for the crown and the FPD supported by the implants and confirming the fitting in the X-rays, final cementation was made by using Relyx Cement.
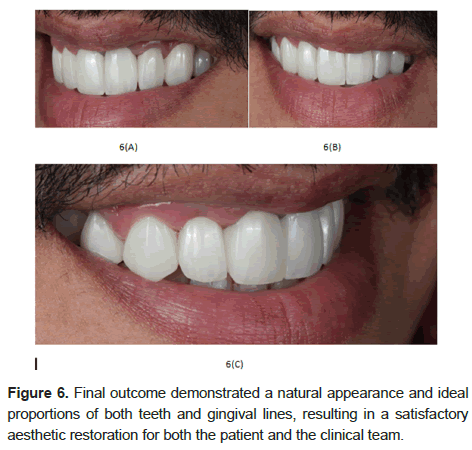
The final result was satisfactory for us and the patient since he got restorations with a natural look and an ideal proportion for the teeth and the gingival lines (Figure 6). The fitting is confirmed by the x-ray (Figure 7).
Our goal was to improve the patient's smile's harmony and balance by treating the teeth and the surrounding gingiva. By carefully evaluating the gingival level, we maximized symmetry and shape, producing outcomes that were both aesthetically pleasing and functionally sound.
The patient was given dental hygiene guidelines that included twice-yearly dental cleanings, daily flossing to remove food particles and plaque, and twice-daily thorough brushing with a soft-bristled toothbrush. After delivery, the patient was reviewed one week, one month, and six months later. After a year, the patient denied experiencing any discomfort or problems with the restorations during the follow-up appointments.
Discussion
Gingival esthetics must be developed to give a pleasing frame for dental restorations to get satisfactory results, as an appealing smile is essential in today's culture [1]. Gingival recession-related deficiencies have been addressed with periodontal procedures [3].
According to the American Academy of Periodontology's comprehensive evaluation, connective tissue grafts yield the best results in clinical settings [4]. To satisfy patients' aesthetic needs, soft tissue grafting techniques may be used in the anterior region [5].
Notably, when planning aesthetic treatments, many physicians tend to focus only on the alignment, shape, and colour of the teeth, frequently ignoring the gingiva's influence on the final appearance [2]. For dental professionals to manage soft tissue surrounding implants effectively, they must possess a thorough understanding of implant placement, prosthetic design, and tissue management, as well as advanced surgical skills for soft tissue grafting and augmentation [3]. This restricted focus can lessen the overall aesthetic effect and jeopardize the restorations' natural appearance. The importance of an integrated approach to smile design was shown when we produced an outcome that more closely matched the patient's aesthetic expectations by giving equal weight to gingival and dental elements in our treatment plan.
We knew the importance of the gingival component in the patient's smile and did not overlook it. The patient's smile looked more cohesive and natural, with the soft tissue and crowns both contributing to a well-balanced appearance. This outcome demonstrated the benefits of a holistic approach to dental aesthetics over a purely tooth-centered approach.
Limitations
This study was conducted at a single center with a small sample size especially in the LAPEG group which limits the statistical power. The decision-making process regarding the choice of Open-G or LAPEG was not governed by a strict protocol and may have been influenced by the lack of a standardized laparoscopic approach in our hospital until 2023. Our cost analysis was based on Japanese public health insurance fees and may not be generalizable to other healthcare systems. Furthermore, we did not include personnel costs, overheads for laparoscopic equipment, or objective measures of postoperative pain in our analysis. Therefore, caution is warranted in interpreting the cost-effectiveness findings. Future multicenter or prospective studies incorporating larger patient populations, more detailed operative data, and comprehensive cost calculations (including personnel and equipment costs) will be essential for a thorough evaluation.
Conclusion
The case highlights the importance of integrating soft tissue management into treatment plans for superior esthetic outcomes. By prioritizing gingiva condition, a harmonious foundation was established for E-max crowns, resulting in a balanced smile. This approach emphasizes the need to consider both dental and gingival components when planning esthetic restorations. The use of a soft tissue graft addressed gingival recession and enhanced the symmetry and contour of the gingiva, ensuring patient satisfaction. This case demonstrates that adopting a holistic perspective can improve the effectiveness of esthetic dental treatments and set a higher standard of care.
References
- Afrashtehfar KI, Bryant SR. Understanding the lived experience of North American dental patients with a Single-Tooth implant in the upper front region of the mouth: Protocol for a qualitative study. JMIR Research Protocols. 2021;10(6):e25767.
[Crossref] [Google Scholar] [PubMed]
- Sun TC, Chang T. Soft tissue management around dental implant in esthetic zone – the current concepts and novel techniques. Journal of Dental Sciences. 2024;19:1348–1358.
[Crossref] [Google Scholar] [PubMed]
- Altindal D, Tunca Y. A comparison of the smile esthetic understanding of periodontists, orthodontists, general dentists, and dental students. European Journal of Therapeutics. 2024; 30(3):267–276.
- Hürzeler MB, Weng D. A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent. 1999;19(3):279–287.
[Google Scholar] [PubMed]
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: A systematic review from the AAP Regeneration Workshop. Journal of periodontology. 2015; 86:S8–S51.
[Crossref] [Google Scholar] [PubMed]





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.