Established Osteoporosis and Gaps in the Management: Review from a Teaching hospital
- *Corresponding Author:
- Prof. Mir Sadat-Ali
Department of Orthopedic Surgery, University of Dammam and King Fahd Hospital of the University, P.O. Box 40071, AlKhobar 31952, Saudi Arabia.
E-mail: drsadat@hotmail.com
Abstract
Background: International osteoporosis foundation described severe or established osteoporosis as an osteoporotic individual with a fragility fracture. Orthopaedic surgeons frequently manage fractures, but we believe that large gaps are prevalent in the medical management of osteoporosis after fractures are fixed. Aim: The aim of this analysis is to assess the investigations and gaps in the management of osteoporosis in patients admitted with a fragility fracture of femur at King Fahd Hospital of the University, AlKhobar, Saudi Arabia. Materials and Methods: A retrospective analysis of all admission and discharge; medical and pharmacy records database of patients over ≥ 50 years with fragility fracture between January 2001 and December 2011. The outcome measures assessed were investigations such as serum calcium, phosphorous, alkaline phosphatase, parathormone, 25 hydroxy vitamin D (25OHD) levels and a dual energy X‑ray absorptiometry (DEXA). Secondly once the fracture was fixed what medications were prescribed, calcium and vitamin D, antiresorptives and anabolic agents. Results: There were 207 patients admitted during the study period with an average age of 69.2 (12.1) years and 118 were females. In 169 (81.6%) patients, the fracture site was proximal femur. Vitamin D (25OHD) was requested in 31/207 (14.9%). DEXA scan was ordered in 49/207 (24.1%). A total of 78/207 (37.6%) patients received calcium and vitamin D3 and 94/207 (45.4%) either got calcium or vitamin D3. Bisphosphonates was used in 35, miacalcic nasal spray in 25 and anabolic agent teriparatide was prescribed in 21 patients. Post‑fixation 126/207 (60.8%) patients did not receive any anti‑osteoporotic medication. In untreated group, there were 87 males and 39 females. Conclusions: The study found that in patients, who sustained a fragility fracture, confirmation of osteoporosis by DEXA was very low and ideal treatment for severe osteoporosis was given out to few patients. More efforts are needed to fill this large gap in the correct management of osteoporosis related fractures by orthopaedic surgeons.
Keywords
Fragility fractures, Management, Osteoporosis, Saudi Arabia
Introduction
Post-menopausal osteoporosis is common among Saudi Arabian population and reported prevalence of 35-38%[1-4] and male osteoporosis is not lagging behind with similar prevalence of 40%.[5,6]
Untreated osteoporosis leads to skeletal fractures with high morbidity and mortality. It was estimated that in USA by the year 2025, 3 million osteoporosis related fractures per year would cost in excess of $25 billion.[7]
It was reported that prevalence of femoral fractures in the eastern province of 6/1000 population with an economic cost to the government of Saudi Riyals 4.27 billion yearly for the whole country.[8]
Osteoporosis and fragility fractures could be prevented and the prevalence reduced if early intervention of diagnosis and proper treatment is introduced. The available treatment for osteoporosis is known to reduce the incidence of fragility fractures provided patients are diagnosed and treated appropriately.[9-11] Even with the well-organized conferences and reminders by international and local osteoporosis foundations emphasizing the problem of osteoporosis and cost in management many patients with established osteoporosis (osteoporosis + fragility fracture) are either missed and improperly treated.[12,13] Added to this Foley et al. (2007),[14] found that even after a fragility fracture only 10.2% of patients had a bone mineral density (BMD) done to diagnose osteoporosis.
The objective of this analysis is to assess the investigations and gaps in the management of osteoporosis in patients admitted with a fragility fracture of femur at King Fahd Hospital of the University, AlKhobar, Saudi Arabia.
Materials and Methods
This is a retrospective analysis of all patients admitted to King Fahd Hospital of the University, AlKhobar and a teaching institution of University of Dammam. All patients admitted to the hospital between January 2001 and December 2011, aged ≥ 50 years with a history of a fracture after a fall from the ground level were studied. Patient data was collected from the medical charts, which included type of fall, place of fall, diseases known to suffer by the patients at the time of admission, type of fracture, diagnosis, surgical management. From the QuadruMed patient care database, investigations ordered and performed like serum calcium, phosphorous, alkaline phosphatase, parathormone, 25 hydroxy vitamin D (25OHD) levels and a dual energy X-ray absorptiometry (DEXA) and medications dispensed to the patients. During the study period the pharmacy had dispensed calcium tablets of 600 mg per tablet, vitamin D analog (1 alpha 0.25 mcg, 0.5 mcg and 1 mcg), alendronate (fosamax 10 mgm, 70 mg), Ibandronic acid (bonviva 150 mg), zoledronic acid 5 mg intravenous (aclasta), calcitonin salmon nasal spray (miacalcic 100 milligrams) and teriparatide teriperatide 20 μmcg (forteo). Data was analyzed using the statistical package for the social sciences, version 14.0, Chicago, Illinois. Data was expressed as mean (standard deviation [SD]). A P < 0.05 was considered as significant.
Results
During the study period, 207 patients were admitted with a fragility fracture out of 9372 admissions, prevalence of 2.2/100 patients. The mean age was 69.2 (12.1) (56-105) years and 118 were females. On follow-up, it was found that 179 (86.4%) were osteoporotic and the rest osteopenic. Table 1 gives the site of fractures. In 169 (81%) patients, the fracture site was proximal femur. All patients had serum calcium and phosphorous levels and only 14 (6.8%) had parathormone level done. Vitamin D (25OHD) was requested in 49 (23.6%). DEXA scan was ordered in 49 (23.6%). There were 20 males and 29 females with the mean age of 68.8 (11.9) years. Table 2 gives the treatment of 49 patients whom BMD was done. Even after the diagnosis of osteoporosis, male patients were neglected more than the female patients.
| Investigation performed | Number of patients |
|---|---|
| Blood investigation (serum calcium, | 207 |
| phosphorus, alkaline phosphatase, | |
| renal function tests, serum creatinin) | |
| Serum 25OHD | 49 |
| DEXA scan hip+spine | 49 |
| Calcium or vitamin D3 | 94 |
| Calcium with vitamin D3 | 78 |
| Calcium+vitamin D3+bisphosphonates | 35 |
| Calcium+vitamin D3+calcitonin | 25 |
| Calcium+vitamin D3+teriparatide | 21 |
25OHD: 25 hydroxy vitamin D, DEXA: Dual energy X-ray absorptiometry
Table 1: Details of investigations and treatment received by patients
| Male (20) | Female (29) | P value | |
|---|---|---|---|
| Mean age | 72.4 (10.2) | 68.7 (11.9) | 0.10 |
| Hip BMD g/cm2 (lowest value) | 0.434 | 0.367 | 0.60 |
| Spine BMD g/cm2 (lowest value) | 0.606 | 0.431 | 0.20 |
| Calcium | 12 | 25 | 0.04 |
| Vitamin D3 | 6 | 29 | <0.001 |
| Calcium vitamin D and | 7 | 19 | 0.03 |
| osteoporosis therapy |
BMD: Bone mineral density, DEXA: Dual energy X-ray absorptiometry
Table 2: Summary of the overall treatment received in patients with DEXA scan
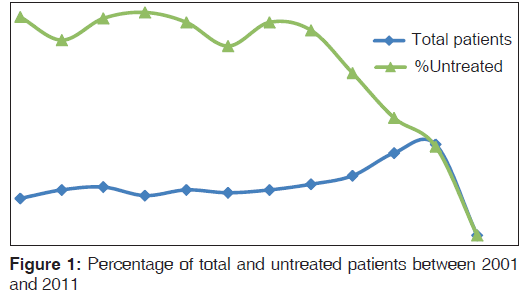
A total of 78 (37.6%) patients received calcium and vitamin D3 and 94 either got calcium or vitamin D3. Bisphosphonates was used in 35, miacalcic nasal spray in 25 and anabolic agent teriparatide was prescribed in 21 patients. Post-fixation 126 patients had did not receive any anti-osteoporotic medication. In this group, there were 87 males and 39 females with a mean age was 69.9 (12.8). The average age of the treated group was 68.2 (11.3) years and the mean age in the untreated group were 69.9 (12.8) (P = 0.30). There is a drop in the trend of untreated patients from 76% in 2001 to 30% in 2011 [Figure 1].
Discussion
In this study, we have found that only 22.7% of the admitted patients with fragility fracture got the recommended treatment for the condition which is calcium, vitamin D, antiresorptive/ anabolic agent. The number of untreated patients who got at least vitamin D and calcium dropped from over 76% in 2001 to 30% in 2011. A DEXA was carried out in 49 (23.6%), in this study and this was lower in comparison to the report of Smith et al.[15] Two reports from USA found that none of the patients who were admitted with a fragility fracture had a DEXA done.[12,16]
The overlooked management of osteoporosis during the post-fracture period appears universal. Rabenda et al. (2008),[17] reported from Belgium that 6% of patients hospitalized for hip fractures were prescribed anti-osteoporotic medications. Bellantonio et al. (2001),[18] reported that in their analysis, 13% were found to have rece12ived the recommended treatment and over 40% did not received any form of treatment even after 25 months, whereas Smith et al.[15] reported that in their patients 39% had received treatment for osteoporosis.
A recent nation-wide study from USA jolted many physicians and surgeons alike when Jennings et al. (2010),[19] found that only 2% of the patients who were admitted to 318 hospitals with osteoporosis related hip fracture received the recommended treatment. This is in comparison to our study is low. The reasons of our better performance is due to the fact that ours is a teaching institution and osteoporosis and its impact on the human race is discussed regularly, whereas Jennings et al. reported from different level hospitals. Secondly, the orthopaedic surgeons usually tend to fix the fractures and internists/endocrinologists do the medical management, but we have taken the privilege to medically manage post-fixation. Lately, it was suggested that age, gender and race could play a role in providing the ideal treatment.[20,21]
Haaland et al. (2009)[22] reported that there were clear improvements in the management of osteoporosis in patients post-fragility fracture at the same center from 1990,[23] from 0% to 21% of antiresorptives and calcium and vitamin D for 17.7% to 34.4%. They have attributed this significant increase due to “Fracture: Think osteoporosis” program, at the McMaster University, Hamilton, Ontario, published guidelines[24] and cost-effectiveness data.[25] In the present study, the number of untreated patients dropped from over 76% in 2001 to 30% in 2011. In Saudi Arabia, still we don’t have any national guidelines; hence the improvement, which we have observed at our center, may not reflect in other hospitals of the country. Department of Orthopaedic Surgery at the University of Dammam, which took the challenge of correctly managing osteoporosis and related fractures, has paid off in the substantial improvement, but much more work is required in early diagnosis and treatment of osteoporosis before a fracture occurs.
We have to acknowledge that our study has few limitations. The retrospective nature of the study in itself raises issues of the completed medical charts from where the data was extracted. The strength of this study was that all physicians orders for BMD, medications, etc., are entered in the QuardruMed when ordered and the patients receive the medications; hence, the results are unbiased.
Our study shows that gaps in the management of osteoporosis post-fracture are universal. At our institution, there was a substantial improvement in the management of post-fracture osteoporosis at our center, but still there is a wide gap in the ideal management of osteoporosis post-fracture, strategies in the form of protocols, guidelines and education programs for all physicians in the issues of osteoporosis and its diagnosis and management. We need to increase the information and knowledge about the ideal osteoporosis management to improve its application in patient care. It is incumbent upon all physicians not to allow any gaps in the treatment of osteoporotic patients.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Sadat-Ali M, Al-Habdan I, Al-Mulhim F, Yousef A. Bone mineral density among postmenopausal Saudi Arabian women. Saudi Med 2004;25:1623-5.
- El-Desouki MI, Sherafzal MS, Othman SA. Comparison of bone mineral density with dual energy x-ray absorptiometry, quantitative ultrasound and single energy X-ray absorptiometry. Saudi Med J 2005;26:1346-50.
- Ardawi MS, Maimany AA, Bahksh TM, Nasrat HA, Milaat WA, Al-Raddadi RM. Bone mineral density of the spine and femur in healthy Saudis. Osteoporos Int 2005;16:43-55.
- Sadat-Ali M, Al-Habdan I, Marwah S. Bone mineral density measurements of distal radius in Saudi Arabian females. Ann Saudi Med 1996;16:414-6.
- El-Desouki MI, Sulimani RA. High prevalence of osteoporosis in Saudi men. Saudi Med J 2007;28:774-7.
- Sadat-Ali M, AlElq A. Osteoporosis among male Saudi Arabs: A pilot study. Ann Saudi Med 2006;26:450-4.
- Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22:465-75.
- Bubshait D, Sadat-Ali M. Economic implications of osteoporosis-related femoral fractures in Saudi Arabian society. Calcif Tissue Int 2007;81:455-8.
- Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 2007;357:1799-809.
- MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, et al. Systematic review: Comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 2008;148:197-213.
- Morin S, Rahme E, Behlouli H, Tenenhouse A, Goltzman D, Pilote L. Effectiveness of antiresorptive agents in the prevention of recurrent hip fractures. Osteoporos Int 2007;18:1625-32.
- Kamel HK, Hussain MS, Tariq S, Perry HM, Morley JE. Failure to diagnose and treat osteoporosis in elderly patients hospitalized with hip fracture. Am J Med 2000;109:326-8.
- Kiebzak GM, Beinart GA, Perser K, Ambrose CG, Siff SJ, Heggeness MH. Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 2002;162:2217-22.
- Foley KA, Foster SA, Meadows ES, Baser O, Long SR. Assessment of the clinical management of fragility fractures and implications for the new HEDIS osteoporosis measure. Med Care 2007;45:902-6.
- Smith MD, Ross W, Ahern MJ. Missing a therapeutic window of opportunity: An audit of patients attending a tertiary teaching hospital with potentially osteoporotic hip and wrist fractures. J Rheumatol 2001;28:2504-8.
- Bahl S, Coates PS, Greenspan SL. The management of osteoporosis following hip fracture: Have we improved our care? Osteoporos Int 2003;14:884-8.
- Rabenda V, Vanoverloop J, Fabri V, Mertens R, Sumkay F, Vannecke C, et al. Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Joint Surg Am 2008;90:2142-8.
- Bellantonio S, Fortinsky R, Prestwood K. How well are community-living women treated for osteoporosis after hip fracture? J Am Geriatr Soc 2001;49:1197-204.
- Jennings LA, Auerbach AD, Maselli J, Pekow PS, Lindenauer PK, Lee SJ. Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc 2010;58:650-7.
- Farley JF, Cline RR, Gupta K. Racial variations in antiresorptive medication use: Results from the 2000 Medical Expenditure Panel Survey (MEPS). Osteoporos Int 2006;17:395-404.
- Feldstein AC, Nichols G, Orwoll E, Elmer PJ, Smith DH, Herson M, et al. The near absence of osteoporosis treatment in older men with fractures. Osteoporos Int 2005;16:953-62.
- Haaland DA, Cohen DR, Kennedy CC, Khalidi NA, Adachi JD, Papaioannou A. Closing the osteoporosis care gap: Increased osteoporosis awareness among geriatrics and rehabilitation teams. BMC Geriatr 2009;9:28.
- Papaioannou A, Wiktorowicz M, Adachi JD, Goeree R, Papadimitropoulos E, Bedard M, et al. Mortality, independence in living, and re-fracture, one year following hip fracture in Canada. Soc Obstet Gynaecol Can 2000;22:591-7.
- Brown JP, Josse RG, Scientific Advisory Council of the Osteoporosis Society of Canada. 2002 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2002;167:S1-34.
- Rosner AJ, Grima DT, Torrance GW, Bradley C, Adachi JD, Sebaldt RJ, et al. Cost effectiveness of multi-therapy treatment strategies in the prevention of vertebral fractures in postmenopausal women with osteoporosis. Pharmacoeconomics 1998;14:559-73.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.