Estimated Probability of Stroke Among Medical Outpatients in Enugu South East Nigeria
- *Corresponding Author:
- Dr. Ezeala-Adikaibe B
Department of Medicine, University of Nigeria Teaching Hospital, PMB 01129, Enugu, Nigeria.
E-mail: birinusadikaibe@gmail.com
Citation: Ezeala-Adikaibe B, Mbadiwe N, Orjioke C, Aneke E, Chime P, Okafor H, et al. Estimated probability of stroke among medical outpatients in Enugu south east Nigeria. Ann Med Health Sci Res 2014;4:879-83.
Abstract
Background: Stroke is a growing noncommunicable disease in Africa and accounts for a substantial number of medical and neurological admissions in Nigerian hospitals. The prevalence of some risk factors for stroke such as hypertension and diabetes are high and growing among Africans. Aim: The aim was to investigate the distribution of stroke risk factors and estimate the 10‑year probability of stroke among patients attending the out‑patient clinics in the two biggest hospitals in Enugu South East Nigeria. Subjects and Methods: Consecutive consenting patients attending out‑patient clinics at University of Nigeria Teaching Hospital and Enugu state University of Science and Technology Teaching Hospital all in Enugu were enrolled. Risk factors for stroke were evaluated using a series of laboratory tests, medical history and physical examinations. The 10‑year probability of stroke was determined by applying the Framingham stroke risk equation. Statistical analysis was performed with the use of the SPSS 17.0 software package (SPSS Inc., Chicago, IL, USA). Results: A total of 165 patients were evaluated. Of these 94 were male and 71 were female. The most common risk factors were left ventricular hypertrophy 70.3% (116/165) and raised systolic blood pressure 52.7% (87/165). The mean age of patients was 66.1 (8.1) years. The mean 10‑year probability of stroke was 18.1 (14.6) (19.7 [14.9] in men and 14.5 [14.6] women) and was higher in older age groups. Conclusion: The 10‑year probability of stroke in Nigerians attending medical outpatient Clinic in SE Nigeria may be high. Aggressive interventions are needed to reduce risk factors and the probability of stroke risks especially in men in SE Nigeria.
Keywords
Cardiovascular risks, Nigeria, Stroke
Introduction
Stroke is a growing non communicable disorder in Nigeria.[1] With a prevalence of 1.14/1000,[2] strokes account for 15.9% of medical ward and 65.5% of neurological admission in tertiary health care facilities in Enugu.[3,4] The 30-day mortality in Nigeria was found to be 40% by Ogun et al.[5] The established risk factors for ischemic stroke include age, systolic blood pressure (SBP), use of anti-hypertensives, diabetes, smoking, cardiovascular diseases (CVD), atrial fibrillation (AF), and left ventricular hypertrophy (LVH). Based on 472 stroke events occurring during 10 years’ follow-up from biennial examinations Wolf et al.[6] computed stroke probabilities using the Cox proportional hazards model for men and women based on a point system. Using the Framingham risk score, we investigated the distribution of stroke risk factors and estimated the 10-year probability of stroke (10-year PS) among patients attending outpatient clinics in the two biggest hospitals in Enugu South East Nigeria.
Subjects and Methods
Study population
We conducted a two center study evaluating patients seen in the medical outpatient clinic of the two largest hospitals in Enugu, South East Nigeria. All consecutive consenting patients aged 54-84 years as at their last birthday were recruited. Patients were recruited from different sub specialist clinics. Our study population included 165 patients between 55 and 84 years of age. Exclusion criteria was refusal to participate and a history of stroke (present or in the past). All investigations were done in the medical out-patient clinic of the two hospitals. All subjects gave informed consent. This study was approved by the hospitals’ ethics committee. The study duration was 7 months (September 2009–March 2010).
Physical examination and laboratory measurement
Blood pressure was measured in the right arm, using an appropriately sized cuff and a standard mercury sphygmomanometer, after the subjects had been seated for at least 5 min, with feet on the floor and arm supported at heart level. Fasting plasma glucose samples were obtained in the morning of the clinic visit. Patients with a previous history of diabetes were recruited irrespective of their last fasting plasma glucose levels. Laboratory investigations were only repeated if they were not previously recorded or physical examination suggested otherwise. LVH and AF were diagnosed using an electrocardiograph. Other risk factors were evaluated through history and physical examination.
Estimation of 10-year probability of stroke
The Framingham stroke risk score was estimated using the risk developed by Wolf et al. using the following predictors-SBP; diabetes/history of diabetes; smoking (current); CVD myocardial infarction or intermittent claudication, angina pectoris, coronary insufficiency, or congestive heart failure; history of AF and LVH on electrocardiogram (ECG). Risk factors identified in the study and used in evaluating the 10-year PS were SBP, use of antihypertensives (treated hypertension), age, diabetes mellitus smoking, medical history of CVD, AF and LVH. Serum cholesterol was not used in the original Framingham equation and was excluded. The formula for risk score evaluation is beyond the scope of this study and has been detailed elsewhere.[6] Based on the presence of any of the above risk factors, patient were assigned specific scores. The sum of these scores was used to check for the probability of stroke within 10 years using stroke risk tables.
Definition of terms
High blood pressure (HBP) was identified by repeated blood pressure measurements or previous diagnosis. HBP stage was classified according to WHO-ISH,[7] stage 1 (140-159/90-99), stage 2 (160-179/100-109), and stage 3 (=180/110). Diabetes mellitus was defined as fasting blood glucose concentration =126 mg/dL, history of diabetes or use of glucose lowering drugs. Only “current smokers” were recorded as smokers. AF was confirmed by ECG. Sokolow and Lyon[8] voltage (SV1 + RV5/6) >35 mm and or the cornell voltage duration product[9] ([RaVL + SV3] × QRS duration [men], [RaVL + SV3 + 0.8 mV] × QRS duration [women] =244.0 mVms) (LVH SV3 + RaVL >28 mm [men], SV3 + RaVL > 20 mm [women])[10] were used to identify LVH. CVD was defined as any or a combination of the following; current history of hospitalization for myocardial infarction, angina and congestive heart failure.
Statistical analysis
For database management and statistical analyses, we used the SPSS version 17 (IBM Corporation, New York, USA). Age of the patients was put into 3 different categories for easy tabulation and comparison. Continuous variables were expressed as means ± standard deviation and categorical variables were reported as numbers and percentages (%). Mean ages of men and women were compared using Student’s t-test. Categorical variables were compared using the Chi-square test or Fisher’s exact tests where applicable. P < 0.05 was considered as statistically significant.
Results
Baseline characteristics and risk factors
The baseline characteristics and risk factors of the patients are summarized in Table 1. Our sample included 94 men and 71 women. The mean age of the patients was 66.1 (8.1) years (67.3 [8.2] men, 64.6 [7.9] women). Men were significantly older than women P = 0.03.
| Risk factors | n (%) | P | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total | ||||
| <60 years | 19(20.2) | 20(28.2) | 39(23.6) | 0.87 | ||
| 60-69 years | 36(38.3) | 33(46.5) | 69(41.2) | 0.72 | ||
| >70 years | 39(41.5) | 18(31.6) | 57(34.6) | 0.01 | ||
| THBP* | 55(58.5) | 42(59.2) | 97(58.8) | 0.93 | ||
| Controlled HBP | 3(5.5) | 7 (17.5) | 10(10.3) | 0.21 | ||
| Normal BP | 42(44.7) | 36(50.7) | 78(47.3) | 0.50 | ||
| Hypertension | ||||||
| SBP stage I | 29(30.9) | 16(25.4) | 45(27.3) | 0.05 | ||
| SBP stage II | 11(11.7) | 14(19.7) | 25(15.2) | 0.54 | ||
| SBP stage III | 12(12.8) | 5 (10.3) | 17(10.3) | 0.09 | ||
| Diabetes | 28(29.8) | 12(16.9) | 40(24.2) | 0.01 | ||
| Heart disease | 18(19.1) | 14(19.7) | 32(19.4) | 0.48 | ||
| Atrial fibrillation | 6(6.4) | 4(5.6) | 10 (6.1) | 0.53 | ||
| LVH† | 69(73.4) | 47(66.2) | 116 (70.3) | 0.04 | ||
| LVH# | 63 (67) | 41(57.7) | 110 (66.6) | 0.39 | ||
| Smoking | 2(1.2) | - | 2(1.2) | - | ||
Table 1: Characteristics of risk factors in study subjects
Systolic blood pressure ranged from 100 to 210 mmHg, with a mean of 143.0 (26.2) mmHg (men 143.9 [27.9], women 141.8 [23.9]) P = 0.86. The commonest risk factor was LVH which was identified in 70.3% (116/165), (73.4% [69/94] men, 66.2% [47/71] women). On recruitment, SBP was high in 52.7% (87/165); (55.3% [52/94] men, 49.3% [35/71] women) [Table 1]. The distribution of risk factors in the various age groups is shown in Table 2. LVH remained the most prevalent risk factor in all age groups, but the proportion was highest in those above 70 years. In that same age group, the proportion of women with LVH was more than that of men.
| n (%) | P | |||||
|---|---|---|---|---|---|---|
| Males | Female | Total | ||||
| <60 years (n=39) | ||||||
| THBP* | 9 (47.4) | 13 (65) | 22(56.4) | 0.19 | ||
| Normal | 10 | (52.6) | 12 (60) | 22(56.4) | 0.67 | |
| Hypertensive | 9 (47.4) | 8 (40) | 17(43.6) | 0.81 | ||
| Diabetes | 1(5.2) | 3 (15) | 4 (10.3) | 0.03** | ||
| Heart disease | 4 (21.1) | 2 (10) | 6 (15.4) | 0.10 | ||
| Atrial fibrillation | - | 1 (5) | 1(2.6) | - | ||
| LVH | 14(73.7) | 7 (35) | 21(53.8) | 0.13 | ||
| LVH# | 12(63.2) | 6 (30) | 18(46.2) | 0.04 | ||
| 60-69 years (n=69) | ||||||
| THBP* | 25(64.4) | 22(66.7) | 47(68.1) | 0.67 | ||
| Normal | 13(36.1) | 16(48.5) | 29 (42) | 0.67 | ||
| Hypertensive | 23(63.9) | 14(42.4) | 37(53.6) | 0.14 | ||
| Diabetes | 10(27.7) | 5 (15.2) | 15(21.7) | 0.07 | ||
| Heart disease | 3(8.3) | 7 (21.2) | 10(14.5) | 0.21 | ||
| Atrial fibrillation | - | 2(6.1) | 2(2.8) | - | ||
| LVH | 26(72.2) | 22(66.7) | 48(69.6) | 0.56 | ||
| LVH# | 25(69.4) | 20(60.6) | 45(65.2) | 0.44 | ||
| >70 years (n=57) | ||||||
| THBP* | 19 | (48.7) | 5 (27.8) | 33(57.9) | <0.01 | |
| Normal | 19 | (48.7) | 8 (44.4) | 27(47.4) | 0.03 | |
| Hypertensive | 20 | (51.3) | 10 | (55.6) | 30(52.6) | 0.07 |
| Diabetes | 16 | (41.0) | 5 (27.8) | 21(36.8) | 0.02 | |
| Heart disease | 10 | (25.6) | 6 (33.3) | 16(28.1) | 0.32 | |
| Atrial fibrillation | 6 (15.4) | 1 | (5.6) | 7 (12.3) | 0.06 | |
| LVH | 27 | (69.2) | 16 | (88.8) | 43(75.4) | 0.09 |
| LVH# | 26 | (66.7) | 15 | (83.3) | 40(70.2) | 0.19 |
| Smoking | 2 | (5.1) | - | 2(3.5) | - | |
Table 2: Distribution of risk factors in different age groups
Ten-year probability of stroke
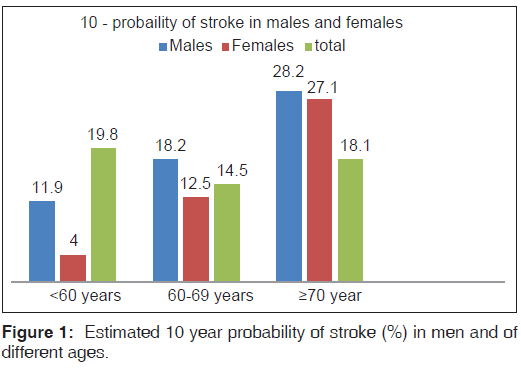
The mean 10-year PS was 18.1 (14.6), significantly higher in men than in women (men 19.7 (14.9) and women 14.5 (14.6) (P < 0.01) [Figure 1]. As expected, 10-year PS was different in different age groups reaching as high as 28.2 (17.8) in men 70 years and above.
Discussion
The major findings in this include high frequency of LVH (70.3%), overall poor blood pressure control (52.7%) and high frequency of diabetes (29.8%) rates of diabetes. LVH remained the most prevalent risk factor in all age groups, but the proportion was highest in those above 70 years. The mean 10-year PS was 18.1 (14.6), significantly higher in men 19.7 [14.9] than women 14.5 [14.6] (P = 0.01) 10-year PS was different in different age groups, reaching as high as 28.2 (17.8) in men 70 years and above.
The 10 year PS was lower than 26.3 found in Koreans[11] hypertensive patients where the 10-year PS was also significantly higher in women than in men. Our study population was selected from medical outpatient clinic, which included nonhypertensive patients. In the US,[12] African Americans had a greater age- and sex-adjusted mean 10-year predicted stroke probability than whites: 12.0 versus 9.2 respectively much lower than the findings in the index study. The mean stroke risk doubled after 60 years and quadrupled after the age of 70. This increase was similar for men and women, but was steeper in women. The major reasons for high estimated probability of stroke in our patients were likely to be high prevalence of HBP and LVH among them.
The mean 10-year PS in women increased with age becoming similar to that of men after 70 years. After this age the frequency of LVH, CVD, and stage II HBP were more in women than in men and the proportion of women with diabetes increased as well. The risk of stroke increases after menopause as the protective function of sex hormones on cardiovascular system wanes. Furthermore, the prevalence of diabetes and obesity are generally higher in older women hence increasing their risk of hypertension and stroke. Factors contributing to higher risk in males in this study would include older age of men and the higher proportion of men above 70 years. Men had a higher proportion of most risk factors such as LVH, diabetes, smoking and AF.
The prevalence of HBP in this study is 58.8% (58.5% in men and 59.2% in females) 27.3% had stage I hypertension, 15.2% stage II hypertension and 24.2% stage III hypertension. These values are higher than what is found in Nigerian general population (14.5% [14.7% men and 14.3% women]).[1] The very high proportion of HBP may be due center bias. All participants were selected from two specialist centers were possible patients with poorly controlled blood pressure were referred and the older age group studied. It is interesting to note that the proportion with stage II HBP were more in females, which is different from what is seen in the general population.[1] The reasons for this are not known, however women are known to have a better health seeking behavior than men.
Even before the commencement of treatment, HBP is known to cause target organ damage.[13,14] The importance of systemic HBP in the etiology of stroke has been well described among Nigerians and has been shown that a history of systemic hypertension is the most common risk factor, found in 50-85% of all patients[13-15]
The prevalence of LVH in this study is 70.3% revealing a high frequency of undiagnosed HBP. LVH has been reported in 31% of the general population with normal blood pressure and in 30% of patients with stage I hypertension,[14,16] thus suggesting that LVH may occur early in hypertensives. Using ECG, Salako et al.[14] found that 44.8% of newly diagnosed hypertensives had LVH. AF was found in 6.1%. This frequency of AF is higher than the frequency of AF among patients with HBP and stroke in Nigeria (3.7% and 1.2% respectively).[13,15]
The higher prevalence of risk factors seen with advancing age supports the fact the CVD and its risk factors increase with age. It also suggests that in individual patients, HBP might have been present for such a long time as to have caused end-organ damage.
The prevalence of diabetes in our study population is 24.2% (29.8% men, 16.9% women), it increased with advancing age; reaching 36.8% (41% in males and 27.8% in females) in those older than 70 years. The prevalence of diabetes in the Nigerian is 2.2% reaching a prevalence of 7.9%[1,17] in those older than 40 years. In addition to age, the role of ethnicity and change in life style on the prevalence of diabetes in some ethnic groups has been documented earlier.[18,19] Worsening of insulin resistance with age, increasing longevity of diabetic patients due to improved care, all contribute to the rising prevalence of type 2 diabetes with age, which may also explain the high prevalence of diabetes found in this study.
The rate of tobacco smoking was 2.5% (5.1% in men, none in women) in this study. The prevalence of current smoking among Nigerians varies both within and between populations. It is influenced by various factors such as age, sex, ethnicity, rural or urban dwelling and religion. Prevalence of smoking in this study was lower than reports from the 2002 national survey which showed a prevalence 8.6% and 17.6% among rural dwellers in South West Nigeria.[20] Our enrolled subjects were older subjects and are considered high risk patients for diabetes mellitus, AF, LVH, HBP, and CVD, but are less likely to be active smokers. Though, tobacco is utilized in many forms in South East Nigeria especially as snuff among the elderly, cigarette smoking is commoner in the young.
Limitations
First, our study population of 165 was derived from a highly selected group of patients who were visiting tertiary hospitals referred for several reasons, including uncontrolled HBP, diabetes mellitus, and CVD. The study population is therefore does not represent the 10 year stroke risk in the community as cardiovascular risk factors may be over represented in our sample. Second, this study was a simple cross-sectional study and did not consider information about practical stroke events. Therefore, we could not compare 10-year probability of stroke with real stroke incidence. Third, we assessed smoking status with a single, self-reported questionnaire. Therefore, non-differential misclassification is possible because patient might use tobacco in various forms.
Conclusion
The mean 10-year PS among patients 54 years and above attending medical out-patient clinic in 2 tertiary hospital in Enugu was 18.1 ± 14.6% (19.7 ± 14.9% men, 14.5 ± 14.6% women). As expected, 10-year probability of stroke was different in different age groups. In subjects below 70 years, there was a statistically significant difference between the 10-year risk of stroke in men and women.
References
- Akinkugbe OO, editor. Non Communicable Disease in Nigeria. Lagos: Final Report of National Survey, Federal Ministry of Health and Social Services; 1997. p. 64-90.
- Danesi M, Okubadejo N, Ojini F. Prevalence of stroke in an urban, mixed-income community in Lagos, Nigeria. Neuroepidemiology 2007;28:216-23.
- Ezeala-Adikaibe B, Aneke E, Orjioke C, Ezeala-Adikaibe N, Mbadiwe N, Chime P, et al. Pattern of medical admissions at enugu state university of science and technology teaching hospital: A 5 year review. Ann Med Health Sci Res 2014;4:426-31.
- Ekenze OS, Onwuekwe IO, Ezeala Adikaibe BA. Profile of neurological admissions at the University of Nigeria Teaching Hospital Enugu. Niger J Med 2010;19:419-22.
- Ogun SA, Ojini FI, Ogungbo B, Kolapo KO, Danesi MA. Stroke in south west Nigeria: A 10-year review. Stroke 2005;36:1120-2.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the Framingham Study. Stroke 1991;22:312-8.
- 1999 World Health Organization – International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Sub-Committee. Blood Press Suppl 1999;1:9-43.
- Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 1949;37:161-86.
- Molloy TJ, Okin PM, Devereux RB, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol 1992;20:1180-6.
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281-357.
- Choi CU, Park CG. Estimating the probability of stroke in Korean hypertensive patients visiting tertiary hospitals using a risk profile from the Framingham study. BMC Neurol 2009;9:16.
- Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, et al. Estimated 10-year stroke risk by region and race in the United States: Geographic and racial differences in stroke risk. Ann Neurol 2008;64:507-13.
- Ayodele OE, Alebiosu CO, Salako BL, Awoden OG, Abigun AD. Target organ damage and associated clinical conditions among Nigerians with treated hypertension. Cardiovasc J S Afr 2005;16:89-93.
- Salako BL, Ogah OS, Adebiyi AA, Adedapo KS, Bekibele CO, Oluleye TS, et al. Unexpectedly high prevalence of target-organ damage in newly diagnosed Nigerians with hypertension. Cardiovasc J Afr 2007;18:77-83.
- Karaye KM, Nashabaru I, Fika GM, Ibrahim DA, Maiyaki BM, Ishaq NA, et al. Prevalence of traditional cardiovascular risk factors among Nigerians with stroke. Cardiovasc J Afr 2007;18:290-4.
- Karaye KM, Okeahialam BN, Wali SS. Cardiovascular risk factors in Nigerians with systemic hypertension. Niger J Med 2007;16:119-24.
- Nyenwe EA, Odia OJ, Ihekwaba AE, Ojule A, Babatunde S. Type 2 diabetes in adult Nigerians: A study of its prevalence and risk factors in Port Harcourt, Nigeria. Diabetes Res Clin Pract 2003;62:177-85.
- Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997;349:1436-42.
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349:1269-76.
- Ayankogbe OO, Inem OA, Bamgbala OA, Robert OA. Attitudes and determinant of cigarette smoking among rural dwellers South West Nigeria. Niger Med Pract 2003;44:70-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.