Evaluation of Inhaler Techniques Among Asthma Patients Seen in Nigeria: An Observational Cross Sectional Study
- *Corresponding Author:
- Dr. Cajetan Chigozie Onyedum
Department of Medicine, Respiratory Unit, College of Medicine, University of Nigeria, Enugu Campus, Enugu, Enugu State, Nigeria.
E-mail: cajetan.onyedum@unn.edu.ng
Citation: Onyedum CC, Desalu OO, Nwosu NI, Chukwuka CJ, Ukwaja KN, Ezeudo C. Evaluation of inhaler techniques among asthma patients seen in Nigeria: An observational cross sectional study. Ann Med Health Sci Res 2014;4:67-73.
Abstract
Background: An Adequate and an effective dose of inhalation drugs can be administered only if the correct inhaler‑specific technique is followed by asthma patients. There is paucity of data on this subject among Nigerians and Africans. Aims: This observational study was to assess the inhaler techniques among asthma patients in Nigeria and also to identify the factors related to an inaccurate or poor inhaler use. Subjects and Methods: Consenting asthma patients on inhalers, who attended medical out‑patients clinic, of two university hospitals in Nigeria were asked to use their inhalers while an inhaler‑administration checklist was used to assess each patients inhaler technique. Information on demographics, asthma symptoms history and history of technique education were obtained. Data was analyzed using standard statistical methods. Results: A total of 140 asthma patients participated out of which 75 were females. All the patients used pressurized metered dose inhalers (pMDI) type; 51 of them used dry powder inhalers (DPI) in addition. For pMDI, 22.1% (31/140) completed all required steps while 37.3% (19/51) did so for DPI (P = 0.04). Patients with higher educational qualification (P < 0.01) and those with less frequent asthma symptoms (P < 0.01) are more likely to use the pMDI inhalers more accurately while patients who have been taught previously by a Doctor were more likely to use the DPI better. Conclusion: Majority of asthma patients use their inhalers inaccurately. Patient‑dependent factors were identified as the cause of incorrect technique of inhaler use. Asthma patients on inhalation medications should have routine assessment of their inhaler technique at every visit and corrected if found to be poor.
Keywords
Asthma, Dry powder inhalers, Inhaler-administration checklist, Inhaler technique, Pressurized metered dose inhaler
Introduction
Drug inhalation is an important and a common mode of administration of drugs used in the management of Asthma and other obstructive airway diseases. These medications are often administered as pressurized metered dose inhalers (pMDI), dry powder inhalers (DPI), or with nebulizers. The pressurized metered dose and the DPI devices are the preferred pulmonary drugs delivery methods as the patients are able to use them on their own with minimal assistance if they are taught well.[1]
Although both pMDIs and DPIs are relatively simple devices to operate, their proper use are not entirely intuitive and each has technical limitations that can limit their effectiveness.[1] Each type of inhaler is different, with device specific instructions for use. In some cases, the steps can be confused between devices, resulting in severe reductions in drug available to patients.[2]
An accurate use of these devices in administering the drugs invariably has a direct relationship with the delivery and efficacy of the medications. When the technique of inhalation is poor, the drugs are often not delivered appropriately to the site of action leading to poor treatment outcomes. Poor inhalation technique leads to insufficient medication effects and to the prescription of more or additional medication with a higher probability of side-effects and to increased costs.[3]
A major limitation to the effective use of inhaled medications is the inability of many patients to use various inhaler devices correctly. Patients require appropriate education in the correct handling of inhaled medications. Undoubtedly, the prescribing physician bears the primary responsibility for this task. However, other clinicians, nurses, Pharmacists and other health-care providers should be conversant with the correct sequence of inhaler use as they are required to check and recheck the correctness of the technique during patients initial and subsequent follow-up visits.[4] Patients are often given the medications without proper detailing/instructions on the correct technique of use because the provider may not be conversant with the technique.[5,6] In an Italian study, misuse of pMDI and DPI was significantly associated with less education and less instruction by health-care personnel.[4]
Several studies have shown that poor use of inhalers by patients is very common.[6,7]
Studies have shown variations in the ability of patients to perform all thesteps of inhalation techniques properly. Investigators working in some areas have estimated that between 14% and 89% of patients seen for the first time will use their inhalers sub-optimally.[3,8] For both types of inhalers, misuse was significantly and equally associated to increased age.[4]
Literature review shows that there is a paucity of data on studies evaluating the correct use of inhaler techniques among asthma patients in Nigeria and Africa in general, hence the need for such a study. This study therefore aims to evaluate the use of inhaler technique among asthma patients in a developing country like Nigeria and to identify the determinants of poor inhaler technique with a view to proffering solutions on how to improve the inhaler use among the growing number of asthma patients on inhaled medications.
Subjects and Methods
Study design
This was an observational cross sectional study. Asthma patients attending the Medical and General out-patient’s clinic of UNTH Ituku-Ozalla and University of Ilorin Teaching Hospital (UITH) between June 2011 and January 2012, who consented to the study, were consecutively recruited into the study if they were already using inhaler medications. Data were collected on the patient’s socio-demographic, asthma history, current asthma control, history of inhaler technique education and type of medication use information. Thereafter, an inhaler administration checklist[1] was then used by the investigators to assess the technique of use of the inhalers. The checklist was ticked, while the patient was observed using the inhaler medications. Patients were subsequently educated on how best to use the medications if mistakes were identified.
For the pMDI, a checklist comprising nine steps was used and they include:[1]
1. Take the cap off the inhaler mouthpiece
2. Shake the inhaler
3. Hold the inhaler upright
4. Breathe out
5. Place the inhaler mouthpiece between the lips and the teeth; keep the tongue from obstructing the mouthpiece
6. Trigger the inhaler while breathing in deeply and slowly
7. Continue to inhale until the lungs are full
8. Hold the breath while counting to 10
9. Breathe out slowly.
For the DPI, the Diskus which is the most common DPI device available in our country was used as the prototype. A checklist of nine steps was used to check for the ability to use it correctly and they include:
1. Open the device
2. Slide the lever away until it clicks
3. Keep device level while inhaling
4. Exhale deeply, away from the mouthpiece
5. Put mouthpiece between teeth and close lips around
6. Inhale deeply and forcefully
7. Hold breath for 10 s
8. Remove Inhaler from the mouth without exhaling into it
9. Breathe out slowly.
The technique of use was classified as inaccurate or improper if the patient committed at least one error or was unable to demonstrate any of the nine steps properly (or by refusing even to try).
Study setting
The study was carried out in two teaching hospitals in Nigeria. The University of Nigeria Teaching hospital Ituku-Ozalla is in the Southern part of Nigeria while the UITH is in the Northern part of the country. Both hospitals offer primary, secondary and tertiary health services and have at least two respiratory physicians per institution.
Ethical approval
Ethical approval was obtained from the Research and ethics committee of the UNTH Enugu and UITH Ilorin.
Sample size
All the patients who met diagnostic criteria recommended by global initiative on asthma[9] and were previously on inhaler medications and consented to the study were consecutively recruited during one year study period.
Data analysis
Data obtained were analyzed using SPSS statistical software version 15 (SPSS Inc., Chicago, IL, USA). Frequency and descriptive statistics were used to analyze the general characteristics of the patients. Data was presented in tables and figures.
Pearson’s Chi-square was used to determine the significance of the factors that affected the correct use of the inhaler devices.
Factors that were found to be significantly related to completion of all steps of inhalation technique by the Pearson’s Chi-square analysis were subjected to logistic regression analysis to determine if those factors significantly predicted the completion of inhalation technique. In all, P < 0.05 was considered to be significant.
Results
A total of 140 patients were recruited during the study period. The general characteristics of the patients are shown in Table 1. There were 46.4 % 65/140) males and 53.6%(75/140) females. Their mean age was 47.6 (21.2) years and 60% (84/140) of them were married. Majority had primary education followed by those with tertiary education.
| Variable | N (%) |
|---|---|
| Gender | |
| Male | 65(46.4) |
| Female | 75(53.6) |
| Age (years) | |
| Mean (SD) | 47.6 (21.2) |
| Marital status | |
| Single | 45(32.1) |
| Married | 84 (60) |
| Divorced/separated | 4(2.9) |
| Widowed | 7 (5) |
| Educational status | |
| No formal education | 4(2.9) |
| Primary | 68(48.6) |
| Secondary | 21(15.0) |
| Tertiary | 46(33.6) |
| Inhaler device used | |
| pMDI | 140 (100) |
| DPI | 51(36.4) |
| Confidence of use of the inhalers | |
| Very confident | 113 (80.7) |
| Not too confident | 27(19.3) |
| Instruction on inhaler technique | |
| By a health-care provider | 128 (91.4) |
| Not by a health-care provider | 12 (8.6) |
| Asthma medications | |
| Salbutamol inhaler | 129 (92.1) |
| Steroid+beta agonist inhaler | 99(70.7) |
| Anti-cholinergic inhaler | 4(2.9) |
| Inhaler medications alone | 101 (72.1) |
| Inhaler medications plus prednisolone, salbutamoland dexamethasone tablets | 39(27.9) |
| Median duration of use of inhalers (months) | 24 |
Table 1: Characteristics of the 140 patients studied
About 50% (71/140) of the asthma patients recruited had asthma symptoms for < 3 years. Nearly 57.9% (81/140) of the patients had monthly symptoms; the rest had daily or weekly symptoms and about 82 (58.6%) of all the subjects considered their asthma well-controlled.
All the patients in this study were already using pMDI and were checked on pMDI, while 36.4% (51/140) of them also made use of DPIs (Diskus) concurrently. The median duration of the use of the inhalers is 24 months and the majority of the patients (90.7%) had used inhalers for at least 3 months. 113/140 (80.7%) were confident on the use of inhalers. 92.1% (129/140) of the patients were on Salbutamol inhaler, while 99/140 (70.7%) were on combined steroid and long acting beta agonist inhaler and only 2.9% (4/140) were on anticholinergic inhaler medications. About128 (91.4%) of the patients had been taught on how to use the inhalers. Instruction on inhaler technique was received predominantly from doctors, which accounted for 75.7% (106/140) of patients source of instruction. About 3.0% (4/140) of patients obtained instruction only from literature; other sources of obtaining information on the use of inhalers include from Pharmacists 5.0% (7/140), nurses 0.7% (15/140) and non-health-care personnel 5.7 (8/140) On the whole, 72.1% (101/140) of the patients received inhaler-administered medications alone, while 27.9% (39/140) in addition received medications such as oral prednisolone, aminophylline, dexamethasone and salbutamol, in various combinations at different times [Table 1].
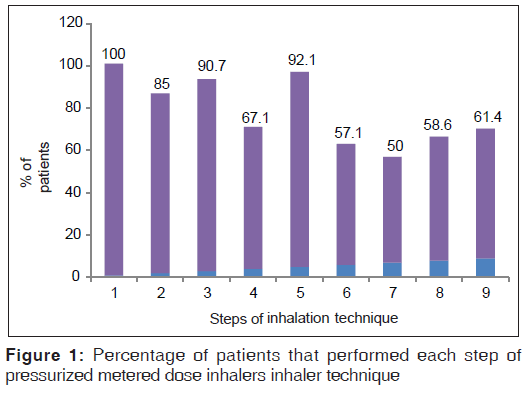
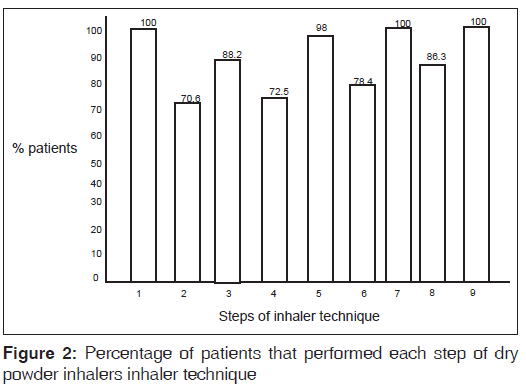
Evaluation of the technique of use of pMDI using the nine-step checklist showed that about half the number of the patients (70/140) did not “continue to inhale until the lungs are full;” but all did “take the cap off the inhaler mouthpiece” [Figure 1]. Similar evaluation for DPI users using DPI specific nine-step check list showed that all were able to “open the device,” “hold breath for 10 s,” and “breath out slowly” [Figure 2].
Only 22.1% (31/140) of the patients completed the nine steps in the inhaler technique checklist for pMDI. For DPI 37.3% (19/140) completed the nine steps [Table 2]. When pMDI and DPI were considered as together, 26.2% (37/140) of the patients completed the nine steps. Significantly greater percentage of DPI users completed the nine-step technique compared with pMDI users (P = 0.04), as shown in Table 2.
| Inhaler device | Complete inhaler technique N (%) | Incomplete inhaler technique N (%) | TotalN (%) | P value* |
|---|---|---|---|---|
| pMDI | 31 (22.1) | 109 (77.9) | 140 (100.0) | 0.04 |
| DPI | 19 (37.3) | 32 (62.7) | 51 (100.0) |
Table 2: Comparing the proficiency of inhaler technique steps performed by DPI and pMDI users
When subjects that completed the nine-step inhaler technique for the pMDI were compared with those that did not complete the nine steps, those with tertiary educational qualifications (P < 0.01) and those with monthly asthma symptoms (P < 0.01) were more likely to use the inhaler technique more accurately than their counterparts [Table 3].
| Characteristic | Complete steps N (%) | Incomplete steps N (%) | Total N (%) | χ2 (P value)* |
|---|---|---|---|---|
| Sex | 31(22.1) | 109 (77.9) | 140 (100) | 0.954 (0.33) |
| Male | 12(18.5) | 53 (81.5) | 65 | |
| Female | 19(25.3) | 56 (74.7) | 75 | |
| Educational status | 31(22.1) | 109 (77.9) | 140 (100.0) | 18.643 (<0.001) |
| No formal education | 0(0.0) | 4 (100.0) | 4 | |
| Primary | 7 (10.3) | 61 (89.7) | 68 | |
| Secondary | 11(52.4) | 10 (47.6) | 21 | |
| Tertiary | 13(27.7) | 34 (72.3) | 47 | |
| Confident in use of inhaler | 31(21.1) | 109 (77.9) | 140 (100.0) | 0.001 (0.99) |
| Very confident | 25(22.1) | 88 (77.9) | 113 | |
| Not confident | 6 (22.2) | 21 (77.8) | 27 | |
| Source of instruction | 31(22.1) | 1.09 (77.9) | 140 (100.0) | 7.938 (0.09) |
| Doctor | 22(20.8) | 84 (79.2) | 106 | |
| Pharmacist | 0(0.0) | 7 (100.0) | 7 | |
| Nurse | 5 (33.3) | 10 (66.7) | 15 | |
| Non health-care person | 4 (50.0) | 4 (50.0) | 8 | |
| Literature | 0(0.0) | 4 (100.0) | 4 | |
| Frequency of symptoms | 31(22.1) | 109 (77.9) | 140 (100.0) | 9.900 (<0.01) |
| Daily | 0(0.0) | 24 (100.0) | 24 | |
| Weekly | 12(34.3) | 23 (65.7) | 35 | |
| Monthly | 19(23.5) | 62 (76.5) | 81 |
Table 3: Completion of pMDI inhaler technique steps performed according to specified characteristics
For the DPI, those who felt they were confident on the use of inhalers (P = 0.03) and those who had previously received instructions on how to use the inhalers from a doctor (P < 0.01 were more likely complete the steps of the technique than their corresponding counterparts [Table 4].
| Characteristics | Complete N (%) | Incomplete N (%) | Total N (%) | χ2 (P value) | |
|---|---|---|---|---|---|
| Sex | 19(37.3) | 32 (62.7) | 51 (100) | 0.844 | (0.36) |
| Male | 10(32.3) | 21 (67.1) | 31 | ||
| Female | 9 (457) | 11 (55) | 20 | ||
| Education | 19(37.3) | 32 (62.7) | 51/100 | 0.110 | (0.74) |
| Primary | 11(31.3) | 17 (60.7) | 28 | ||
| Post primary | 8 (34.8) | 15 (65.2) | 23 | ||
| Confident in use of inhaler | 19(37.3) | 32 (62.7) | 51 (100) | 4.759 | (0.03) |
| Very confident | 18 (45) | 22 (55) | 40 | ||
| Not too confident | 1(9.1) | 10 (90.7) | 11 | ||
| Source of instruction | 19(37.3) | 32 (62.7) | 51 (100) | 10.145 | (<0.01) |
| Doctor | 15(41.7) | 21 (583) | 36 | ||
| Nurse | 0 (0) | 10 (100) | 10 | ||
| Others | 4 (80) | 1 (20) | 5 | ||
| Frequency of symptoms | 19(77.3) | 32 (62.4) | 51 (100) | 0.412 | (0.81) |
| Daily | 2 (33.3) | 4 (67.7) | 16 | ||
| Weekly | 455 | 6 (51.5) | 11 | ||
| Monthly | 12 (353) | 22 (64.7) | 34 | ||
Table 4: Completion of DPI inhaler technique steps performed grouped according to specified characteristics
When the variables that were significantly associated with completion of the different inhaler technique were subjected to logistic regression analysis, higher educational status was the only significant predictor of completion of pMDI inhalation technique (P < 0.001, odds ratio = 5.058, confidence interval 2.005-12.758) as shown in Table 5. Those with higher education were more likely to complete the technique.
| Variable | B | SE | P value | OR | 95% CI for OR | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Higher educational status (pMDI) | 1.636 | 0.472 | <0.001 | 5.058 | 2.005 | 12.758 |
| Monthly asthmasymptoms(pMDI) | 0.170 | 0.437 | 0.70 | 1.185 | 0.503 | 2.792 |
| Confident in theuse of inhalerdevice (DPI) | 2.025 | 1.102 | 0.07 | 7.578 | 0.874 | 65.715 |
| Inhalertechniquetaught by adoctor (DPI) | 0.468 | 0.711 | 0.51 | 1.597 | 0.396 | 6.435 |
Table 5: Logistic regression analysis showing the association between completion of the steps of inhaler technique and independent variables
Discussion
This observational study of 140 asthmatic patients showed that the vast majority of patients use their inhalers incorrectly, whether it is pMDI or DPI. It also showed that significantly more DPI users followed the correct sequence of steps required during inhalation than do pMDI users as documented earlier.[10] It equally showed that patient dependent factors like educational status affected completion of the inhaler technique steps.
Our study showed that only 22.1% of pMDI users and 37.3% of DPI users were able to complete all the steps in their different techniques. About 26.2% of both pMDI and DPI users completed the nine steps without mistakes. In the work by van Beerendonk et al. in the Netherlands,[11] only 11.1% patients completed the required steps. Our finding is consistent with that of Adeyeye and Onadeko working in Lagos State University Teaching Hospital, Lagos Nigeria;[12] 32% of the 106 asthmatic patients they studied performed all steps of inhalation technique. The 11.1% recorded by van Beerendonk et al. compared to 26.2% in our study may have resulted from studying a population with a higher mean age (61.83 [14.56]) as well as their finding that older patients had more difficulty with the correct use of the inhaler than younger patients. Adeyeye and Onadeko studied patients who were in the age range of 13-64, comparable with our study. However in contrast to our study, a systematic review of other previous studies showed that higher percentages of patients used their inhalers correctly; About 63% for metered dose inhalers (MDIs); 75% for breath-actuated MDIs; and 65% for DPIs.[13] The bulk of the data for that review were outside Africa, where education of patients on inhalation technique could probably have been better.
We found that DPI users made fewer mistakes than pMDI users during inhalation. The type of inhalator device is an important determinant of incorrect inhalation technique with most previous studies showing that DPI users were able to complete the steps better than pMDI users.[3,10] This is probably because pMDI device requires hand-breath co-ordination unlike DPI. One review of inhaler technique on the other hand concluded that there is no difference in the ability of patients to use DPIs or MDIs.[13] However, this finding was noted among patients who were supposedly taught the correct inhaler technique just before their ability to use an inhaler was assessed.
The factors that significantly affected pMDI inhaler technique in this study include education and frequency of asthma symptoms. Fewer percentages of patients with no formal or with primary education completed the steps of inhaler technique than did those with secondary and tertiary education. This is comparable to what was observed in an earlier study where poor inhaler technique was associated with less education.[4] Furthermore none of the patients with daily asthma symptoms completed the pMDI inhaler steps as compared those with weekly (34.3%) and monthly (23.5%) symptoms (P = 0.007). A previous study has documented higher rates of poor technique in DPI users with severity of airway obstruction.[14] Daily asthma symptoms may well be a consequence of poor inhaler technique since this would result in an ineffective drug delivery. Ineffective drug delivery of asthma medication due to incorrect use of an inhaler device has been associated with an uncontrolled asthma in recent study in Nigeria.[15]
Among DPI users, our study revealed that those who have been taught the use of the technique earlier by a doctor and those who felt that they very confident in their use completed the whole steps more than their counterparts. However, logistic regression analysis of these variables did not show that they were good predictors of completion of DPI inhalation technique.
It is however interesting to note that none of the patients using DPI who received the instructions by nurses could perform the technique correctly and equally those who received the instruction from Pharmacists could not perform the MDI technique correctly. This calls for a lot of concern because usually both nurses and Pharmacist are important health providers required to give instructions relating to inhaler use in well-organized asthma care units. We are of the opinion that these health-care providers should be continuously trained and retrained on the techniques of inhaler use.
Similar to our observation, Gray et al.[16] found no association between age, sex and prediction of incorrect pMDI among subjects with a mean age of 69.7 years. In contrast Goodman et al.[17] found that males perform significantly better than females in subjects aged 20-81 (mean 38 years). This difference may be related to the sample age range.
The most common errors in the use of pMDI in our study were step 7 (Continue to inhale until the lungs are full), followed by step 6 (Trigger the inhaler while breathing in deeply and slowly). For DPI the most common errors were step 2 (Sit upright or stand) followed by step 4 (Exhale deeply, away from the mouthpiece). These findings are consistent with those of van Beerendonk et al.,[11] who identified steps 7 and 4 as the most common “skill” and “non-skill” mistakes respectively. Similarly, other studies identified our steps 7 and 6 as the most common mistake made by patients using an MDI.[3,18,19] Indeed the most important aspect of inhalation technique in pMDI is a slow (< 60 L/min) and deep inhalation.[20]
This study however has some limitations; it was not possible to ascertain whether the inhaler technique, which patients had been taught by health practitioners prior to this study, was correct. Hence the impact of previous teaching of inhaler technique to patients was not assessed properly. The assumption that inhaler technique taught by any doctor or other health-care providers must be correct may not be true as studies have shown that health-care providers may not know how to use inhalers correctly.[5,6] This could form basis of future research which will assess the knowledge of the inhaler techniques among health-care practitioners that actually teach the patients how to use the inhalers.
Equally, some other significant determinants of an incorrect inhaler technique were not assessed in this study and include low score in mini mental state examination, poor hand grip strength[17] bronchodilator unresponsiveness, lack of additional teaching on proper inhaler technique, lack of patients perception of importance of inhaler use, low emotional quality-of-life and being treated in a general practice.[18]
Furthermore the small number of subjects studied may have affected some of the conclusions drawn from this study.
In spite of the limitations, this study has been able to assess inhaler techniques among selected asthma patients seen in a developing nation like Nigeria and was carried out in two major regions of the country and will no doubt add to the body of literature in this area of practice.
This study which is the first comprehensive study of this sort in a resource poor country like Nigeria is expected to generate future research in this novel area including assessment of health-care provider knowledge of correct inhaler technique. It will equally form bases of continued education of the patients who use these inhalers during their routine clinic visits.
Conclusion
Our study showed that majority of our asthma patients used their inhalers inaccurately. Patient-dependent factors were identified as the cause of incorrect technique of inhaler use. There is need for increased awareness among all the health-care personnel involved in asthma care most especially the Pharmacists ensuring they know the correct inhaler technique since most patients from our study were actually taught by doctors on the use of the inhalers.
We recommend that instructions on the use of the inhalers should be translated to several local languages for ease of understanding.
Asthma patients on inhalation medications should have their inhaler technique routinely checked during visits and should be given detailed education on proper inhalation technique if found to be poor.
References
- Rubin BK, Fink JB. Optimizing aerosol delivery by pressurized metered-dose inhalers. Respir Care 2005;50:1191-200.
- van der Palen J, Klein JJ, van Herwaarden CL, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. Eur Respir J 1999;14:1034-7.
- Inhaler Error Steering Committee, Price D, Bosnic-Anticevich S, Briggs A, Chrystyn H, Rand C, et al. Inhaler competence in asthma: Common errors, barriers to use and recommended solutions. Respir Med 2013;107:37-46.
- Sestini P, Cappiello V, Aliani M, Martucci P, Sena A, Vaghi A, et al. Prescription bias and factors associated with improperuse of inhalers. J Aerosol Med 2006;19:127-36.
- Stelmach R, Robles-Ribeiro PG, Ribeiro M, Oliveira JC, Scalabrini A, Cukier A. Incorrect application technique of metered dose inhalers by internal medicine residents: Impact of exposure to a practical situation. J Asthma 2007;44:765-8.
- Basheti IA, Qunaibi E, Bosnic-Anticevich SZ, Armour CL, Khater S, Omar M, et al. User error with Diskus and Turbuhaler by asthma patients and pharmacists in Jordan and Australia. Respir Care 2011;56:1916-23.
- Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: An observational study in 3811 patients in primary care. J Aerosol Med 2003;16:249-54.
- Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008;102:593-604.
- From the global strategy for asthma management and prevention, Global Initiative for Asthma (GINA) 2012. Available from: http://www.ginasthma.org/. [Last accessed on 2013 May 1].
- Rootmensen GN, van Keimpema AR, Jansen HM, de Haan RJ. Predictors of incorrect inhalation technique in patients with asthma or COPD: A study using a validated videotaped scoring method. J Aerosol Med Pulm Drug Deliv 2010;23:323-8.
- van Beerendonk I, Mesters I, Mudde AN, Tan TD. Assessment of the inhalation technique in outpatients with asthma or chronic obstructive pulmonary disease using a metered-dose inhaler or dry powder device. J Asthma 1998;35:273-9.
- Adeyeye OO, Onadeko BO. Understanding medication and use of drug delivery device by asthmatic in Lagos. West Afr J Med 2008;27:155-9.
- Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al. Comparison of the effectiveness of inhaler devices inasthma and chronic obstructive airways disease: A systematic review of the literature. Health Technol Assess 2001;5:1-149.
- Wieshammer S, Dreyhaupt J. Dry powder inhalers: Which factors determine the frequency of handling errors? Respiration 2008;75:18-25.
- Desalu OO, Fawibe AE, Salami AK. Assessment of the level of asthma control among adult patients in two tertiary care centers in Nigeria. J Asthma 2012;49:765-72.
- Gray SL, Williams DM, Pulliam CC, Sirgo MA, Bishop AL, Donohue JF. Characteristics predicting incorrect metered-dose inhaler technique in older subjects. Arch Intern Med 1996;156:984-8.
- Goodman DE, Israel E, Rosenberg M, Johnston R, Weiss ST, Drazen JM. The influence of age, diagnosis, and gender on proper use of metered-dose inhalers. Am J Respir Crit Care Med 1994;150:1256-61.
- Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care 2001;19:255-60.
- Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life andis associated with reduced disease control. Respir Med 2011;105:930-8.
- Pauwels R, Newman S, Borgström L. Airway deposition and airway effects of antiasthma drugs delivered from metered-dose inhalers. Eur Respir J 1997;10:2127-38.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.