Factors Associated with Practices of Recommended Lifestyle Modification among Hypertensive Patient
2 Department of Internal Medicine, Hawassa University, Hawassa, Ethiopia
Received: 18-May-2020, Manuscript No. AMHSR-23-10987; Editor assigned: 21-May-2020, Pre QC No. AMHSR-23-10987 (PQ); Reviewed: 04-Jun-2020 QC No. AMHSR-23-10987; Revised: 11-Aug-2023, Manuscript No. AMHSR-23-10987 (R); Published: 08-Sep-2023
Citation: Hirigo AT, Kibru S, Tesfaye S. Factors Associated with Practices of Recommended Lifestyle Modification among Hypertensive Patients. Ann Med Health Sci Res. 2023;13:774-781.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Proper adherence to recommended lifestyle change is a nonpharmacological option and plays great role to decrease comorbidity and expenditure of healthcare assets. Data regarding practices of recommended lifestyle change among hypertensive patients in Ethiopia is scarce. Therefore, this study aimed to assess practices of lifestyle change and its associated factors among diagnosed hypertensive patients.
Methods: This hospital-based cross-sectional study was conducted among 299 hypertensive patients in Hawassa University comprehensive, specialized hospital, Southern-Ethiopia from April to August 2019. A pre-structured interviewer-administered questionnaire was used to collect sociodemographic and clinical related data and study subjects were selected by systematic random sampling technique.
Results: The study indicated that only 37.8% (95% CI: 31.9-43.1) of the patients practiced recommended lifestyle changes. The study revealed the duration since the diagnosis of hypertension (Adjusted Odds Ratio (AOR)=2.3, 95% Confidence Interval (CI): 1.2-4.4), home blood pressure check-up (AOR=3.5, 95% CI: 1.7-7.1), hypertension controlling status (AOR=2.8, 95% CI: 1.6-5.4) and counseling (AOR=4.5, 95% CI: 1.7-11.7) were significantly associated with practice of lifestyle modification. Besides selfefficacy (AOR=2.4, 95% CI: 1.2-4.7), appointment follows up status (AOR=29.8, 95% CI: 1.8-52.2) and knowledge on hypertension and related consequences (AOR=4.3, 95% CI: 2.1-9.3) also were significantly associated with the practice of lifestyle change.
Conclusion: In general, this study revealed that the practices of lifestyle change among hypertensive patients were very low. Therefore, proper awareness creation and health education on the recommended lifestyle modifications might support patients to control their hypertension and to prevent comorbidity with different diseases.
Keywords
Hypertension; Healthy lifestyles; Adherence; Southern-Ethiopia
Abbreviations
CI: Confidence Interval; DBP: Diastolic Blood Pressure; ETB: Ethiopian Birr; HTN: Hypertension; NCDS: Non-Communicable Diseases; NGO: Non-Governmental Organizations; SBP: Systolic Blood Pressure; SPSS: Statistical Package For Social Sciences; WHO: World Health Organization
Introduction
Hypertension (HTN) is a progressive risk factor of cardiovascular diseases, which is characterized by raised both systolic and diastolic blood pressures. HTN is associated with serious complications like coronary artery disease, cerebrovascular accidents, congestive heart failure, renal failure and peripheral arterial diseases. According to the World Health Organization (WHO), HTN is defined as Systolic Blood Pressure (SBP) ≥ 140 mmHg and Diastolic Blood Pressure (DBP) ≥ 90 mmHg or individuals taking antihypertensive agents. HTN is one of the public problems and global prevalence in adults was about 1.13 billion with 24% in men and 20% in women in 2015. About 9.4 million deaths expected every year due to HTN complications in the world [1]. Besides HTN accounts for nearly 50% of coronary heart disease and 67% of the cerebral vascular problems. In Africa, HTN is one of the leading cause of heart failure and accounts for more than half of the deaths from stroke. The prevalence of HTN in developing countries, particularly in African was about 46% in adults and around 13.7% living in rural and 20.7% in urban areas of sub Saharan Africa. Several community-based studies in Ethiopia showed the prevalence ranging from 16.9% to 31.5%, while WHO revealed a 35.2% probability of being hypertensive in Ethiopia. Around 40% of adults aged ≥ 25 years were reported to have raised blood pressure in 2008, 15 and HTN is responsible for 3.5% of all types of deaths in Ethiopia [2].
Socio-demographic, economic, biological and behavioral characteristics, environmental, unhealthy lifestyle and rapid growth of urbanization, were risk factors of HTN. Therefore, effective lifestyle modification can lower blood pressure to the maximum use of single antihypertensive agent. Besides, interventions like reduce of tobacco utilization and alcohol consumption are an important limiting factor of HTN. Decrease in dietary sodium intake plays an important role to lower blood pressure. Conversely, poor practice to recommended lifestyle change is associated with comorbid illness and expenditure of health care resources [3].
The national Non-Communicable Diseases (NCDs) guideline of Ethiopia recommends both pharmacological and nonpharmacological interventions for hypertensive patients. However, non-pharmacological options can be prioritized and suggested for all patients who are found in any classes of hypertension. These healthy lifestyle modification include reduction of body weight to normal Body Mass Index (BMI), performing moderate-intensity physical activity, restriction of salt intake, avoiding behavioral factors and diet modifications [4].
However, studies are scarce on the practices of lifestyle modification among hypertensive patients in Ethiopian and the trend might vary from one place to another. Therefore, the finding of this study would create awareness for health professionals as well as other responsible bodies on the lifestyle modifications and associated factors with the practice of lifestyles in order to control hypertension before developing any complications [5].
Materials and Methods
Study setting and study population
This cross-sectional study was conducted in Hawassa university comprehensive specialized hospital, Southern- Ethiopia from April to August 2019. Hawassa is the capital city of the Southern-Ethiopia region and located 275 km away from Addis Ababa. This hospital established in November 2005 for the purpose of health professionals training and health care service delivery. Currently, it has more than four hundred beds and expected to serve more than 18 million population of Southern-Ethiopia and nearby regions. The source population was all hypertensive patients who were attending in the hospital, while adult hypertensive patients with age ≥ 18 years old were included in the study. However, unconscious and critically sick patients were excluded from the study [6].
Sample size determination and sampling technique
A single population proportion formula was applied using 23% of the practiced lifestyle modifications at 95% confidence interval and a 5% marginal error. In addition, 10% non-response rate was considered and then final sample size was calculated to be 299. Then, the study subjects were selected using a systematic random sampling technique [7].
Data collection and assessments
Data on socio-demographic, anthropometric, practices of lifestyles, individuals' knowledge of hypertension and patients' health status were collected by pre-structured questionnaire. The questionnaire concerning the measurement of practices of lifestyle modification was primarily prepared by adapting several studies and WHO stepwise surveillance questionnaires. In addition, clinical nurses who were working at chronic disease follow up clinic were measured the Blood Pressure (BP) and anthropometric variables. SBP and DBP were measured using Omron automatic blood pressure monitor after individuals rested for at least 5-10 minutes in the clinic. However, those patients who received caffeine or alcohol and those who did physical exercises at the time of clinic arrival were rested for 30 minutes before BP measurement [8].
Assessments
The healthy weight management: The weight was calculated as Body Mass Index (BMI) and it derived from individuals’ height and weight using standard measuring scales. Then an individual with a BMI range 18.5 kg/m2-24.9 kg/m2 was considered to have a good weight management practice.
A healthy salt diet: It was assessed by asking patients on the ingesting of non-salty foods or less than 6-gram salt per food palate. If the subjects utilized non-salty foods or less than half of the teaspoon salt per food palate were considered as having a good/healthy salt diet practice [9].
Healthy physical exercise: It was measured by performing activities with increase breathing or heart rate including brisk walking, jogging or running, riding a bicycle or exercise bicycle, swimming, aerobic exercise, aerobic dancing and the like. The requirement was doing one of the above-mentioned exercises for a minimum of 30 minutes per day; at least three times per week. If the patients responded yes answer to the exercise-related question considered as having a good physical activity practice.
Smoking: It was evaluated as self-report of never smoked or stopped smoking before 12 months. If a patient, who responded yes answer for never smoked or stopped smoking before 12 months were considered as a non-smoker/a good practice of smoking [10].
Alcohol consumption: Alcohol consumption frequency was assessed by 4 items and a score of (0-4 scale) depending on individuals response. That means 0 for never drink, 1 for drink less than monthly, 2 for drink monthly, 3 for drink weekly and 4 for drink daily or almost daily. If a patient who scored less than or equal to 3, considered as having a good practice of alcohol consumption.
Healthy diet allowance: Diet Allowance to Stop Hypertension (DASH) is a diet rich in fruits, vegetables, reduced saturated and total fat. The respondents were evaluated by asking questions like (do you eat fruit, vegetable, completely grain and low-fat diet a minimum of 3 times per week). If a patient, who responded yes answer was considered as having a good practice to diet recommendation [11].
Knowledge on hypertension and related consequences: All patients were asked whether the following statements were true or false to assess individuals knowledge like (high blood pressure can damage blood vessels and lead to heart attacks and strokes, being overweight affects blood pressure? Can salt consumption raises blood pressure? Can physical activity helps reduce blood pressure? Is the medication needed to treat hypertension). If a patient responded yes answer on ≥ 75% of the total knowledge questions was considered as having a good knowledge on hypertension and related consequences [12].
Self-Efficacy: it was evaluated based on self-efficacy for the managing chronic disease-item scale. It assesses a measure of how confident hypertensive patients with chronic disease are in doing their day-to-day activities. This assessment consists of 6 items were graded on a 10-point scale that starting from the lowest (not at all confident=1 point) to the highest (totally confident=10 points). The assessment scale is applied by calculating a mean score of total and as a minimum of four of the six items. If a patient, missing a maximum of two response items considered as having a good self-efficacy.
Practices of healthy lifestyle modifications: It was assessed by the six recommended lifestyles that were advised by a Joint National Committee (JNC) to prevent and manage hypertension. These include physical exercise, Diet Allowance to Stop Hypertension (DASH), moderation of alcohol intake, low dietary sodium intake, termination of smoking and maintaining a healthy weight of the body. If a patient who have adherences on a minimum of five items considered as “having agood practice of lifestyle modifications’’ while those who adherent for less than five items were considered as “having a poor practice of lifestyle modifications [13].
Data quality control
The pre-test was done on 10% questionnaires in Adare general hospital that is 5 km away from the study site. Then all necessary rearrangement of the questionnaire was done following pre-test feedback. Besides, training was given for data collectors (nurses who were working in the clinic) concerning the data collection approach and ways of blood pressure measurements.
Statistical analysis
Data coded and entered in to and analyzed using Statistical Package for Social Science (SPSS) version 22. Descriptive statistics were used to describe the study population with different variables. Bivariate and multivariate logistic regression analysis was used to evaluate the differences in the distribution of independent variables in comparison with the outcome variable. In addition, a variable with P-value <0.25 in the bivariate analysis was considered for multivariable analysis. Furthermore, the Hosmer-Lemeshow goodness-offit was evaluated for each variable in the logistic regression model. A p-value <0.05 was considered as statistical significance at 95% CI.
Results
Socio-demographic characteristics of the study population
Of 299 study subjects, more than half of 176 (58.9%) were females and the mean age of the study subjects was 51 (± 13) years. Two-hundred twenty nine (76.6%) of the study subjects were ≥ 40 years old. Majorities, 235 (78.6%) of patients were urban inhabitants and regarding educational status, 50 (16.7%) were unable to read and write and 93 (31.1%) were college and above. Two-hundred thirty nine (79.9%) of participants were married and 239 (79.9%) of subjects' monthly income was less than 3000 Ethiopian Birr (ETB) (Table 1) [14].
| Variable | Frequency | Percent | |
|---|---|---|---|
| Gender | Male | 176 | 58.9 |
| Female | 123 | 41.1 | |
| Age, years | 18-39 | 70 | 23.4 |
| 40-60 | 102 | 34 | |
| ≥ 60 | 127 | 42.5 | |
| Residence | Rural | 64 | 21.4 |
| Urban | 235 | 78.6 | |
| Education | Unable to read and write | 50 | 16.7 |
| Non-formal education | 44 | 14.7 | |
| Primary level (grade1-8) | 39 | 13 | |
| Secondary level ( grade 9-10) | 73 | 24.4 | |
| College or university | 93 | 31.1 | |
| Marital status | Single | 32 | 10.7 |
| Married | 239 | 79.9 | |
| Divorced | 13 | 4.3 | |
| Widowed | 12 | 4 | |
| Separated | 3 | 1 | |
| Occupational status | Government employed | 101 | 33.8 |
| NGO employed | 24 | 8 | |
| House wife | 64 | 21.4 | |
| Farmer | 37 | 12.4 | |
| Merchant | 34 | 11.4 | |
| Daily laborer | 8 | 2.7 | |
| Student | 3 | 1 | |
| Pensioner | 25 | 8.4 | |
| Other | 3 | 1 | |
| Monthly household income | <1000 ETB | 37 | 12.4 |
| 1000-1999 ETB | 89 | 29.8 | |
| 2000-2999 ETH | 113 | 37.8 | |
| ≥ 3000 ETB | 60 | 20.1 | |
| A distance of hospital from their residence | <5 km | 56 | 18.7 |
| 5 to 10 km | 62 | 20.7 | |
| >10 km | 181 | 60.5 | |
Note: ETH: Ethiopian birr; NGO: Non-Governmental Organization
Table 1: Socio-demographic characteristics of hypertensive patients.
Co-morbidities and other characteristics of the study subjects
Out of 299 study subjects, 162 (54.2%) have type-2 hypertension, 119 (39.8%) have type-1 hypertension and 18 (6%) have pre-hypertension. Thirty-seven (12.4%), 102 (34.1%), 155 (51.8%) and 5 (1.7%) of participants were obese (BMI: ≥ 30 kg/m2), overweight (BMI: 25 kg/m2-29.9 kg/m2), normal weight (BMI: 18.5 kg/m2-24.9 kg/m2) and underweight (BMI: <18.5 kg/m2), respectively. One-hundred ninety-one (63.9%, 95% CI: 58.7-69.2) of participants had a good knowledge of HTN and its related consequences. In addition, 52.5% (46.3-57.9) of the participants have controlled blood pressure with an acceptable limit. Regarding comorbidity, 85 (55.6%), have diabetes, 29 (19%) have cardiac diseases, 22 (14.4%) have neurological problems, 7 (4.6%) have asthma and 4 (2.6%) have HIV. Moreover, 112 (37.5%) had a family history of hypertension and 34 (11.4%) of patients were khat chewers (Table 2).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Years since the diagnosis of HTN | <2 years | 70 | 23.4 |
| 2 to 4 years | 102 | 34.1 | |
| >4 years | 127 | 42.5 | |
| Family history of HTN | Yes | 112 | 37.5 |
| No | 187 | 62.5 | |
| Comorbidity | Yes | 153 | 51.2 |
| No | 146 | 48.8 | |
| Type of comorbidity (n=153) | Diabetes | 85 | 55.6 |
| Cardiac disease | 29 | 19 | |
| Neurologic disease | 22 | 14.4 | |
| Asthma | 7 | 4.6 | |
| HIV/AIDS | 4 | 2.6 | |
| Other | 6 | 3.9 | |
| Blood pressure status during diagnosis | Pre-HTN (SBP 120-139/DBP 80 mmHg-89 mm Hg | 18 | 6 |
| Stage 1-HTN (SBP 140-159/DBP 90 mmHg-99 mmHg) | 119 | 39.8 | |
| Stage 2 HTN ( SBP ≥ 160/DBP ≥ 100 mmHg) | 162 | 54.2 | |
| Blood pressure status | Good control | 157 | 52.5 |
| Poor control | 142 | 47.5 | |
| Knowledge on HTN | Good | 191 | 63.9 |
| Poor | 108 | 36.1 | |
| Use of medication | Yes | 294 | 98.3 |
| No | 5 | 1.7 | |
| Number of medication | One | 164 | 55.8 |
| Two | 110 | 37.4 | |
| Three or more | 20 | 6.8 | |
| Counseling | Yes | 238 | 79.6 |
| No | 61 | 20.4 | |
| Self-efficacy | Good | 187 | 62.5 |
| Poor | 112 | 37.5 | |
| Regular follow-up | Yes | 268 | 89.6 |
| No | 31 | 10.4 | |
| Khat (Catha edulis leaves) | Yes | 34 | 11.4 |
| No | 265 | 88.6 | |
| Home blood pressure checkup | Yes | 206 | 68.9 |
| No | 105 | 35.1 | |
| Presence of stress | Yes | 107 | 35.8 |
| No | 192 | 64.9 | |
| Got social support | Not at all | 88 | 28.8 |
| A little | 114 | 38.1 | |
| Somewhat | 20 | 6.7 | |
| Very much | 79 | 26.4 | |
Note: AIDS: Acquired Immunodeficiency Syndrome; HIV: Human Immunodeficiency Virus; HTN: Hypertension; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure
Table 2: Co-morbidities and other characteristics of hypertensive patients.
The practice of recommended lifestyle modification
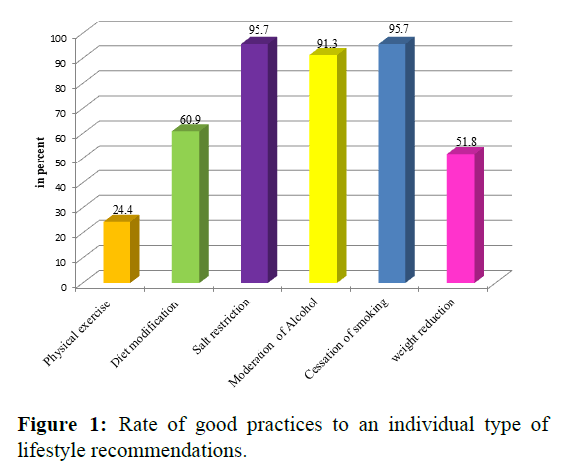
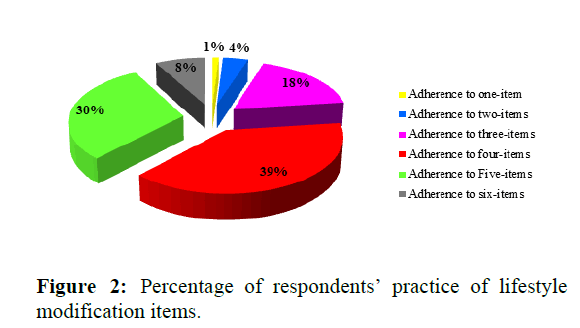
The overall 113 (37.8%, 95% CI: 31.9-43.1) patients practiced recommended lifestyle modification. Regarding patients practice, 286 (95.7%), 286 (95.7%), 273 (91.3%), 182 (60.9%), 155 (51.8%) and 73 (24.4%) have good practice on salt diet reduction, cessation of smoking, moderation of alcohol intake, diet modification, weight reduction and physical exercise, respectively (Figure 1). All patients practiced at least one item of lifestyle recommendations and only 24 (8%) practiced all six items of lifestyle recommendations (Figure 2) [15].
Factors associated with practices of recommended lifestyle modifications
Education (Crude Odds Ratio (COR)=1.7, 95% CI: 1.1-2.8), patients duration ≤ 4 years since the diagnosis of HTN (COR=2.3, 95% CI: 1.4-3.8), self-efficacy (COR=3.9, 95% CI: 2.2-6.7), appointment follow up status (COR=9.9, 95% CI: 2.3-42.4) and knowledge on HTN and related consequences (COR=8.0, 95% CI: 4.2-15.3) were associated with practice of lifestyle changes. In addition, home blood pressure check-up and overall control rates of hypertension were associated with the practice of lifestyle recommendations. While the multivariable analysis was adjusted for potential confounding factors and patients duration ≤ 4 years since the diagnosis of HTN was found to be 2 times more likely to be practiced recommended lifestyle modifications when compared to their counterparts (Adjusted Odds Ratio (AOR)=2.3, 95% CI: 1.2-4.4). Patients who had a trend of home BP check-up were 3 times more likely to be practiced recommended lifestyle recommendations when compared to their counterparts (AOR=3.5, 95% CI:1.7-7.1). Moreover, overall control rate of hypertension (AOR=2.8, 95% CI: 1.6-5.4), counselling of patients (AOR=4.5, 95% CI: 1.7-11.7), self-efficacy (AOR=2.4, 95% CI: 1.2-4.7), appointment follow up status (AOR=29.8, 95% CI: 1.8-52.2) and knowledge on HTN and related consequences (AOR=4.3, 95% CI: 2.1-9.3) also were significantly associated with practice of lifestyle changes (Table 3).
| Variable | Healthy lifestyle adherence | COR | AOR | ||
|---|---|---|---|---|---|
| (95% CI) | (95% CI) | ||||
| Adherent | Non-adherent | ||||
| Educational status | ≤ Primary level | 41 (13.7) | 92 (30.8) | 1 | 1 |
| Secondary and above | 72 (24.1) | 94 (31.4) | 1.7 (1.1-2.8)* | 1.6 (0.9-3.0) | |
| Duration since the diagnosis of HTN | 1-4 years | 79 (26.4) | 93 (31.1) | 2.3 (1.4-3.8)** | 2.3 (1.2-4.4)** |
| > 4 years | 34 (11.4) | 93 (31.1) | 1 | 1 | |
| Home BP checkup | Yes | 97 (32.4) | 109 (36.5) | 4.3 (2.3-7.8)*** | 3.5 (1.7-7.1)** |
| No | 16 (5.4) | 77 (25.8) | 1 | 1 | |
| Counseling | Counseled | 105 (35.1) | 133 (44.5) | 5.2 (2.0-10)*** | 4.5 (1.7-11.7)** |
| Not counseled | 8 (2.7) | 53 (17.7) | 1 | 1 | |
| BP controlling status | Good | 80 (26.8) | 77 (25.8) | 3.4 (2.1-5.6)*** | 2.8 (1.6-5.4)** |
| Poor | 33 (11.0) | 109 (36.5) | 1 | 1 | |
| Regular follow-up | Yes | 111 (37.2) | 157 (52.7) | 9.9 (2.3-42.4)** | 29.8 (1.8-52.2)** |
| No | 2 (0.7) | 28 (9.4) | 1 | 1 | |
| Social support | Supported | 54 (18.1) | 45 (15.1) | 2.9 (1.7-4.7)** | 1.2 (0.65-2.4) |
| Not supported | 59 (19.7) | 141 (141) | 1 | 1 | |
| Self-efficacy | Good | 91 (30.4) | 96 (32.1) | 3.9 (2.2-6.7)*** | 2.4 (1.2-4.7)* |
| Poor | 22 (7.4) | 90 (30.1) | 1 | 1 | |
| Knowledge on HTN | Good | 100 (33.4) | 91 (30.4) | 8 (4.2-15.3)*** | 4.3 (2.1-9.3)*** |
| Poor | 13 (4.3) | 95 (31.8) | 1 | 1 | |
| Khat chewing | Yes | 8 (2.7) | 26 (8.8) | 1 | 1 |
| No | 105 (35.1) | 160 (53.5) | 2.2 (0.95-5.0) | 066 (0.22-1.9) | |
Note: AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio; HTN: Hypertension; *: p<0.05; **: p<0.01; ***: p<0.001
Table 3: Factors associated with adherence to lifestyle modifications in hypertensive patients.
Discussion
The present study revealed 63.9% (95% CI: 58.7-69.2) of the participants had good basic knowledge concerning hypertension and related problems that are almost similar to the study conducted in the Jimma-Oromia region, Ethiopia, which was 67.7%. However, the finding is higher than the rate reported by different studies like 44.9% in Hosanna, South-Ethiopia, 34.9% in Nedjo, West Ethiopia and 12.9% in Egypt. A higher rate also was reported from Harar, Eastern Ethiopia that was 83.8%. From the study subjects, 52.5% (95% CI: 46.3-57.9) had the overall rate of controlled of hypertension and the finding is higher than the study conducted in Addis Ababa (41.1%), Northwest Ethiopia (42.9%), Eastern Ethiopia (22.2%), Southwest Ethiopia (22.4%) and survey of the USA (37%). This indirectly might reflect the adherence rate of hypertensive patients’ to therapeutic agents or practices of recommended lifestyle modification.
About 11.4% of the respondents were khat (Catha edulis leaves) chewers. The rate was lower than the study conducted in Harar, which was 33.7%. The differences might be attributed to the socio-cultural variations concerning the practice of khat chewing from place to place. The overall practices of lifestyle change among hypertensive patients were 37.8% (95% CI: 31.9-43.1). Conversely higher rate was reported from Northwest Ethiopia (77.3%), East Shewa, Ethiopia (59.5%), Southwest Ethiopia (60.5%), Eastern Ethiopia (62.1%) and Ghana (72%). Lower rates also were reported from different studies like 23%, 27.3% and 31.4%. The variations in practices of recommended lifestyle modification might be attributed to methodological differences, socioeconomic status of individuals, provision of health education, behavioral characteristics of individuals and willingness of individuals to act recommended lifestyle moderation.
The present study found that no statistical association between education and practices of lifestyle modality. Conversely, the study conducted in another part of South- Ethiopia and West Ethiopia revealed that the association between education and practice lifestyle modification. The variation may be attributed to differences in the classification of education level for the purpose of statistical analysis. The studies conducted in South Ethiopia, Addis Ababa and Ghana were reported the association between the duration since the diagnosis of hypertension and practices of lifestyle modality. This in line with the current study finding that revealed the experience of hypertension ≤ 4 years since its diagnosis was associated with the practices of lifestyle modification (AOR=2.3, 95% CI: 1.2-4.4).
In addition, those patients who had basic good knowledge on hypertension and its consequences were 4 times more likely to be practiced lifestyle modification (AOR=4.3, 95% CI: 2.1-9.3) when compared to poor-knowledge patients. In similar studies conducted in Addis Ababa, West Ethiopia and South West Ethiopia reported a significant association between patients’ knowledge and practices of recommended lifestyle change. However, this study indicated no association between residence and practice of recommended lifestyle change. The finding is inconsistent with the study reported from West Ethiopia and Addis Ababa. Moreover, Tibebu et al. reported that the association between self-efficacy and practices of lifestyle change, and this in line with the finding of the current study (AOR=2.4, 95% CI: 1.2-4.7). Social support was not associated with the practices of recommended lifestyle modification in this study and the finding is not in line with the study conducted in Addis Ababa. The variation might be attributed to the differences in social support approach from culture to culture and the sympathetic level of individuals.
One study revealed the association of gender and occupation with the practice of lifestyle modification, In addition, Obirikorang et al. reported the association between marital status and the practice of lifestyle modifications. However, the present study revealed no association gender, marital status and occupation with the adherence of practice of lifestyle change.
Good control rate of hypertension upsurges adherence to the healthy lifestyle modalities. This is consistent with the finding of the present study. Furthermore, almost 75% of people living with hypertension in developing countries with limited resource settings have low awareness of hypertension control rate. Therefore, hypertension control status plays a critical role to avoid its side effects.
Conclusion
This study revealed the practice of recommended lifestyle modification among hypertensive patients was very low. Duration since the diagnosis of HTN, home-based BP checkup, counseling, overall hypertension controlling status, the status of social support, self-efficacy and knowledge on HTN were important significant predictors of adherence to practices of lifestyle modifications. Therefore, proper awareness creation and health education on the recommended lifestyle modifications might support patients to control their hypertension and to prevent comorbidity with different diseases.
Limitations of the Study
The practices of lifestyle modification in hypertensive patients was assessed using only patients’ responses alone. The other limitation was the cross-sectional nature of the study that signifying it cannot provide adequate evidence of association about practices of lifestyle modification. Irrespective of the described limits, this study eventually adds helpful information on practices of lifestyle modification in an inadequate situation of Ethiopia.
Data Sharing Statement
The data set of this article is not openly accessible, but it can be accessible on reasonable request from the corresponding author with the permission of the clinical and academic director of Hawassa university’s comprehensive specialized hospital clinical.
Author Contributions
All stated authors participated in the research project. SK hypothesized and designed the study did data collection including data analysis; ST was the main advisor throughout the project and ATH did required data analysis, manuscript preparation including with manuscript review. All authors read and approved the final version of the manuscript.
Funding
The study fiscally supported by Hawassa university college of medicine health science.
Disclosure
The authors declare that they have no competing interests in this work.
Acknowledgments
We want to acknowledge the nurses who were working in the cardiac clinic of Hawassa university comprehensive specialized hospital. Further, our appreciation is also extended to hypertensive patients for their willingness to involve in the study.
Ethics Approval and Consent to Participate
The study was approved by the Institutional Review Board (IRB) of Hawassa university college of medicine and health sciences (IRB-2019). All the study participants were well known about the protocol of the study and written informed consent was obtained from study participants. In addition, the confidentiality of the participants’ information was well kept.
References
- Giles TD, Materson BJ, Cohn JN, Kostis JB. Definition and classification of hypertension: An update. J Clin Hypertens. 2009;11:611-614.
[Crossref] [Google Scholar] [PubMed]
- Zhou B, Bentham J, di Cesare M, Bixby H, Danaei G, et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37-55.
[Crossref] [Google Scholar] [PubMed]
- Tibazarwa KB, Damasceno AA. Hypertension in developing countries. Can J Cardiol. 2014;30:527-533.
[Crossref] [Google Scholar] [PubMed]
- Twagirumukiza M, de Bacquer D, Kips JG, de Backer G, Vander Stichele R, et al. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: An estimate from population studies. J Hypertens. 2011;29:1243-1252.
[Crosref] [Google Scholar] [PubMed]
- Abebe SM, Berhane Y, Worku A, Getachew A. Prevalence and associated factors of hypertension: A crossectional community based study in Northwest Ethiopia. PloS One. 2015;10:0125210.
[Crossref] [Google Scholar] [PubMed]
- Anteneh ZA, Yalew WA, Abitew DB. Prevalence and correlation of hypertension among adult population in Bahir Dar city, northwest Ethiopia: A community based cross-sectional study. Int J Gen Med. 2015;8:175-185.
[Crossref] [Google Scholar] [PubMed]
- Asfaw LS, Ayanto SY, Gurmamo FL. Hypertension and its associated factors in Hosanna town, Southern Ethiopia: Community based cross-sectional study. BMC Res Note. 2018;11:1-6.
[Crossref] [Google Scholar] [PubMed]
- Awoke A, Awoke T, Alemu S, Megabiaw B. Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: A community based cross-sectional study. BMC Cardiovascular Dis. 2012;12:1-6.
[Crossref] [Google Schoalr] [PubMed]
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438-1447.
[Crossref] [Google Scholar] [PubMed]
- Mtabaji JP, Moriguchi Y, Nara Y, Mizushima S, Mano M, et al. Ethnic differences in salt sensitivity: Genetic or environmental factors? Clin Exp Pharmacol Physiol Suppl. 1992;20:65-67.
[Google Scholar] [PubMed]
- Ambaw AD, Alemie GA, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;12:1-6.
[Crossref] [Google Scholar] [PubMed]
- Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adhere. 2017:323-330.
- Hareri HA, Abebe M, Asefaw T. Assessments of adherence to hypertension managements and its influencing factors among hypertensive patients attending black lion hospital chronic follow up unit, Addis Ababa, Ethiopia-a cross-sectional study. Int J Pharma Sci Res. 2013;4:1086.
- Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, et al. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br J Nutr. 2015;113:1-5.
[Crossref] [Google Scholar] [PubMed]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effect Clin Pract. 2001;4:256-262.
[Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.