Gingival Recession in a Child‑Patient; Easily Missed Etiologies: Case Report with Video
- *Corresponding Author:
- Dr. Solomon Olusegun Nwhator
Department of Preventive Dentistry , University of Abuja Teaching Hospital, Abuja, Nigeria.
E-mail: periodontologist2010@ gmail.com
Abstract
Gingival recession is commonly associated with plaque‑induced inflammation and calculus. A high frenal attachment is more important in gingival recession in the child‑patient. A healthy child‑patient with impeccable oral hygiene presented with localized gingival recession without plaque‑induced inflammation which led to the exploration of other possible etiologies. Multiple factors appeared to be acting in consonance (Concomitant multiple etiologies [CME]). The factors were a high frenal attachment, traumatic overbite and bruxism induced by premature tooth contacts. Pedodontists and periodontists should rule out CME in cases of gingival recession in the child‑patient.
Keywords
Bruxism, Gingival recession, Traumatic overbite
Introduction
Gingival recession – the apical migration of the marginal gingiva[1] - results from several factors. In a study of historical interest, Baker and Seymour[2] suggested plaque-induced inflammation as an important cause of gingival recession. Determinants of gingival recession identified among Nigerians were age, calculus, high frenal attachment and bleeding on probing. Many factors affect prevalence but only age and frenal attachment co-influenced both prevalence and severity of gingival recession.[3]
Gingival recession is uncommon in the child patient[4,5] and where present, is more prevalent in the mandibular incisor region. In an extensive survey of recession in mandibular central incisors of 1800 children, Mathur et al. reported a prevalence of only 18%[5] with no differences in prevalence by age and gender. Frenal attachment (the thin variety) significantly associates with prevalence of recession.
A lingering controversy regarding possible etiologies of recession is notable in literature. One school of thought completely denies the existence of “true” recession in children. This gave rise to the appellation of “apparent” gingival recession as described by Woofter.[6] He dismissed recession in children as a mere indication of delayed maturity of the gingival cuff of the adjacent paired tooth and not a “true” recession of the affected tooth - an observation lacking scientific evidence.
Of great interest is the role of high frenal attachment and associated retraction of the gingival margin during normal oral function as observed in several previous studies.[3-6] Although the controversy lingers, is it possible that we are overlooking recessions resulting from multiple etiologies of differing impacts?
Case Report
General evaluation
The mother of a 9-year-old boy on referral to the specialist periodontal clinic of a Nigerian teaching hospital was not happy with the appearance of a mandibular tooth. Preliminary medical and dental history revealed a healthy 9-year-old boy with age-appropriate complement of teeth except for a missing tooth 42.
Periodontal evaluation
Periodontal evaluation revealed a healthy mouth with good oral hygiene and absence of inflammation. A localized Miller’s class II gingival recession was present on the labial surface of tooth 31. The affected tooth (31) was asymptomatic with no plaque or calculus accumulation and there was neither associated inflammation nor bleeding on probing.
A high frenal attachment was found in relation with a thin labial frenum inserted into the mesial marginal gingiva of tooth 31. Gentle retraction of the lower lip revealed gingival retraction and blanching of the labial marginal gingiva related to tooth 31. The gingivae of the adjacent 32 and 41 were at the same level and appeared clinically healthy. Tooth 31 appeared healthy.
Orthodontic evaluation
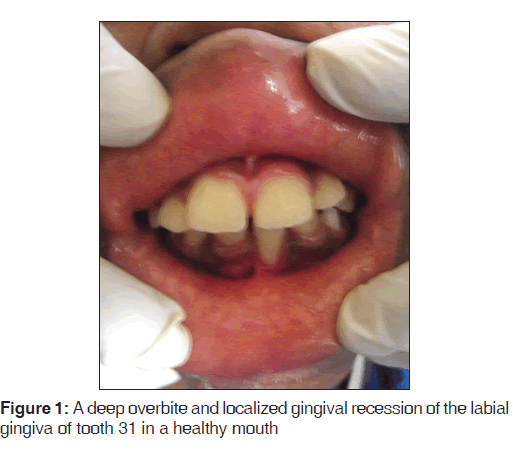
The child’s occlusion was Angle’s class I division 1 malocclusion complicated by an increased over jet and deep overbite [Figure 1]. The authors observed an unusual pattern of closure with a transient deviation to the right before going into centric occlusion.
The first contact in occlusion was a simultaneous contact between teeth 11-41 on the right and teeth 21-32 on the left. The affected tooth (31) was spared during this initial contact. Once in full occlusion, the jaws occlude in centric position with no apparent right mid-line shift despite the absence of tooth 42. A close observation of the child while “off-guard” revealed a bruxism habit of maxillary incisors teeth against the mandibular incisors.
Approval
Informed verbal consent and approval was only obtained from the patient’s mother to obtain pictures and videos. Full explanation was offered to the child’s mother that the child’s pictures and video would not in any way identify the child. The mother was shown the picture and she approved of them.
Video assessment
The closing pattern of the child-patient recorded on Video (video 1) shows a right shift of the midline on closure. Premature contacts between teeth 32-21 and teeth 11-41. Tooth 31 appeared spared in the video recording but close observation of the child-patient prior to this video recording had revealed a bruxism habit related to the tooth.
Contribution to knowledge
None of the facts presented here - high frenal attachment, traumatic overbite and bruxism secondary to premature tooth contact-is new. Authors do not intend to present these factors as novel – they are not. Our intention is to highlight the action of these factors in consonance - and reflect on how many cases we have missed in search of “obvious” factors.
Discussion
The role of plaque-induced inflammation in the etiology of gingival recession is established in literature.[3,7,8] However, it was inconsequential in the child-patient seen in this report – a 9-year-old with impeccable oral hygiene. Tooth 31 was well-aligned and hence the so-called gingival abrasion did not play a role. The fact that the two adjacent teeth were spared rules out a possible role of brushing-induced gingival abrasion. Whatever was responsible was therefore likely to be local to tooth 32.
Again, the principle of differential gingival maturation of the adjacent tooth giving rise to the so-called “apparent” gingival recession as postulated by Woofter[6] appeared unlikely to play a role in this case. The gingival level of the two adjacent teeth (41 and 32) was the same while the gingiva of the affected tooth was about 3-4 mm short of the margin of the adjacent teeth.
The probable reason for the recession observed in the study can be explained under the theory of concomitant multiple etiology (CME) of differing impacts. First was the thin high frenal attachment into the mesial side of the labial marginal gingiva of tooth 31 with associated blanching and retraction of the marginal gingiva on lip retraction. This identified etiology corroborates literature as being more important than plaque accumulation as an etiological factor for gingival recession in children[4,9-11] and in the maxilla.[12]
High frenal attachment alone did not explain the pathology in this case report. Tooth 41 is also closely associated with the frenal pull but not affected by recession. Though there was no retraction of the marginal gingiva of 41 on manipulation of the lip, the complete absence of recession made the author to explore other causes acting concomitantly.
Malpositioning of teeth has been identified as important in the etiology of recession in children. While there was no obvious mispositioning in this instance, orthodontic forces might have played a role. A traumatic overbite of the mandibular incisors was not serious enough to cause stripping of the maxillary palatal gingivae of the opposing incisor.
The role of traumatic overbite observed in the current report corroborates observations by Ustun et al. They described a phenomenon of “muco-gingival stress” resulting from a traumatic deep overbite[13] which is also in consonance with a previous report.[14] Moreover, spontaneous resolution of mandibular gingival recession following treatment of traumatic overbite has been described.[15]
To further explore the concomitant factors at play, the patient was asked to close his mouth slowly. This revealed an unusual closure pattern that resulted in an initial right excursion of the occlusion before resting in centric occlusion. Sparing of tooth 31 did not fully explain the recession until the patient’s para-functional habit of grinding tooth 31 against the maxillary incisor (21) was observed [Figure 2].
Pradeep and Sharma[16] highlighted the neglected phenomenon of para-functional habit-associated gingival recession while Soto et al.[17] have reported a statistically higher prevalence of gingival recession amongst bruxers. Another reason supporting the role of bruxism in the present report is the premature contact linking bruxism with premature tooth contacts.[17-19] This occurs more with non-working side contacting on the same tooth as evident in the current report.[19]
In conclusion, the CME factors for recession in the current report were high frenal attachment, traumatic overbite and bruxism in decreasing order of importance. This order of importance is purely based on the objective evaluation of the patient but cannot be generalized. The patient was therefore referred for orthodontic treatment prior to a planned periodontal plastic surgery to correct the recession defect.
The main reason that led to further exploration of concomitant factors in the present report was the absence of plaque-induced inflammation and calculus. The contributory factors could have been missed if plaque-induced inflammation was present. Pedodontists and periodontists should rule out the role of concomitantly acting multiple etiological factors in gingival recession involving children. Although the concept of (CME) is not new, we must take care to identify these factors even in the presence of other “obvious” etiologies - that is the whole essence of this report.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Lindhe J, Karring T, Lang NP. Clinical Periodontology and Implant Dentistry. 3rd ed. Copenhagen: Munksgaard; 1998. p. 550-96.
- Baker DL, Seymour GJ. The possible pathogenesis of gingival recession. A histological study of induced recession in the rat. J Clin Periodontol 1976;3:208-19.
- Nwhator SO, Ogunbodede E, Adedigba M, Sagay D. Prognostic indicators of gingival recession in Nigeria: Preliminary findings. TAF Prev Med Bull 2010;9:187-94.
- Manchala SR, Vandana KL, Mandalapu NB, Mannem S, Dwarakanath CD. Epidemiology of gingival recession and risk indicators in dental hospital population of Bhimavaram. J Int Soc Prev Community Dent 2012;2:69-74.
- Mathur A, Jain M, Jain K, Samar M, Goutham B, Swamy PD, et al. Gingival recession in school kids aged 10-15 years inUdaipur, India. J Indian Soc Periodontol 2009;13:16-20.
- Woofter C. The prevalence and etiology of gingival recession. Periodontal Abstr 1969;17:45-50.
- Arowojolu MO. Gingival recession at the University College Hospital, Ibadan – Prevalence and effect of some aetiological factors. Afr J Med Med Sci 2000;29:259-63.
- Steiner GG, Pearson JK, Ainamo J. Changes of the marginal periodontium as a result of labial tooth movement in monkeys. J Periodontol 1981;52:314-20.
- Mumghamba EG, Honkala S, Honkala E, Manji KP. Gingival recession, oral hygiene and associated factors among Tanzanian women. East Afr Med J 2009;86:125-32.
- Lafzi A, Abolfazli N, Eskandari A. Assessment of the etiologic factors of gingival recession in a group of patients in Northwest Iran. J Dent Res Dent Clin Dent Prospects 2009;3:90-3.
- Kaimenyi JT. Occurrence of midline diastema and frenum attachments amongst school children in Nairobi, Kenya. Indian J Dent Res 1998;9:67-71.
- Al-Talib RA. The prevalence of gingival recessions and its association with the width of attached gingiva, oral hygiene status, gingival conditions and toothbrushing. Al-Rafidain Dent J 2004;4:119-27.
- Ustun K, Sari Z, Orucoglu H, Duran I, Hakki SS. Severe gingival recession caused by traumatic occlusion and mucogingival stress: A case report. Eur J Dent 2008;2:127-33.
- Gupta ND, Maheshwari S, Prabhat KC, Goyal L. A critical review of the management of deep overbite complicated by periodontal diseases. European J Gen Dent 2012;1:2-5.
- Pini-Prato GP, Cozzani G, Magnani C, Baccetti T. Healing of gingival recession following orthodontic treatment: A 30-year case report. Int J Periodontics Restorative Dent 2012;32:23-7.
- Pradeep AR, Sharma DC. Gingival recession and pathologic migration due to an unusual habit. J Int Acad Periodontol 2006;8:74-7.
- Soto A, Velasco - Neri J, Brihuega R, G”Mez C, Troyo-Sanroman R, Ramirez L. Association between bruxism and gingival recession, abfraction and premature contacts. The IADR/AADR/CADR 83rd General Session (March 9-12, 2005). Available from: http://www.iadr.confex.com/ iadr/2005Balt/techprogram/abstract_61038.htm. Last accessed on 28 December, 2013.
- Reyes E, Hildebolt C, Langenwalter E, Miley D. Abfractions and attachment loss in teeth with premature contacts in centric relation: Clinical observations. J Periodontol 2009;80:1955-62.
- Bedi S, Sharma A. Management of temporomandibular disorder associated with bruxism. J Indian Soc Pedod Prev Dent 2009;27:253-5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.