House Calls: Telepsychiatry with Patients with Intellectual Disability
Citation: Merrill B, et al. House Calls: Telepsychiatry with Patients with Intellectual Disability. Ann Med Health Sci Res. 2017; 7: 463-465
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Individuals with intellectual disability experience high rates of mental illness, and there is a lack of medical and mental health professionals in rural and underserved areas. Since patients with disabilities may not travel well or tolerate changes in routine, utilization of telepsychiatry is well suited to this patient population because it allows a highly traumatized group to meet with a psychiatrist from a location of their choice. Ohio’s Telepsychiatry Project for Intellectual Disability provides specialized mental health services to rural communities. After five years, over 1,000 complex needs patients with intellectual disability from 68 counties are engaged in the project.
https://maviyolculuk.online/
https://mavitur.online/
https://marmaristeknekirala.com.tr
https://tekneturumarmaris.com.tr
https://bodrumteknekirala.com.tr
https://gocekteknekirala.com.tr
https://fethiyeteknekirala.com.tr
Keywords
Telepsychiatry; Disability; Patients
Introduction
Ohio’s Telepsychiatry Project for Intellectual Disability was designed for individuals with multiple disabilities to access specialized psychiatric care in their home communities. Inclusion criteria for the project include diagnosis of co-occurring mental illness and intellectual disability. Many of the patients also have functional limitations and mobility problems in addition to limited financial and other resources. Patients must be Medicaid eligible or enrolled; case management assistance is available to navigate entitlements if needed. There are unique features of the program that better fit individuals with multiple disabilities, described below.
Virtual House Calls – Home-based services and the ability to practice psychiatry as it once was
In “Ghosts in the Nursery” we learn about the intergenerational transmission of despair and anger associated with past trauma and the direct link between a parent’s own childhood and the experience of oneself being a parent. [1] The power of this seminal piece lies in the effectiveness of the psychodynamic, home-based interventions. It is the mutual availability between psychotherapist and patient that resonates with the intimacy of entering a patient’s home and access to valuable clinical information that allows intervention in real time and in natural context.
While Fraiberg practiced in the mid-twentieth century; an era, which was undoubtedly different than our current landscape and with infant-mother dyads, as opposed to the older children and adults of our telepsychiatry project, her work provides both a conceptual framework and clinical imperative for home-based interactions. In addition the patients in our project have obstacles to attending appointments outside of the home, including excessive distance to the appointment, mobility impairments, and lack of transportation resources. Thus, we sought and gained exemption from The Centers for Medicare and Medicaid Services (CMS) to bill for our services from a patient’s home. Traditionally, telepsychiatry must be conducted from an “originating site” such as a physician’s office, a Federally Qualified Health Center, et cetera; but our project has the ability to see patients from a location of their choice. The logistical advantages of this arrangement are substantial. Patients can literally wake up moments before their appointment and not be late. Inclement weather is no impediment to obtaining services. Coordinating availability of the originating sites “telepsychiatry suite” is obviated. We could go on, but beyond these practical considerations are the valuable clinical implications. To witness a mother chain-smoking cigarettes and agitatedly cursing at the television and her husband in the background of the appointment of her son diagnosed with intellectual disability, who is experiencing his own issues with frustration-tolerance and anger, is enlightening and more importantly actionable. Intervening instantly with this mother, helping her see the direct link between her own negative emotions and her son’s symptoms, and helping her understand the immediately transmittable nature of this phenomenon was effective and improbable had she attended an office-based appointment as a more professional and better-behaved version of herself, as most humans are when they leave their home.
Therefore, borne out of patient convenience and practicality, our CMS exemption to provide home-based telepsychiatry services, in fact allows for vivid observations of parental phenomena that parallel our patients’ own difficulties and is accessible to the psychiatrist, the patient, and the parent as a “teachable moment” and opportunity for intervention. The CMS exemption has deepened and enriched our clinical experience.
Telepsychiatry to overcome expressive language limitations in individuals with intellectual disability
A common concern expressed to those practicing telepsychiatry is the perceived lack of the human connection between provider and patient. Another perceived barrier to care is the lack of expressive language that can co-occur in individuals with intellectual disability. A sense of adventure can easily overcome both these obstacles. Our team meets first in person, which serves to allay the interdisciplinary team’s concern of feeling disconnected from the psychiatrist and allowing for in-person alliance building. Interestingly, in a review of telepsychiatry, Hubley et al. [2] found that patient satisfaction and alliance was rated the same as face-to-face while the provider rating of the alliance was lower.
As discussed, one variable in telepsychiatry is working with software that allows for manipulation of the screen display. To build rapport for individuals with limited communication skills, the telehealth provider may offer a traditional videoconferencing set-up with the doctor in a large window and the patient and team in a smaller window. This allows the psychotherapist to pretend to be a giant person looming over the patient and team, which is good for rapport building and a laugh. Switching the display to the reverse with the patient and team in the larger window and the psychiatrist in the smaller window allows the patient to then take that role and experience increased agency in the appointment.
In the event that a patient is quiet or seems reluctant with the equipment, the provider can rely on the telehealth set-up’s similarity to television. If the provider creeps closer and closer to the camera, they appear larger and larger on the screen, and if they then tap the camera, to the patient it appears as though they are tapping on the inside of the television screen. Individuals with intellectual disability understand that the teleprovider is not actually in the television screen and generally are more interactive in the appointment after the proverbial ice has been broken.
Patients with limited expressive language appear to be engaged in watching themselves and team members on screen as well as the telehealth provider. While a few patients can navigate the software to connect via the internet, most patients require a team member to facilitate logging in and finding the patient’s private HIPAA compliant cyberlink. Once the appointment begins, all patients are able to participate. Some computers require certain activity before entering ‘sleep’ mode and quite a few patients are more than willing to move the electronic mouse to keep the session active. This participation encourages a more active role for the patient in his or her own treatment as well. Onsite intelligence technology support is helpful but not required. Difficulties with webcam, software updates, and hardware occasionally occur but routine maintenance of computers typically circumvents serious hindrances to care.
Web Cam Display Preferences
The prototype for the project involved ninety patients from 23 counties in Ohio seen at a Community Mental Health Clinic to determine if specialized psychiatric services would be a key factor in keeping patients in their home communities, decreasing emergency department visits, hospitalizations and admissions to state operated institutions. Over a five-year period, none of the ninety patients were hospitalized or readmitted to developmental centers. The patients were offered the option to transition to telehealth, which was optional, per patient/guardian consent and interest.
It was noticeable that some patients were more conversational via web cam, and less anxious versus being seen in an office setting, and some appeared to have improved eye contact. Some patients requested to talk to doctor one on one, as opposed to routinely having a caregiver or family member present when seen in the office setting. Collateral data from caregivers and summary of the appointment was navigated at the beginning and/or the end in these situations.
It is known that individuals with Autism Spectrum Disorders look less at eyes and more at the mouth compared to individuals who are neuro-typical. There are several potential explanations; is it possible the eyes are less meaningful? Threatening? Too stimulating? Fixation on mouth may be functional response related to early stages of normative language development. We are conducting a small research study to determine if introversion/extroversion and/or the etiology of the intellectual disability (Autism versus Down syndrome) are correlated to the web cam display preferences. Preliminary results show that patients with Autism are more often introverted and may prefer to look at themselves rather than their doctors; patients who were extroverted preferred to look at their doctors or a split screen. Viewing oneself may be less stimulating and anxiety producing; expanding this project to a larger number of subjects will reveal these nuances. Overall, studying web cam display preferences can add depth to our understanding of unique aspects of syndromes of ID and the cognitive and communicative strengths of this specialized patient population.
Conclusion
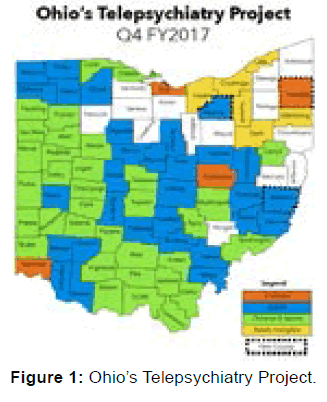
Patients with intellectual disability experience mental and medical illness at higher rates than the general population. Despite this, there is a great under-reporting of symptoms due at least in part to expressive language communication difficulties in patients with ID. Initiated in 2012, [3,4] Ohio’s Telepsychiatry Project for Intellectual Disability currently provides psychiatric care to over 1,000 patients with intellectual disability with complex needs from 68 of Ohio’s 88 counties. The result of the grant has been improved access to care, improved outcomes (including reduced emergency department visits and hospitalizations), and cost savings in the form of reduced travel expenses, reduced medical expense and long term services and support costs. The project has supported more than 200 patients transitioning from institutions in the state of Ohio. The unique aspects of this project and patient population may allow us to learn more about interpersonal interface in ID, benefit from a view into individual’s homes, and improve opportunities for effective communication. Telemedicine is an easy to use modality with clear benefits in the treatment of patients, especially those patients with co-occurring intellectual disability and mental health diagnoses living in rural areas [Figure 1].
Acknowledgements
The authors acknowledge grant support for the clinical project described from the Ohio Department of Mental Health and Addiction Services and the Ohio Department of Developmental Disabilities; no funding is associated with this article.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Fraiberg S, Adelson E, Shapiro V. Ghosts in the Nursery, Journal of the American Academy of Child Psychiatry, 1975; 14: 387-421.
- Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World Journal of Psychiatry. 2016; 6: 269-282.
- Gentile JP, Gillig PM (2012). Psychiatry of intellectual disability: Wiley and Sons, NY, USA.
- TCN Behavioral Healthcare Inc. Retrospective Chart Review, 2011.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.