Human Papillomavirus Screening: Study of HPV prevalence and cervical cancer in North Indian Women Population
2 Department of Obesity, Krishna Medical Center, Lucknow, India
3 Department of Biochemistry, Dr Ram Manohar Lohia Institute of Medical Sciences, Lucknow, India, Email: pratimatripathi.lko@gmail.com
, DOI: 10.54608.annalsmedical.2021.2
Citation: Misra M, et al. Human Papillomavirus Screening: Study of HPV prevalence and cervical cancer in North Indian Women Population. Ann Med Health Sci Res. 2021;11:1561-1565.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Genotyping of Human PapillomaVirus (HPV) has become a necessary criterion to establish a clear connection between the efficiency of HPV vaccine clinical trials and HPV prevalence worldwide. HPV infections contribute to 40%-60% of all known cancers and its screening and vaccination is an important aspect for a healthy life in females. Studies in North India Population have not been conducted yet in this regard. Materials & Methods: In this study, overall HPV prevalence and type specific prevalence were assessed in cervical smear of 2700 samples, using real time polymerase chain reaction for screening and linear array assay for genotyping. HPV status was studied in relation to age and other lifestyle factors. Results: Twenty per cent of samples were HPV positive. HPV type diversity was broad, and multiple strains of HPV infections occurred in half of the HPV positive samples. Younger women were significantly more likely to harbor multiple high risk HPV (HR-HPV) infections. Infections with high risk HPV types were found to be 41% of positive tested samples followed by 35% of moderate risk HPV types. The 41% infections were contributed by HPV type 16 and 18 alone. Conclusion: HR-HPV infections were most prevalent in North Indian women population due to multiple factors related to the marital and sexual life style of the subjects. Extensive cross-cultural study needs to be conducted to reach some scientific conclusion that will help the medical community in developing targeted therapeutics against HPV and thus will help in mitigating the burden of cervical cancer in the society.
Keywords
Human papilloma virus; Cervical cancer; HR-HPV
Introduction
Cervical cancer research has witnessed different approaches to tackle the issue in past few years. Pap smear test have helped a lot in the acceptance and early detection of cervical cancer, initiating a transition towards huge care in the management and prevention of this disease. Pap smear implementation since 1950 has significantly reduced the incidences of cervical cancer in several communities across the world with easily accessible high-quality screening programs. The occurrence and incidence of this cancer has remained high in the developing world in spite of huge screening and vaccination, due to lack the resources for widespread screening programs as compared to the developed nations. Human Papilloma Viruses (HPV) were etiologically linked to cervical cancer in the 1970s and the most important achievement in the field of cervical cancer was the understanding of its etiology and pathogenesis. This information further helped in development of HPV vaccine as a means of primary prevention and HPV assays for screening and secondary prevention. The availability of these interventional facilities may offer the possibility of bringing an economical strategy for cervical cancer prevention in the developing world. Since cervical cancer remains the second most common cause of death from cancer among women worldwide, accounting for more than 288,000 deaths each year there is an urgent need for such interventions. [1]
HPV infections are mostly sexually acquired that paves way for the virus to enter the skin and mucous membranes of the mouth, anus, penis and female reproductive tract. HPV infection ranges from 40%-60%, between sexual partners and may be affected by the length of marital age, number and length of sexual relationship, frequency of intercourse, use of contraceptives, and polyamory [1,2] as HPV infection is a sexually transmitted disease and can be easily passed on from an infected to another. [3] Probability for a new genital HPV infection in men within a year is 0.29-0.39, which is similar to previous estimates for women as proposed by some studies. [4,5] Transmission rate from a heterosexual partner to the other is estimated to be 3.7 cases per 100 person-months within a year. [6] HPVs are small, non-enveloped DNA viruses with over 150 types where HPV genotypes 16 and 18 are responsible for approximately 70% of cervical cancers and are considered to be high risk strains, while the remaining 30% cervical cancers are caused by other carcinogenic HPV types. [7-9] HPV16 is the most carcinogenic and is known to cause most of the complications associated with Cervical Intraepithelial Neoplasia (CIN). [10,11] While low-risk genotypes 6 and 11 are usually associated with genital warts. HPV infection accounts for approximately 8% of human cancer burden worldwide leading to approximately 500,000 invasive cervical cancer cases in women worldwide and 50% deaths associated with these cases due to lack of proper diagnosis and early prognosis. [12,13] Among HIV-infected homosexuals the incidence rates are even higher [14] since the introduction of Highly Active Anti-Retroviral Therapy (HAART). [15] Rate of anal cancer in HIV-infected homosexuals is higher than cervical cancer reported across the world. [16]
In a study conducted by National Health and Nutrition Examination Survey (NHANES), US in 2011, 4,000 women were investigated for types of HPV infections and cervicalvaginal specimens from more than where 37 different types of HPV were found to be positive with 42.5%, representing 40 million infections. [7] Despite their high prevalence, most cervical HPV infections are transient and asymptomatic and young women are more likely to clear infections readily than older women. [11] Negative oncogenic HPV test states a low risk condition of cervical intraepithelial neoplasia as compared to a positive oncogenic HPV test. Study confirms that rates of progression to cervical intraepithelial neoplasia ranges from 8% to 28% among women who do not clear their infection. [17] The transition to cancer usually takes years or decades; maximum incidences of HPV infection occurring around 20 years of age, and maximum cervical intraepithelial neoplasia incidences occuring at about 30 years ultimately leading to full grown cancer 40 years of age. [18] Cervical intraepithelial neoplasia/ cervical cancer in women with oncogenic HPV infection has been significantly associated with frequent smoking habits. [17,18]
In the present study the authors aimed at screening the North Indian Women population for HPV testing to identify the individuals at higher risk of developing cervical cancer and related medical issues that arise in the HPV positive patients if left unattended.
Material and Methods
In the present study, cervical scraping collected from 2700 women age 30 years-65 years, from north India were screened for 34 strains of HP virus by liquid-based cytology method between 1st April 2016 to 31st March 2019 at Krishna medical center, Lucknow and January 2018 till October, 2019 at Dr. Ram Manohar Lohia Institute of Medical Sciences, Lucknow, India. The demographic details of the subjects were collected as a routine work on their visit to the OPD. After the routine checkup in the OPD, pap smears of these subjects were collected and screened for HPV testing using PCR technique at both the Medical centers.
Specimen collection, preparation and testing of HPV DNA by liquid-based cytology method
Cervical scraping from the endocervical canal and ectocervix were collected with the help of brush from the patients in dorsolithotomy position and labelled for HPV testing by Liquid- Based Cytology (LBC). The smears were prepared from the cervical scrapings on glass slide and immediately fixed in 95% ethyl alcohol or the fixatives available commercially for 30 minutes which were later tested for detection of 34 strains of HPV DNA at KMC and DRMLIMS, Lucknow, India.
Statistical analysis
Percentage analysis technique was used for analysis of the data.
Results
Table 1 represents, the demographic details of the subjects enrolled in the current study. All the subjects of the study were north Indian married females aged 30 and more. As shown in the table, out of 2700 participants, 21.11% i.e. 570 subjects tested positive for various strains of HPV. Out of these 570 subjects who were screened positive for the HPV testing, 64.56% were the females married at an early age and 69.30% females had pregnancy before 30 years of age. 55.79% females had number of pregnancies more than 3 and 70.16% never used contraception. If we look at these factors it becomes very obvious that early marriage and pregnancy leads to more number of the latter along with the habit of avoiding contraceptives. All these factors are the major contributors of HPV infection and cervical cancer in the near future if left unattended.
| Sr. No. | Parameters | Participants of each criteria | Total HPV + ve (%) |
|---|---|---|---|
| 1 | Number of subjects | 2700 females | |
| 2 | Age | 30-65 years | |
| 3 | HPV testing + ve | 570 | 21.11 % of total screened cases |
| 4 | Marital age | ||
| >25 | 202 | 35.44% | |
| <25 | 368 | 64.56% | |
| 5 | Pregnancy age | ||
| >30 | 175 | 30.70% | |
| <30 | 395 | 69.30% | |
| 6 | No. of children | ||
| >3 | 318 | 55.79% | |
| <3 | 252 | 44.21% | |
| 7 | Contraception use | ||
| No | 400 | 70.16% | |
| Yes | 170 | 29.83% |
Table 1: Demographic details of subjects participated in the study.
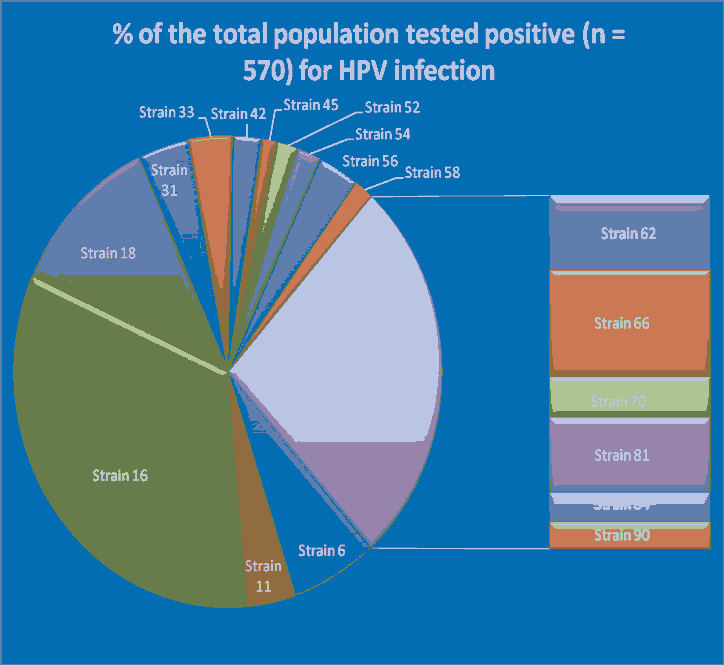
Table 2 represents the different strains of HP virus and the number of individuals tested positive for these strains. Out of the 2700 women subjects tested for 34 strains of HPV, 21.11% (570) subjects were found positive for different strains. Number of subjects for to be positive for strain 16 and 18 were 32%, and 11% respectively followed by strain 66, 6, 62, 81, 11, 31 and 70 where the number of HPV patients were 7.72%, 6.32%, 5.44%, 5.43%, 3.51%, 3.68% and 2.98% respectively. The individuals tested positive for these group of strains sum up to 35.08% of the total positive tested population. This shows that HPV strain 16 and 18 alone contributes to almost 41% of the cervical cancers and related complications in north Indian women population. Whereas, strains 6, 66, 62, 81, 11, 31 and 70 contributes to 35% of HPV positive cases that is still lower than the contribution made by strains 16 and 18 [Figure 1]. The strains contributing to 35% of positive tested cases can be considered as moderate risk groups or low risk group depending on other criteria of their prevalence while the other strains as shown in table 2 can be considered low risk types as the contribution by each of them doesn’t even cross 4% of the total positive cases [Table 2]. Number of patients tested positive for different strains of HPV. Total number of subjects enrolled in the study (N=2700).
| Sr. No. | HPV strain type | Number of patients tested positive for HPV Testing (total n = 570) | % of the total population tested positive (n = 570) for HPV testing |
|---|---|---|---|
| 1 | 6 | 36 | 6.32% |
| 2 | 10 | 1 | 0.18% |
| 3 | 11 | 20 | 3.51% |
| 4 | 16 | 181 | 31.76% |
| 5 | 18 | 63 | 11.05% |
| 6 | 31 | 21 | 3.68% |
| 7 | 32 | 1 | 0.18% |
| 8 | 33 | 18 | 3.16% |
| 9 | 35 | 3 | 0.53% |
| 10 | 39 | 2 | 0.35% |
| 11 | 40 | 2 | 0.35% |
| 12 | 42 | 12 | 2.11% |
| 13 | 44 | 2 | 0.35% |
| 14 | 45 | 6 | 1.05% |
| 15 | 52 | 9 | 1.58% |
| 16 | 53 | 5 | 0.88% |
| 17 | 54 | 10 | 1.75% |
| 18 | 56 | 17 | 2.98% |
| 19 | 58 | 8 | 1.40% |
| 20 | 59 | 1 | 0.18% |
| 21 | 62 | 31 | 5.44% |
| 22 | 66 | 44 | 7.72% |
| 23 | 67 | 3 | 0.53% |
| 24 | 68 | 1 | 0.18% |
| 25 | 70 | 17 | 2.98% |
| 26 | 73 | 1 | 0.18% |
| 27 | 81 | 30 | 5.43% |
| 28 | 82 | 4 | 0.70% |
| 29 | 83 | 2 | 0.35% |
| 30 | 84 | 12 | 2.11% |
| 31 | 87 | 2 | 0.35% |
| 32 | 89 | 3 | 0.53% |
| 33 | 90 | 11 | 1.93% |
| 34 | 91 | 1 | 0.18% |
| Total % of positive cases: 21.11% | |||
Table 2: Number of patients tested positive for different strains of HPV.
Discussion Cervical cancer and high-risk HPV infections have been found to be associated with the age of marriage below 18 years by 22-fold in India. [2] The risk of HPV infection has been found to be higher in women aged 25years-34 years (odds ratio, 1.11), in married women below 20 years of age (odds ratio, 1.80), and in women with parity ≥ 4 (odds ratio, 1.04) as shown in a study carried out by Dutta et al. This study coincides with our finding that an early age of marriage followed by maximum number of children increases the possibility of high-grade squamous intraepithelial lesion in the subjects, thus increasing the chances of cervical cancer. [19] Risk of HSIL/SCC cases increases with number of live births in HPV positive cases as per the study of Hildesheim et al. [20] In this study high HPV prevalence in women had been linked to age, duration of sexual activity and parity of women. Frequency of HPV infections has been found to be more in pregnant women than in non-pregnant women. [2] In India early marriages, and higher number of pregnancies, pose high risks of cervical cancer due to immature cervix. HPVs have been grouped into high-risk and low-risk HPV types on the basis of their association with cervical cancer and precursor lesions. Low-risk HPV types include types 6, 11, 42, 43, and 44. High-risk HPV types include types 16, 18, 31, 33, 34, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 and 70.
Infection with high risk (HR) HPV-16 and HPV-18 contributes to about 70% of cervical cancer cases worldwide. In India, occurrence of HPV type 16 associated cervical cancer is 70%-90% while that from HPV type 18 ranges from 3%-20% according to WHO Report. [1] Our study reported the need of a screening program with the possibility of early diagnosis because success of an HPV screening program primarily depends on a better understanding of the factors that determine a woman's willingness to participate in the screening. Awareness of the risks and factors associated with cervical cancer and the necessity of screening and vaccination program has been documented by other studies too. [19,20] Insufficient information or magnification of facts leads to anxiety and negligence associated with cervical cancer screening that emphasizes the need for dissemination of knowledge about this cancer to ensure the uptake of HPV screening and vaccination services. [21-24] Means of public communication such as mass media and commercials can be used to raise awareness and disseminate the correct knowledge with utmost sensitivity towards religious and cultural beliefs. [22] This could also be done with the help of trained non-medical personnel like accredited social health activist who are females and are from the same or nearby community. Proper knowledge and a timely screening followed by vaccination can prevent the occurrence of cervical cancer in huge number of females in reproductive age and thus can help them lead a successful, healthy and happy life ahead. This will help reduce the medical burden on the country’s economy as well.
Conclusion
Indian women continue to share a significant burden of invasive cervical cancer. HPV 16 and 18 is the predominant genotypes in both infected women who are symptomatic as well as asymptomatic for the HPV infection. Various risk factors other than HPV, like early marriage, no. of pregnancies and age are associated with the risk of progression from HPV infection to cervical cancer. Extensive cross-cultural study needs to be conducted to reach some scientific conclusion that will help the medical community in developing targeted therapeutics against HPV and thus will help in mitigating the burden of cervical cancer in the society.
Conflict of Interest
The authors declare that there is no conflict of interest to compete.
REFERENCES
- World Health Organisation. Human Papillomavirus and Related Cancers-Summary Report Update. (3rd Edn). 2010.
- Das BC, Gopalkrishna V, Hedau S, Katiyar S. Cancer of the uterine cervix and human papillomavirus infection. Curr Sci. 2000;78:52-63.
- Vinodhini K, Shanmughapriya S, Das BC, Seenivasan NK. Prevalence and risk factors of HPV infection among women from various provinces of the world. Arch Gynecol Obstet. 2012;285:771-777.
- Kailash U, Hedau S, Gopalkrishna V, Katiyar S, Das BC. A simple paper smear method for dry collection, transport and storage of cervical cytological specimens for rapid screening of HPV infection by PCR. J Med Microbiol. 2002;51: 606-610.
- Sotlar K, Diemer D, Dethleffs A, Hack Y, StubnerA. Detection and typing of human papillomavirus by E6 nested multiplex PCR. J Clin Microbiol. 2004;42:3176–3184.
- Baay MFD, Quint WFV, Koudstaal J, Hollema H, Duk JM, Burger MPM, et al. Comprehensive study of several general and type-specific primer pairs for detection of human papillomavirus DNA by PCR in paraffin-embedded cervical carcinomas. J Clin Microbiol. 1996;34:745–747.
- Woodman CB, Collins S, Winter H, Bailey A, Ellis J, Prior P, et al. Natural history of cervical human papillomavirus infection in young women: a longitudinal cohort study. Lancet. 2001;357:1831–1836.
- Franceschi S, Herrero R, Clifford GM, Snijders PJ, Arslan A, Anh PT, et al. Variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int J Cancer. 2006;119:2677–2684.
- Palefsky JM, Holly EA. Immunosuppression and co-infection with HIV. J Natl Cancer Inst Monographs. 2003;31:41-46.
- Plummer M, Schiffman M, Castle PE, Maucort-Boulch D, Wheeler CM. A 2-year prospective study of human papillomavirus persistence among women with a cytological diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion. J Infect Dis. 2007;195:1582–1589.
- Wang CJ, Palefsky JM. Human PapillomaVirus (HPV) Infections and the Importance of HPV Vaccination. Curr Epidemiol Rep. 2015;2:101-109.
- Chung CH, Bagheri A, D'Souza G. Epidemiology of oral human papillomavirus infection. Oral Oncol. 2014;50:364-369.
- Castellano T, Ding K, Moore KN, Landrum LM. Simple hysterectomy for cervical cancer: Risk factors for failed screening and deviation from screening guidelines. J Low Genit Tract Dis. 2019;23:124-128.
- RauhHJA, Clemmer JT, Bradford LS, Clark RM, Growdon WB, Goodman A, et al. Racial disparities in cervical cancer survival over time. Cancer. 2013;119: 3644-3652.
- Pergialiotis V, Bellos I, Thomakos N, Haidopoulos D, Perrea DN, Kontzoglou K, et al. Survival outcomes of patients with cervical cancer and accompanying hydronephrosis: A systematic review of the literature. Oncol Rev. 2019;13:381-387.
- Wadhwani M, Phuljhele S, Kumar R, Shameer A. Cervical carcinoma leading to orbital apex syndrome and blindness. BMJ Case Report. 2019;12.
- Schiffman M, Wentzensen N. Human papillomavirus infection and the multistage carcinogenesis of cervical cancer. Cancer Epidem Biomar Preven. 2013;22:553-560.
- Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941-1953.
- Dutta S, Begum R, Mazumder ID, Mandal SS, Mondal R, Biswas J, et al. Prevalence of human papillomavirus in women without cervical cancer: A population-based study in Eastern India. Int J Gynecol Pathol. 2012;31:178-183.
- Hildesheim A, Herrero R, Castle PE, Wacholder S, Bratti MC, Sherman ME, et al. HPV co-factors related to the development of cervical cancer: Results from a population-based study in Costa Rica. Br J Cancer 2001;84:1219-1226.
- Wallington SF, Luta G, Noone AM, Caicedo L, LopezCM, Sheppard V, et al. Assessing the awareness of and willingness to participate in cancer clinical trials among immigrant Latinos. J Commun Health. 2012;37: 335-343.
- Ndikom CM, Ofi BA. Awareness, perception and factors affecting utilization of cervical cancer screening services among women in Ibadan, Nigeria: A qualitative study. Reprod Health. 2012;9:11.
- Baileff A. Cervical screening: Patients’ negative attitudes and experiences. Nurs Stand. 2000;14: 35-37.
- Hussain SM. Cancer control in South Asia: Awareness is key to success. South Asian J Cancer. 2013; 2:55-56.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.