Identifying the Optimal Age to Perform Newborn Screening for Hearing Loss in Uganda
- *Corresponding Author:
- Miss. Maia Walsh,
Miss. Maia Walsh, Ian Hutcheon Clinic for Children, 3 Ambrose Lane, Harpenden, AL5 4AU, UK.
E-mail: maia.walsh@nhs.net
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Permanent congenital hearing loss affects up to 6/1000 births in developing countries. Currently, in Uganda there is no newborn screening for hearing loss (NSHL) program and no published work on this topic. Within the existing healthcare system there are two opportunities to deliver screening, at birth or 6 weeks of age when infants receive their immunizations. Aim: This study explored the outcomes of otoacoustic emission (OAE) testing in infants at birth and 6 weeks of age, to identify the optimal age for screening. Subjects and Methods: This cross‑sectional pilot study recruited 60 consecutive infants from two health centres in Kampala, Uganda. Thirty infants were newborns recruited from the postnatal ward and 30 were aged 4–8 weeks from the immunization clinic, we performed OAE testing on all infants. Results: The results showed 56.7% (17/30) of newborn infants passed OAE testing compared with 90.0% (27/30) of the immunization infants, P < 0.01. Furthermore, of the 11 newborn infants aged ≥24 h of age 90.9% (10/11) passed, compared with the 19 infants <24 h of age where 37% (7/19) passed, P < 0.01. Conclusions: This study demonstrates a higher pass rate for OAE testing for infants ≥24 h of age compared to those <24 h of age. The overall lower pass rate of the newborn infants could be due to external ear debris and middle ear fluid compromising the OAE testing. These findings would support a NSHL programme in Uganda that offers screening to infants ≥24 h of age, to maximize the cost‑effectiveness of the program.
Keywords
Hearing loss, Newborn, Screening
Introduction
Permanent congenital hearing loss (PCHL) is a major cause of disability worldwide affecting up to 6/1000 births.[1] This disease burden is highest in developing countries due to an increased prevalence of infectious disease and poor access to maternal healthcare. Furthermore, affected individuals are particularly vulnerable to social isolation and abuse due to the cultural beliefs about deafness and disability.[2] To date, there is no published work exploring newborn screening for hearing loss (NSHL) in Uganda.
NSHL faces many challenges to its successful implementation in developing countries. These include more limited access to audiological diagnostics and interventions, a high proportion of unattended home births and lower staffing levels. Therefore, it is important that NSHL protocols are appropriate for the resources and the healthcare infrastructure of each country. This concept is strongly encouraged by the World Health Organization, who advocate the implementation of NSHL program informed by local pilot projects.[3]
A key consideration for an NSHL program is when to screen the infants to ensure the best possible coverage. Uganda has a birth rate of 44/1000 population, one of the highest crude birth rates worldwide. Within Uganda most common place of birth shows significant geographical variability with 27.1% delivering in a health facility in Karamojo region compared with 92.9% in Kampala.[4,5] The first immunizations, bacillus Calmette–Guérin (BCG) and polio, are administered at birth prior to discharge from the health facility. The second set of immunizations are at 6 weeks of age and include diphtheria, pertussis and tetanus, hepatits B, haemophilus influenza B, and polio, with few infants receiving any clinical contact between the birth and this time point.[4] Infants born in the community receive their birth immunizations at the first point of contact, which is highly varied. The vaccination rate is more consistent across Uganda than the place of birth. In 2011, the rate for BCG vaccination in infants aged 12–23 months ranged from 85.2% in the Central region to 99.8% in Karamoja. Kampala’s BCG immunization rate at 12–23 months is reported as 94.6%, with 92.7% of infants receiving it by 8 weeks of age.[4,6]
Screening protocols have a significant impact on the cost-effectiveness of an NSHL program. Countries with an operational NSHL program include the UK, Germany, Canada, the United States, and Brazil and commonly use a combination of otoacoustic emission (OAE) and auditory brainstem response (ABR). OAE testing is a quick and low cost, but generates a higher numbers of false positives when compared with automated-ABR (A-ABR). Combining these two tests generates an effective screening protocol while limiting cost, however, for some developing countries the cost of A-ABR remains prohibitive.[7,8] Worldwide screening is largely performed in the newborn nursery with the first screening test performed from birth until approximately 10 days of age.[3] Newborn screening at a very young age has been shown to increase the false positive rate of OAE testing, especially in those <48 h of age.[9] These findings can be attributed to impaired conduction of the OAEs through the ear due to ear canal debris, middle ear fluid, and anatomical distortions of the external ear impacting ear probe fit.[9-12] Initiating screening in the immediate postnatal period facilitates a prompt diagnosis and timely intervention for affected infants. This allows NSHL programs to initiate appropriate interventions by 6 months of age, in keeping with the recommendations of the Joint Committee on Infant Hearing (JCIH).[13]
This study explores the outcomes of OAE testing in newborns and infants attending for their 6 weeks immunizations, at government health centres in Kampala, Uganda.
Subjects and Methods
This cross-sectional pilot study recruited 60 consecutive infants from two health centres in Kampala, Uganda. Thirty infants were newborn, aged 12 h–7 days and 30 were aged 4–8 weeks. The newborn group was recruited from the postnatal ward and the older infant group were attending the health center for their 6 weeks immunizations. The testing was performed using transient OAEs (TOAEs). Infants who failed the OAE testing were invited for two repeat OAE tests and then audiological diagnostics if required. Follow-up for any infant requiring further investigations or management was provided by the pediatric ear clinic at Kisugu health centre. The exclusion criteria for the groups were infants admitted to the neonatal unit and a birth weight <2.5 kg. Low birth weight was used as a proxy for prematurity as many mothers did not know their accurate gestation at birth. These babies were excluded due to the higher risk of auditory neuropathy that would not be detected using OAE testing.
The screening was performed using TOAEs with a Path Medical Solutions Sentiero device. For infants to pass the OAE test, they required a minimum signal to noise ratio of 6 dB in 3 bands out of 1, 1.5, 2, 3 or 4 kHz in both ears.
The screening was performed by two medically qualified personnel from the UK. The staff received 2 days of training prior to commencing the study. Two local members of staff at each location were recruited to assist with translation for consenting and discussing results with parents when required. In addition to a verbal discussion, all families were given an information leaflet in either English or Luganda with education about normal developmental milestones for hearing and speech and contact details for the pediatric ear clinic at Kisugu health centre.
The screening was performed over a 1-month period, in Kisenyi and Kisugu health centres in Kampala. At both health centers, the quietest available space was found to perform the screening assessment. Repeat screening was performed in the same location as the original testing, however, audiological diagnostics were provided in a private clinic with follow-up at the Pediatric Ear Clinic at Kisugu Health Centre. For families attending the follow-up and requiring further audiological diagnostics travel expenses and the cost of the diagnostics were provided. Families who failed to attend for repeat testing were contacted by telephone on one occasion to schedule a new appointment for repeat testing. The study complied with the ethical requirements of the declaration of Helsinki. Data were analyzed using SPSS Statistics for Windows, Version 17.0. Chicago, IL, USA: SPSS Inc. Fisher's exact test was used to test for statistcial significance when comparing pass rates between the newborn and immunisation groups and to compare the pass rates between the newborn infants aged <24 hrs and ≥24 hrs.
Results
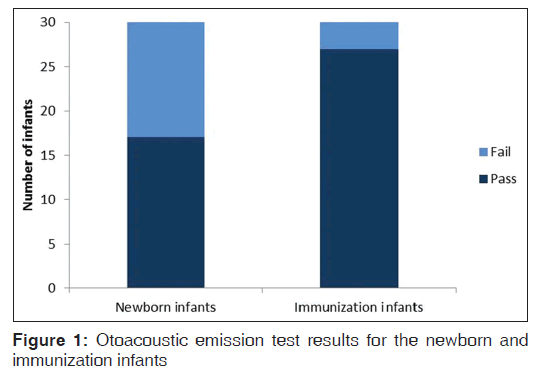
Sixty infants were enrolled in this study, of which 30 were newborn and 30 were from the immunization clinic. The newborns were aged between 12 and 149 h, median 21 h (interquartile range 17-29 h). The immunization group was aged between 28 and 56 days, median 43 days (interquartile range 42-45 days). The median birth weight of the newborns was 3.2 kg (interquartile range 2.9-3.6 kg) and for the immunization infants it was 3.4 kg (interquartile range 2.8-3.5 kg). 56.7% (17/30) (confidence interval 95% [CI] 39.2–72.6%) of the newborn infants passed the screening and 90.0% (27/30) (95% CI 73.6–97.3%) of the immunization infants passed the screening, as shown in Figure 1, all CIs are at the 95% level. Following analysis using Fisher’s exact test this result was shown to be statistically significant at the 5% level (P < 0.01).
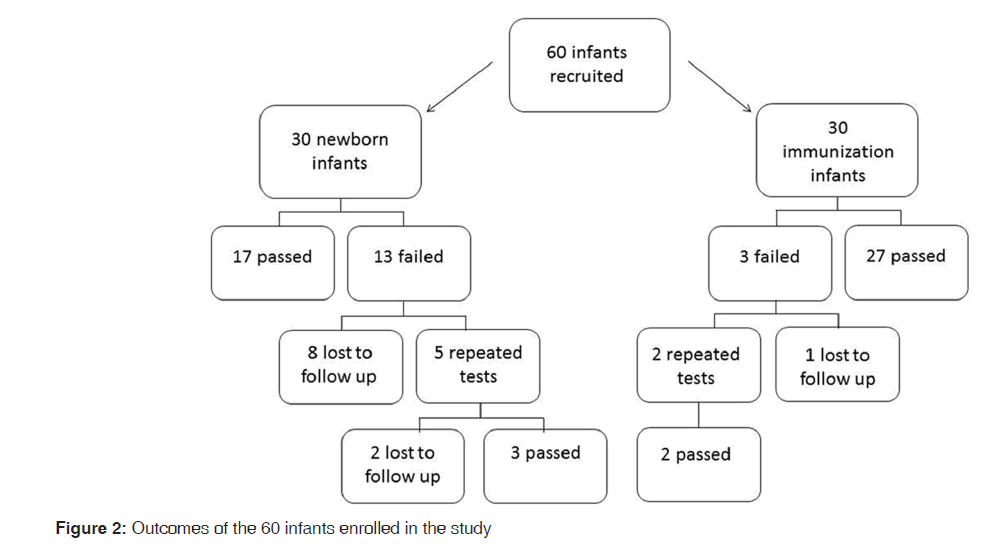
Of the 13 newborn infants who failed the first OAE test, 10 were lost to follow-up during the re-testing process and three passed at re-test. At the first repeat test, the attendance rate was 38.5% (5/13) and at the second repeat test, the attendance rate was 33.3% (1/3). Of the 10 newborn infants lost to follow-up, 1 was aged ≥24 h and 9 were <24 h of age. From the immunization group only the first repeat test was required with an attendance rate of 66.7% (2/3,) shown in Figure 2.
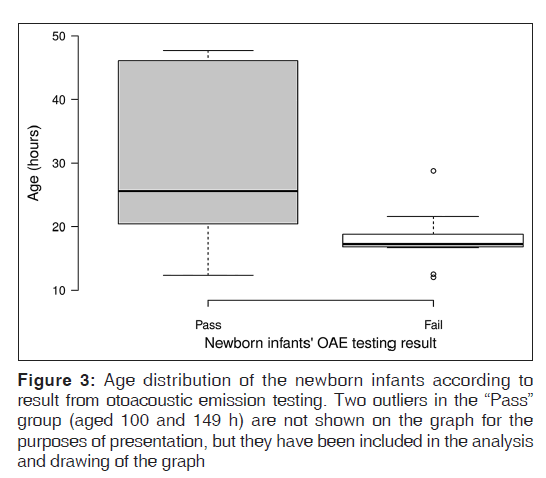
Within the newborn group, there was a difference in the age distributions of the infants who passed and failed the screening test as shown in Figure 3. The median age of infants who passed was 25.6 h compared to 17.3 h for the infants who failed. Furthermore, of the 11 newborn infants aged ≥24 h of age 90.9% (10/11) (95% CI 60.1–99.9%) passed, compared with the 19 infants <24 h of age where 36.8% (7/19) (95% CI 19.1–56.1%) passed. Analysis with Fisher’s exact test shows these results are statistically significant at the 5% level (P < 0.01).
The mean duration of test time for each ear that passed the test was 35 s for the newborn infants and 25 s for the immunization infants. However, this difference did not reach statistical significance.
Discussion
The findings of this study reveal a statistically significant higher pass rate in the immunization infant group and newborns aged ≥24 h of age compared with the newborns aged <24 h. This finding correlates with other studies and could be the result of external ear debris and middle ear fluid, which is thought to resolve in the 1st days of life.[9-12] The suggestion that 24 h of age could be a threshold point where the pass rate for OAE testing significantly improves could be used to inform an NSHL protocol. This would ensure the best use of limited resources - an important factor for health services in Uganda. However, the small sample size of infants ≥24 h of age limits the strength of this conclusion and more research in this population is required to corroborate this finding.
The published pass rate, following a single OAE test, varies widely ranging from 59% to 90%. An average pass rate of 75% can be calculated using data from the meta-analysis conducted by Akinpelu et al. as well as other recent publications.[9,14-17] While our newborn pass rate of 56.7% reflects a lower than average pass rate, there are numerous factors that explain this. First, 63.3% of the newborn infants screened in this study were <24 h old, which is shown to be associated with a lower pass rate.[9-11,18,19] Our test environments had a high ambient noise level averaging 65–70 dB, which is also shown to negatively impact pass rates.[20,21] Finally, our pass criteria were more stringent than some of those used in the studies listed above which may also have contributed to a lower pass rate. Although the latter two factors were the same for both the newborn and immunization group, it may be that the combination of all three effects creates such a challenging environment for OAE testing that we see a threshold effect with a sudden decrease in pass rates.
The attendance rate for re-testing in this study was 66.7% for the immunization infants and 38.5% and 33.3% for the first and second re-test, respectively, for the newborn infants. Although the difference in attendence rate appears large between the two groups, the result is not statistically signigicant as the number of infants involved was very small. A low attendance rate for re-testing is a recognized problem of NSHL programs in developing coutries with programs in South Africa and Nigeria reporting the re-test attendance rates of between 40% and 48% per screening stage.[22,23] We encountered significant difficulties contacting the families by telephone to rearrange the repeat testing and found an appointment based service had limited success. A more frequent walk in service is likely to be more effective, as it offers families more flexibility and is more in keeping with how other health services in Uganda are organized. Improving the attendance rate for re-testing is crucial to being able to provide an effective NSHL service and the findings here suggest limiting the number of repeat tests would help address this issue.
Gaining the widest level of coverage is another key factor in a successful NSHL program and is heavily influenced by the platform from which screening is delivered. Within Kampala up to 92.7% of infants are delivered in a healthcare facility and the same number receives their BCG immunization by 8 weeks of age.[4,6] This suggests that NSHL in Kampala could be delivered from either a health care facility or an immunization clinic with similar levels of coverage. However, in Karamoja region only 27% of infants are delivered in a health care facility whereas 99.8% receive their BCG vaccination by 12–23 months of age. Although data is not available to indicate at specifically what age infants in Karamoja receive their BCG vaccination, the number who deliver in a health facility is so low that it would not be a viable platform for NSHL in this region.[4] A NSHL service would need to consider regional differences when deciding on the best platform to deliver a program and whether a service should be delivered from both to maximize coverage.
The disadvantage of screening infants at 4–8 weeks of age is the difficulty of organizing all the required testing and initiating interventions by 6 months of age, as recommended by the JCIH. However, at present there is no state funded hearing amplification service in Uganda and it is unlikely that this will change in the near future. For the average Ugandan these services are only accesible through partnerships with Nongovermental Organizations, the local healthcare system and private audiology services. It will require the further development of such partnerships to verify how long it would take an infant to navigate all the diagnostics and reach the point of initiating an intervention. Concerns that older infants may be more problematic to the screen as they are more active and the alert was not our experience. This is shown in the average 10 s shorter testing time per ear for the immunization infants. Furthermore, we feel this group of infants are easier to screen as the mothers are more mobile than those on the postnatal ward. This allows for a wider choice of testing venues which could be particularly helpful in minimizing the high background noise levels.
Amplification is not the only means of providing a life-changing intervention. Better access to speech and language therapy, education for families, and suitable schooling environments can have a hugely beneficial effect on an individual with PCHL. In Uganda the stigma attached to deafness and disability prevents many families from accessing help when it becomes evident that a child is not developing appropriately. To diagnose children in early infancy provides unique access to these families and the opportunity to educate families about deafness and disability. However, no research has been done to explore the impact of an early diagnosis of PCHL in Uganda. While we hope an earlier diagnosis would lead to a better outcome for the child and family, it could negatively affect the early relationship between a mother and baby and result in rejection of the baby. Further research needs to be conducted to explore the impact of an early diagnosis of PCHL in a setting where access to audiological services for confirmation of the diagnosis and amplification servies is limited.
Conclusions
This study demonstrates a higher pass rate for OAE testing for infants ≥24 h of age compared to those <24 h of age. We suggest that 24 h of age could be the threshold where the pass rate for OAE testing significantly improves, however, further research needs to be done to corroborate this finding in this population group. These findings would support an NSHL program in Uganda that offers screening to infants ≥24 h of age. The screening platform needs to consider regional healthcare behaviors regarding the place of delivery and attendance at immunization clinic, to capture the highest number of infants and deliver the most cost-effective service. In addition, the pathway for audiological diagnostics and interventions needs to be clarified to see whether testing at 4–8 weeks could be compatible with achieving interventions by 6 months of age.
Acknowledgements
This study was funded by the Ian Hutcheon Clinic for Children and the Ugandan Maternal and Newborn HUB.
Huge thanks to Dr. Paul and Liz Choudhury from the Ian Hutcheon Clinic for Children for the guidance, support and enthusiasm. Furthermore, thanks to Apollo Muhangi and all the staff at Kisenyi and Kisugu health centre for their support and help.
Financial support and sponsorship
Funding and equiment for this study has been provided by the Ian Hutcheon Clinic for Children, Charity No. 1145080.
Conflicts of interest
There are no conflicts of interest.
References
- World Health Organization. WHO Workgroup for Development of Version of ICF for Children and Youth. International Classification of Functioning, Disability and Health Children and Youth Version (ICF-CY). Geneva: WHO; 2007. Available from: http://www.apps.who.int/ iris/bitstream/10665/43737/1/9789241547321_eng.pdf. [Last accessed on 2014 Oct 04].
- Kiyaga NB, Moores DF. Deafness in sub-Saharan Africa. Am Ann Deaf 2003;148:18-24.
- World Health Organization. Newborn and infant hearing screening. Current issues and guiding principles for action. Outcome of a WHO informal consultation held at WHO head-quarters, Geneva, Switzerland, 9-10 November, 2009. Geneva: WHO; 2010.
- Uganda Bureau of Statistics (UBOS), ICF International Inc. Uganda Demographic and Health Survey 2011. Kampala, Uganda, Calverton, Maryland: UBOS, ICF International Inc.; 2012.
- The Wor ld Bank Group. Wor ld Deve lopment Indicators – Crude Birth Rate. The World Bank’s Open Data Catalog; 2012. Available from: http://www.data.worldbank. org/indicator/SP.DYN.CBRT.IN?order=wbapi_data_ value_2012+wbapi_data_value+wbapi_data_value-last and sort=asc. [Last accessed on 2015 Jan 17].
- Babirye JN, Engebretsen IM, Makumbi F, Fadnes LT, Wamani H, Tylleskar T, et al. Timeliness of childhood vaccinations in Kampala Uganda: A community-based cross-sectional study. PLoS One 2012;7:e35432.
- Lin H, Shu M, Lee K, Lin H, Lin G. Reducing false positives in newborn hearing screening program: How and why comparison of referral rates after discharge. Otol Neurotol 2007;28:788-92.
- Cavalcanti HG, Melo LP, Buarque LF, Guerra RO. Overview of newborn hearing screening programs in Brazilian maternity hospitals. Braz J Otorhinolaryngol 2014;80:346-53.
- Akinpelu OV, Peleva E, Funnell WR, Daniel SJ. Otoacoustic emissions in newborn hearing screening: A systematic review of the effects of different protocols on test outcomes. Int J Pediatr Otorhinolaryngol 2014;78:711-7.
- Torrico P, Gómez C, López-Ríos J, de Cáceres MC, Trinidad G, Serrano M. Age influence in otoacoustic emissions for hearing loss screening in infants. Acta Otorrinolaringol Esp 2004;55:153-9.
- Korres S, Nikolopoulos T, Ferekidis E, Gotzamanoglou Z, Georgiou A, Balatsouras DG. Otoacoustic emissions in universal hearing screening: Which day after birth should we examine the newborns? ORL J Otorhinolaryngol Relat Spec 2003;65:199-201.
- Maxon AB, White KR, Culpepper B, Vohr BR. Maintaining acceptably low referral rates in TEOAE-based newborn hearing screening programs. J Commun Disord 1997;30:457-75.
- Joint Committee on Infant Hearing, American Academy of Audiology, American Academy of Pediatrics, American Speech-Language-Hearing Association, Directors of Speech and Hearing Programs in State Health and Welfare Agencies. Year 2000 position statement: Principles and guidelines for early hearing detection and intervention programs. Joint Committee on Infant Hearing, American Academy of Audiology, American Academy of Pediatrics, American Speech-Language-Hearing Association, Directors of Speech and Hearing Programs in State Health and Welfare Agencies. Pediatrics 2000;106:798-817.
- Olusanya BO, Ruben RJ, Parving A. Reducing the burden of communication disorders in the developing world: An opportunity for the millennium development project. JAMA 2006;296:441-4.
- Firoozbakht M, Mahmoudian S, Alaeddini F, Esmaeilzadeh M, Rafiei M, Firouzbakht A, et al. Community-based newborn hearing screening programme for early detection of permanent hearing loss in Iran: An eight-year cross-sectional study from 2005 to 2012. J Med Screen 2014;21:10-7.
- Haghshenas M, Zadeh P, Javadian Y, Fard H, Delavari K, Panjaki H, et al. Auditory screening in infants for early detection of permanent hearing loss in northern Iran. Ann Med Health Sci Res 2014;4:340-4.
- Qi B, Cheng X, En H, Liu B, Peng S, Zhen Y, et al. Assessment of the feasibility and coverage of a modified universal hearing screening protocol for use with newborn babies of migrant workers in Beijing. BMC Pediatr 2013;13:116.
- Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of children with mild-profound congenital hearing loss at 7 to 8 years: A population study. Ear Hear 2004;25:1-8.
- Prieve BA, Hancur-Bucci CA, Preston JL. Changes in transient-evoked otoacoustic emissions in the first month of life. Ear Hear 2009;30:330-9.
- Jacobson JT, Jacobson CA. The effects of noise in transient EOAE newborn hearing screening. Int J Pediatr Otorhinolaryngol 1994;29:235-48.
- Headley GM, Campbell DE, Gravel JS. Effect of neonatal test environment on recording transient-evoked otoacoustic emissions. Pediatrics 2000;105:1279-85.
- Olusanya BO, Ebuehi OM, Somefun AO. Universal infant hearing screening programme in a community with predominant non-hospital births: A three-year experience. J Epidemiol Community Health 2009;63:481-7.
- Swanepoel de W, Hugo R, Louw B. Infant hearing screening at immunization clinics in South Africa. Int J Pediatr Otorhinolaryngol 2006;70:1241-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.