Idiopathic Ileo-ileal Intussusceptions: A Case Report and Brief Review of the Literature
2 House officer, Civil Hospital Karachi, Karachi, Pakistan, Email: mohammaduddin2020@gmail.com
3 Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
4 Pediatric Medicine, National Institute of Child Health, Karachi, Pakistan
Citation: Yaqoob U, et al. Idiopathic Ileo-ileal Intussusceptions: A Case Report and Brief Review of the Literature. Ann Med Health Sci Res. 2018;8:18-20
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A disease influencing babies and little children is the definition of intussusception. It as a rule happens at the age of 5-9 months. Small bowel intussusceptions are extremely uncommon however here we report an instance of a 6-day old baby, with idiopathic ileoileal intussusception, conveyed to the emergency department with 1 day history of fever and fits. She was in respiratory distress on presentation. Urea and creatinine was notably raised. Primary diagnosis of acute kidney damage with sepsis was made and differentials of febrile seizures, CNS meningitis and epilepsy were considered. Bleeding per rectum and greenish vomiting (and aspirate after passing nasogastric tube) began on the second post admission day. We thought of intestinal atresia (ruled out on X-rays) or intussusception. Ultrasound recommended intussusception with no lead point (potentially ileo-ileal). Barium study additionally indicated ileo-ileal intussusception. After barium examination patient passed normal stools and her nasogastric tube demonstrated no extra aspirate. Nasogastric tube was evacuated after oral encouraging trial. Moreover, her laboratory values also improved. We did another ultrasound, which demonstrated no proof of intussusception. Oral intake was started and the patient was discharged. Our case features the fact that finding of intussusception in newborn children is extremely testing because of the variable clinical presentation and an expansive scope of differentials. Consequently, small bowel intussusceptions can easily be overlooked clinically. Furthermore, it also tells us the importance of conducting prompt investigations such as barium meals and ultrasound on toddlers presenting with nonspecific symptoms of small bowel intussusception.
Keywords
Intussusception; Nasogastric tube; Ultrasound
Introduction
Intussusception is a disease affecting infants and toddlers, with a peak incidence between 5-9 months. Studies have reported that only 10-20% of the cases occur after 2 years of age, whereas the incidence of cases in school-aged children is known to be 1-6%. [1] Small bowel intussusceptions are very rare, with 90% of the cases in pediatric age accounting for ileocolic, ileocecal or ileo-ileo-colic intussusceptions. [1] The basis of diagnosis of intussusception can be cleaved into major and minor criteria. Major criteria includes evidence of intestinal obstruction (with signs of bilious vomiting, with a tender distended abdomen and a plain radiograph showing gas-filled distended loops of as well as air-fluid levels), features of intestinal invagination (with palpation of a soft tissue mass on abdominal or rectal examination or visualized on abdominal radiograph, ultrasound or CT.), and intestinal vascular compromise or venous congestion (with rectal bleeding that can appear dark red, mixed with mucoid thereby giving it a current jelly-like appearance). Furthermore, minor criteria include age less than 1-year-old and male gender, vomiting, lethargy, abdominal pain, pallor and shock. [2] Here we report a case of a 6-day old girl, with idiopathic ileo-ileal intussusception.
Case Report
A 6-day old girl came in the emergency department with the complaint of fever and fits since one day. As far as the antenatal, natal and postnatal history was concerned, there was nothing significant. On examination, the child was in distress but rest of the examination was unremarkable. The patient was kept NPO (nil per oral) and on oxygen using nasal prongs. Furthermore, antibiotic coverage Cebac (Sulbactam and Cefoperazone) 120 mg (twice a day), Linezolid 30 mg (twice a day) was started and for the seizures IV phenytoin, 5 mg (twice a day was started. The Patient was catheterized and urine output was monitored. At this point in time, we assumed differentials such as febrile seizures, CNS meningitis or epilepsy. We did an emergency ultrasound of the brain which was normal.
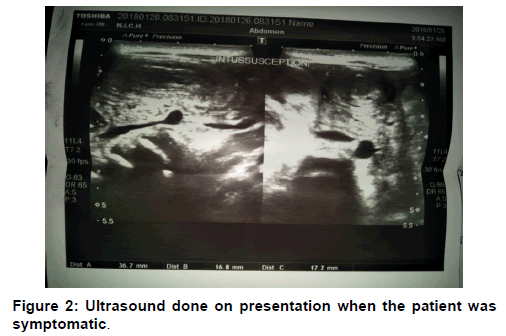
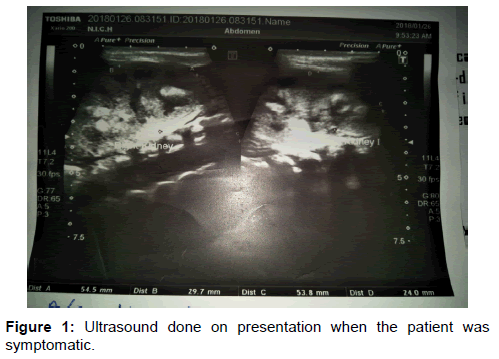
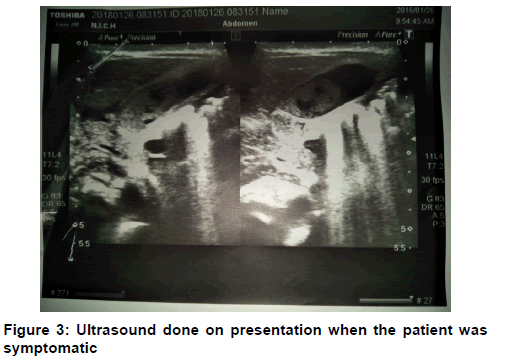
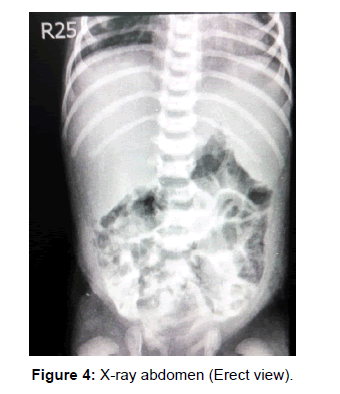
At the time of admission, Patient’s laboratory values came out to be hemoglobin 21.9 gm/dl, total leukocyte count 21.8 × 10^9/l (with 52% neutrophils), platelet 137000, urea 268 mg/l, creatinine 3.2 mg/l, sodium 165 meq/l, potassium 6.9 meq/l and chloride 124 meq/l. Based on these laboratory values we made a diagnosis of acute kidney injury with sepsis. However, since the second day of admission, the patient’s mother started complaining of bleeding per-rectal and no stools were being passed since then. There has also been green colored vomiting from the same day. A nasogastric tube was passed and it contained a greenish aspirate, which appeared to be bilious in nature. At this point in time, we thought of intestinal atresia (at the level of duodenum or jejunum) or intussusception. Immediately and X-Ray abdomen (erect and supine view) were advised after surgical review. Both X-Rays were unremarkable and small bowel atresia was ruled out. Ultrasound showed a hypo-echoic area with central crescent-in-doughnut target sign measuring 1.6 × 1.7 cm, seen at the right lower abdomen suggesting intussusception without any lead point (possibly ileo-ileal). After about a week of admission the patient was no longer in distress, we took the neonate for barium meal and follow through, which showed a normal duodenum and pyloric canal, very slow passage of barium in jejunal loops. Jejunal loops appear dilated with thickened walls and segmentation. Up to 7 hours film barium is showed in proximal ileal loops. Furthermore, 48 hours film showed all of the contrast in the jejunum. No contrast was seen in ileum and another ultrasound at that point showed ileo-ileal intussusception. Preparation for surgery was done [Figures 1-4].
After barium investigation patient passed normal stools and her nasogastric tube showed no additional aspirate. The tube was clamped and oral feeding trial was given. Since there was no vomiting nasogastric tube was removed. Furthermore, her laboratory values also improved with urea 64 mg/dl, creatinine 0.5 mg/l, sodium 152 meq/l, potassium 3.7 meq/l. Since intussusception can spontaneously resolve on its own, we did another ultrasound, which showed marked improvement as compared to the previous scan and there was no evidence of intussusception. Oral intake was started and the patient was discharged [Tables 1 and 2].
| Variables | 24/1/2018 | 23/1/2018 | 26/1/2018 | 28/1/2018 | 25/2/2018 | 1/2/2018 |
|---|---|---|---|---|---|---|
| Urea | 260 | 268 | 296 | 240 | 269 | 64 |
| Cr | 2.4 | 3.2 | 2.3 | 1.3 | 2.3 | 0.5 |
| NA | 155 | 165 | 147 | 159 | 151 | 152 |
| K | 4.5 | 6.9 | 4.7 | 4.3 | 4.4 | 3.7 |
| CL | 115 | 124 | 108 | 119 | 109 | 111 |
Table 1: Serum urea creatinine and electrolytes.
| Variables | 23/1/2018 | 25/2/2018 |
|---|---|---|
| HB | 21.9 | 22.0 |
| TLC | 21800 | 24800 |
| N | 52 | 80 |
| L | 40 | 16 |
| PLT | 137000 | 30000 |
Table 2: Complete blood profile.
Discussion
Intussusception is defined as the invagination of a segment of the bowel into a segment of the adjoined intestinal lumen. [3] The incidence of intussusceptions is approximately 50 per 100,000 individuals. This incidence is lower among children younger than 3 years or older than 6 years. [4] Ileo-colic intussusception is one of the most common causes of an acute abdomen in children and also has a classic clinical picture of vomiting, currant jelly stools, and severe colicky abdominal pain. [5] Small bowel intussusceptions are unusual, accounting for 1-10% of all intussusceptions but up to 50% of all cases in older children. Literature has described ileo-ileal, jejuno-jejunal, jejuno-ileal and duodeno-jejunal intussusception in the descending order of frequency. Furthermore, the presentation of small bowel intussusception is also variable, as the classic features of palpable abdominal mass and bloody stools are rarely present, making it difficult to diagnose, leading to increased risk of ischemic complications. [1,5] Our case also showed a difficulty in diagnosis, as no abdominal mass was palpable and bloody stools were only found after the second day of admission.
Literature states that >29% small bowel intussusceptions are associated with pathological lead points. Furthermore, studies also show that after 2 years of age, pathological lead points are found in one-third of the patient, and toddlers and children are more likely to have idiopathic intussusception. Commonly mentioned pathological entities include polyps, Meckel’s diverticulum, intestinal duplication and lymphomas. [1,6] Our case further adds up to the literature as it also reported an infant with idiopathic intussusception and without any lead point. There are several factors that lead to idiopathic intussusception; the presence of swelling in the small bowel, abnormal gastrointestinal motility, and scars or adhesions from previous insults. [1] After reviewing the literature, we found numerous cases with similarities to ours that resolved without any intervention. [3,7] Furthermore, authors have stated if the ultrasound shows benign small bowel intussusception, and child is asymptomatic, the patient can be managed conservatively and should be monitored by subsequent imaging at 45 minutes interval to confirm the reduction. In addition, if the reductions do not occur and child is asymptomatic, it is appropriate to follow up these patients without doing any repeat ultrasounds. However, if the patient has persistent symptoms, with either recurrent or multiple intussusceptions, then they should undergo surgical exploration. [7]
Barium enema and ultrasound has been used widely for definitive diagnosis of intussusception (an added advantage of reduction by enema is there) but in our case, the game-changing investigation turned out to be barium meal and follow through, although our basic aim was to rule out duodenal/jejunal atresia. [8]
A 2-3 cm doughnut-like lesion in the left abdomen or paraumbilical region with ultrasound is highly suspicious for small bowel intussusception. Furthermore, an intussusception length >3.5 cm has been reported as a sensitive and specific predictor that requires surgical intervention as compared to those that resolved spontaneously. [5] Our patient had a doughnut-like lesion roughly measuring 2.72 cm (1.6 × 1.4), but the intussusception length was not assessed.
Conclusion
Our case highlights the fact that diagnosis of intussusception in infants is very challenging because of the variable clinical presentation and a broad range of differentials. Hence, small bowel intussusceptions can easily be overlooked clinically. Furthermore, it also tells us the importance of conducting prompt investigations such as barium meals and ultrasound on toddlers presenting with nonspecific symptoms of small bowel intussusception.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- El-Gasim SHB, Benziger H. Idiopathic ileo-ileal intussusception in older children: A case report and brief literature review. The Internet Journal of Pediatrics and Neonatology. 2009;12.
- Bines JE, Ivanoff B, Justice F, Mulholland K. Clinical case definition for the diagnosis of acute intussusception. Journal of pediatric gastroenterology and nutrition. 2004;39:511-518.
- Nelson MJ, Paterson T, Raio C. Case report: A transient small bowel intussusception presenting as right lower quadrant pain in a 6-year-old male. Critical Ultrasound Journal. 2014;6:7.
- Asaumi Y, Miyanaga T, Ishiyama Y, Hattori M, Hashizume Y. Pediatric ileoileal intussusception with a lipoma lead point: a case report. Gastroenterology report. 2013 Dec 19;2:70-72.
- Smyth R, McCallion WA, Paterson A. Total jejunoileal intussusception: A case report and literature review. The Ulster Medical Journal. 2009;78:10.
- Stringer MD, Pablot SM, Brereton RJ. Paediatric intussusception. British Journal of Surgery. 1992;79:867-876.
- Parikh M, Samujh R, Kanojia R, Sodhi KS. Does all small bowel intussusception need exploration?. African Journal of Paediatric Surgery. 2010;7:30.
- Del-Pozo G, Albillos JC, Tejedor D, Calero R, Rasero M, De-la-Calle U, et al. Intussusception in children: Current concepts in diagnosis and enema reduction. Radiographics. 1999;19:299-319.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.