Informed Consent Practices and its Implication for Emergency Obstetrics Care in Azare, North-Eastern Nigeria
- *Corresponding Author:
- Dr B. Bako
Department of Obstetrics and Gynecology University of Maiduguri Teaching Hospital P.M.B 1414 Maiduguri, Borno State, Nigeria
Tel: +2348025997255
E-mail: babaganabako@yahoo.com
Date of Received : 02-03-11
Date of Accepted : 21-08-11
Date of Published : 22-12-11
Abstract
Background: Consent practices can affect the institution of emergency obstetrics care in the health facility, and may indeed, determine the degree of maternal mortality and morbidity.
Objectives: This study was aimed at determining informed consent practices and its implication for Emergency Obstetrics Care (EOC).
Methods: A cross-sectional study involving 787 women who presented with obstetric emergencies at the FMC Azare from 1st January 2008 to 31st December 2009 was done. The sociodemographic characteristics and birth outcome were compared between those that gave early consent (EC) and those that gave delayed consent (DC). Data was analysed using SPSS version 11. Morbidities and mortalities were compared in the two groups and P < 0.05 was considered statistically significant.
Results: EC for obstetric intervention was obtained in 260 (33.0%) of the cases, while 527 (66.0%) gave DC. The mean length of time for DC was 4.5 + 3.5 hours (Range 1.25 to 72 hours). In 62.9% of cases the consent was given by the husband while the patient consented in 5.6%. In-laws, relatives and others were responsible for 13.8%, 8.5%, 5.7% and 3.5% respectively. Consent was significantly delayed when given by the husbands, in-laws and relatives. Patients that gave consents for their own treatment were more likely to be gainfully employed (P=0.019), educated (P=0.004) and booked (P=0.001). Maternal mortality, intrauterine fetal death, low Apgar scores and early neonatal death were significantly increased in the DC group with P values of 0.016, 0.032 and 0.026 respectively.
Conclusion: Delay in giving Consent contributes significantly to maternal and fetal morbidity and mortality in our environment because it increases the 3rd level of delay.
Keywords
Informed Consent, Early consent, Delayed consent, Emergency obstetric care, Obstetric intervention, Azare.
Introduction
Informed consent forms the basis of the fiducial relationship between the patient and the physician and it is essential to the physician's ability to diagnose and treat patients as well as the patient's right to accept or reject clinical evaluation, treatment, or both.[1] It is a mandatory process needed in the course of treatment of all patients and its main value is that it satisfies the ethical requirements of the autonomy of the treated individual.[2] The concept originated from the legal and ethical right of the patient to direct what happens to his/her body and from the ethical duty of the physician to involve the patient in healthcare decisions.[3]
Informed consent may be defined as 'the legal term describing a patient's voluntary agreement to a doctor performing an operation, arranging drug treatment, or carrying out diagnostic tests.[4] For medical intervention, informed consent is widely accepted as a voluntary, uncoerced decision made by a sufficiently competent, autonomous person on the basis of adequate information and deliberation to accept rather than to reject some proposed course of action that will affect him or her.[5] Informed consent therefore implies that a discussion has taken place about basic elements including the nature of the decision/procedure; reasonable alternatives to the proposed intervention; the relevant risks, benefits and uncertainties related to each alternative; an assessment of patient’s understanding and the acceptance of the intervention by the patient.[6]
To obtain an informed consent, the physician should take time and use simple language to facilitate patient’s comprehension of a treatment or procedure. Adequate time should be allowed for the patient to understand the information and truly make an informed choice.[7] In some African societies, consent for intervention may not be obtainable immediately the patient arrives the hospital mainly because of the paternal nature of our societies, where women play a subordinate role to the man.[8] The communal traditions ensure that the designated head of a family unit has the honour and sole responsibility of assenting and consenting to an operation or invasive procedures to be carried out on a younger, or female, member of the family.[9] The consent practices are also influenced by the level of education, extended family system, urbanisation, religious practices and health care financing options available.[10] Therefore, the consent can be given by the patient or her legal guardian.
Delays along the ‘path’ to receiving adequate care are prominent factors contributing to maternal deaths in developing countries.[11] While it is known that delays could occur at various levels,[11] delay at the health facility may not be due to faults in the health care delivery system alone but could sometimes be attributed to delay in giving informed consent. Complications and deaths resulting from delays in giving consent in time contribute to the bulk of discussion in our departmental clinical audit meetings. This study was aimed at documenting informed consent practices and consequences of delay in giving consent for obstetrics intervention at the hospital. This information can be used for advocacy to the community and policy makers.
Subjects and Methods
This was a cross-sectional study conducted at the department of Obstetrics and Gynecology of the Federal Medical Centre (FMC) Azare from 1st January 2008 to 31st December 2009. The FMC is a 300 bed capacity tertiary health facility located in the sub-urban town of Azare in Bauchi State, North-eastern Nigeria. It serves the people of Bauchi state and the neighbouring states of Jigawa and Yobe.
The subjects were pregnant women who presented to the department with any of the four major obstetric causes of maternal mortality. [12] These emergencies were obstetric hemorrhage, severe Pregnancy Induced Hypertension (PIH) and eclampsia, obstructed labour and severe anemia in pregnancy. Those that developed fetal distress while in labour were also included. Other emergencies such as abortions, retained placenta, cord prolapse e.t.c. were excluded because they were less frequent causes of maternal death in our environment and informed consent could be gotten promptly in these cases. Patients were recruited consecutively as they presented and the emergencies were managed according to the departmental protocols. However, for any invasive procedure or surgery the patient and/or her legal guardian were counselled and informed consent sought. Counselling was done using simple language so that the patient or her legal guardian could understand the discussion. Local languages such as Hausa and Fulfulde were employed to ascertain full comprehension of the discussion before informed consent was sought. For the purpose of this study, we categorized the patients into 2 groups depending on the time lapsed from the end of the discussion and informed consent given. Early consents (EC) were those that gave consent within an hour while delayed consents (DC) were those that delayed giving informed consent for more than one hour. Counselling was done by the registrar or senior registrar on duty. The consultant was also involved in those cases where consent was delayed or declined. He usually confirms that the patient or her legal guardian really understood their condition and the consequences of their actions. Record was made of the person who gave the consent and for the DC; the delay period was recorded in hours. Informed consent was written in Cesarean Section (C/S), destructive operation and instrumental vaginal delivery while verbal consent was gotten for blood transfusion and Induction of Labour (IOL). Only the first invasive treatment that required consent was used in this study.
Interventions studied were blood transfusion, emergency cesarean section, instrumental vaginal delivery, induction of labour (IOL) and destructive operation. IOL was done on emergency basis for patients with eclampsia that were stabilized with magnesium sulphate.
Other information such as the sociodemographic characteristics of the patient, fetal viability, birth weight, Apgar scores, neonatal unit admission and neonatal death were also obtained.
The nature of the interventions and complications were compared in the two groups. The dexterity to give consent was also compared among the individuals that gave consent. Only patients that consented to take part in the study were recruited while those that did not consent for the obstetrics intervention or did not give consent for the study were excluded.
Severe anemia was PCV < 18% [13] and sepsis, included wound infection and puerperal sepsis. Low Apgar score refers to 5th minutes Apgar score of <7 [14] and early neonatal death were neonatal death within 7 days of delivery. [15]
All the information obtained were coded and transferred on to a proforma already designed for the study. It was then entered into an international business machine (IBM) compatible personal computer (PC) for analysis using SPSS version 11.0 for window statistical package. Chi square was computed for categorical variable at 95% confidence interval. P value of less than 0.05 was considered significant. The hospital ethical committee reviewed and approved all aspects of the study.
Results
During the study period, 942 women that presented with obstetric emergencies met the inclusion criteria and were selected for the study. One hundred and fifty five patients were excluded from the study; 9 patients declined consent, 7 patients declined treatment and 139 patients were excluded because of incomplete information. Seven hundred and eighty seven 787 (84.9%) patients were analysed. The mean age of the patients was 22.5+10.5 years and 549 (58.3%) were young women below the age of 25 years. Nulliparous women constituted 221 (28.1%) and 570 (72.4%) of them were unbooked. About fifty two percent (409) had no formal education and 640 (81.3%) were unemployed housewives.
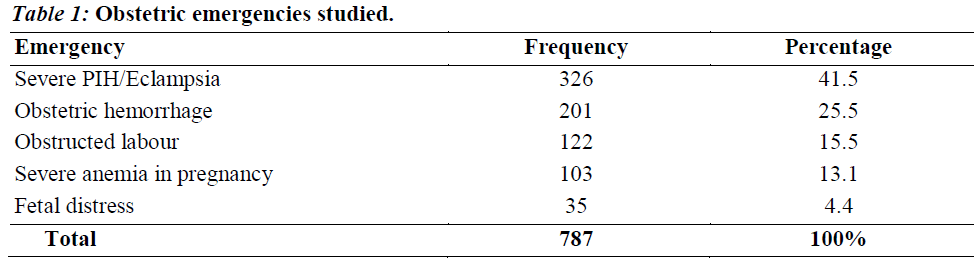
The common obstetric emergencies seen were hypertensive disorders of pregnancy (severe pregnancy induced hypertension and eclampsia) and obstetrics hemorrhage which constituted 326 (41.5%) and 201 (25.5%) respectively as shown in table 1. Thirty five (4.4%) women developed fetal distress while in labour.
Blood transfusion and emergency cesarean section were the commonest obstetric interventions offered to 336 (42.7%) and 244(31.0%) of the patients respectively, while destructive operation was needed in 28 (3.5%) of the cases. Instrumental vaginal delivery and IOL were offered to 113 (14.4%) and 66 (8.4%) of the patients.
EC for obstetric intervention was obtained in 260 (33.0%) of the case while 527 (67.0%) delayed consent and constituted the DC group. The range of the delay for DC was 1.25 to 72 hours with a mean of 4.5 + 3.5 hours.
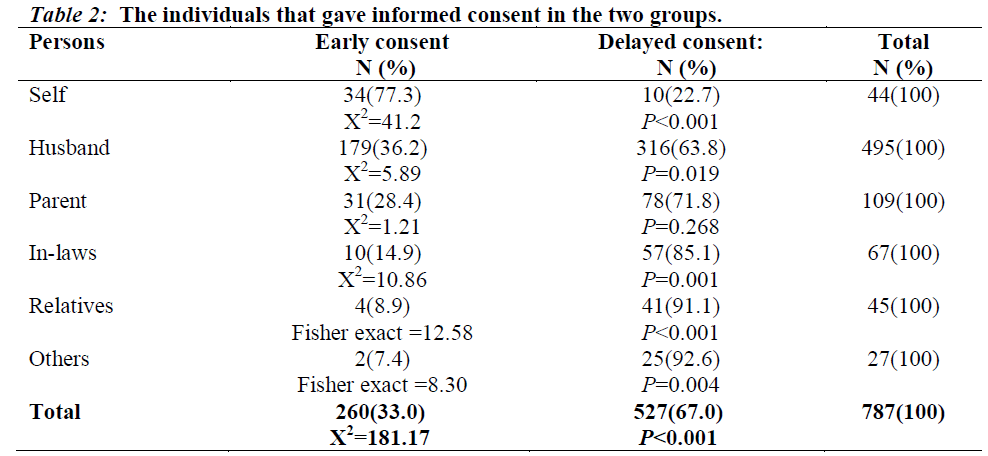
In 495 (62.9%) of cases the consent was given by the husband, 44 (5.6%) was given by the patient while the parents, in-laws, relatives and others were responsible for 109 (13.8%), 67 (8.5%), 45 (5.7%) and 27 (3.4%) respectively. There was significant difference in the dexterity to give consent by the various individuals responsible as shown in table 2. Consent was more readily gotten when it was given by the patient and 34/44(77.3%) of the patients gave EC (P<0.001). Consent was more likely to be delayed when it was given by the husbands (P=0.019), in-laws (P=0.001) and relatives (P<0.001).
Patients that gave consent for their own treatment were more likely to be gainfully employed (P=0.001), educated (P=0.004) and booked (P=0.001) as shown in table 3.
Table 4 shows the various interventions offered to treat these emergencies and the informed consent obtained. Consent was more readily obtained for instrumental vaginal delivery and IOL with 90/113 (79.6%) and 52/66 (78.8%) of the case giving EC. Emergency cesarean section had the highest case of DC 218/244 (89.3%).
| Intervention | Early consent (%) | Delayed consent (%) | Total |
|---|---|---|---|
| Blood transfusion | 82 (24.4) | 254 (75.6) | 336 |
| Emergency C/S | 26 (10.7) | 218 (89.3) | 244 |
| Instrumental Vaginal delivery | 90 (79.6) | 23 (20.4) | 113 |
| Induction of Labour | 52 (78.8) | 14 (21.2) | 66 |
| Destructive operation | 10 (35.7) | 18 (64.3) | 28 |
Table 4: The Relationship between the Obstetric interventions and Informed consent
Maternal mortality was significantly higher in the DC group compared to the EC group (P=0.010). Other complications including uterine rupture, sepsis and VVF were also higher in the DC but the differences were not statistically significant (P=0.448, 0.150, and 0.740 respectively) as shown in table 5. In all 841 babies delivered, 278 were born to the EC group while 563 were delivered to the DC group. Intrauterine fetal death (IUFD) (P= 0.016), low Apgar score (P=0.026) and early neonatal death (P=0.032) were higher in DC group as shown in table 5.
| Complications | Early consent | Delayed consent | TotalN (%) | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| • | Maternal death | 5(15.2) | 28(84.8) | 33(100) |
| X2=4.98 | P=0.026 | |||
| • | Sepsis | 15(28.3) | 38(71.7) | 53(100) |
| X2=0.58 | P=0.448 | |||
| • | Uterine rupture | 10(47.6) | 11(52.4) | 21(100) |
| X2=2.09 | P=0.150 | |||
| • | VVF | 2(40.0) | 3(60.0) | 5(100) |
| Fisher exact=0.11 | P=0.740 | |||
| • | IUFD | 8(17.0) | 39(83.0) | 47(100) |
| X2=4.73 | P=0.016 | |||
| • | Low Apgar scores | 25(23.6) | 81(76.4) | 106(100) |
| X2=4.92 | P=0.026 | |||
| • | ENND | 4(14.3) | 24(85.7) | 28(100) |
| Fisher exact =4.61 | P=0.032 | |||
NB: VVF=Vesico-Vaginal Fistula, IUFD=Intrauterine Fetal Death, ENND=Early Neonatal Death
Table 5: Maternal and fetal complications
Discussion
The provision of emergency obstetric care services to effectively handle obstetric complications is perhaps the most effective means of reducing maternal deaths in developing countries. However, women with these complications need to give an informed consent before some of these services can be rendered by the healthcare providers. Obtaining an informed consent promptly may be a challenge in culturally diverse settings where understanding of diseases may differ; decisionmaking may be both collective and individual coupled with the fact that the woman is not culturally empowered to give consent. [16]
Most of the consents in this study were given by the husbands and this further buttress the deeply rooted subordination of women to men in the society. This low status of women has persisted in most developing countries and forms the basis of gender discrimination and other practices that lay the foundation for the prevalent high maternal mortality in these regions.[9] Our finding showed that, only a small percentage of the women can give consent and this conformed to the finding in other part of the country.[11] We also found that, it is only when the consent is given by the patient that EC easily obtains and those that are gainfully employed, educated and booked are more likely to give EC. With good counselling, the women appreciate the magnitude of their problems and are willing to consent for emergency obstetric intervention to save their lives. However, the cultural setting may not permit them to consent for the treatment without the approval of their husbands. Obviously, there is the need to liberate our women from this retrogressive culture so that they take critical life-saving decisions. This can be achieved with better education and economic empowerment of the women. The high level of illiteracy and unemployment among the studied patients could also explain why only a few of them gave consent and this concurred with the finding of Irabor and Omonzejele, 2009 in Ibadan, Nigeria.[8]
The husbands also offer some glimpse of hope as over a third of them gave EC. Unfortunately, even the husbands are sometimes not empowered to give consent in the society especially if he cannot bear the financial burden of the treatment. In this situation, the consent will be given by the parent, in-laws or other relatives as obtained in the study. These people often do not accompany the patient to the hospital and reside in remote areas. The logistics in reaching out to them often leads to the delay in obtaining consent.
Overall, about a third of the cases gave EC for obstetric interventions. The highest number of EC was for instrumental vaginal deliveries and IOL which are the least invasive of the emergency obstetric interventions. This may be because the procedures may not involve general anesthesia and are perceived to involve minimal risk to the mother and fetus. Destructive operation also enjoyed over a third of EC because the surgical operation is on the dead fetus and the procedure does not leave surgical scars on the woman. For emergency cesarean section, abysmal 10.7% gave EC. This may not be unconnected to the general aversion for surgery by our women and some women might feel that there is the loss of an idealized delivery they had hoped for during pregnancy.[9] For these reasons they may be reluctant to give consent until it is affirmed by the husbands, parents or in-laws which often lead to undue delay in instituting treatment.
In emergency obstetric, timely intervention is the hallmark of good clinical practice for both maternal and fetal survival. Maternal death was commoner among the DC group. This may be because irreversible damages could have occurred before consent was given and therefore the patient could not be revived. Prophylactic antibiotic cover is universal in all emergency Cesarean section in our centre; hence delay in giving consent did not increase the risk of sepsis. Our routine practice of continuous drainage of bladder by Foleys catheter for 7 – 10 days after prolonged obstructed labour could explain why the occurrence of Vesico-vaginal fistula was also similar in the 2 groups. The fetus is particularly vulnerable and any delay in obtaining consent will affect it negatively, hence fetal complications were higher in the DC group. The process of obtaining informed consent from our diverse socioeconomic environment could be very challenging to the untrained practitioner. This study thus highlights some variables that could affect the patient’s attitude towards informed consent. However, some compounding variables were not controlled for and cases were not matched. A larger multi-centre study is required to validate the findings.
Conclusion
Delay in obtaining consent is an unforeseen contributor to maternal and neonatal morbidity and mortality our environment as it increases the 3rd level of delay in the health facility, a delay that is otherwise attributed to inadequacies of the health facility. Informed consent can be obtained from the husbands or the legal guardians at booking or during antenatal visit for comprehensive obstetrics care interventions. This will allow prompt institution of treatment and could reduce maternal morbidity and mortality in our environment. Advocacy to the community in order to encourage the husbands and legal guardians to accompany the women to the hospital during emergencies can also help. Similarly, we advocate for the girl child education and gainful employment of the women for economic empowerment.
References
- Paterick TJ, Carson GV, Allen MC and Paterick TE. Medical Informed Consent: General Considerations for Physicians. Mayo Clin Proc 2008; 83(3):313 – 9.
- Lawal YZ, Garba ES, Ogirima MO, Dahiru IL, Maitama MI and Abubakar K. The doctrine of informed consent in surgical practice. Ann Afr Med 2011; 10: 1-5.
- Edwards KA. Informed consent. University of Washington School of Medicine: 1998. Available from: http://depts.washington.edu/bioethx/topics/ consent.html [accessed 02/04/2011].
- Peters M. In: M Peters, editor. The British Medical association Illustrated medical dictionary. Second edition, London. Dorling Kindersley 2008; p. 142.
- Gillon R. Philosophical Medical Ethics - Consent. BMJ 1985; 297: 1700-1.
- Liesegang TJ. The meaning and need for informed consent in research. Indian J Ophthalmol 2007; 55: 1-3.
- Chafe SM. Legal obligation of physicians to disclose information to patients. Can Med Assoc J 1991; 144(6): 681–5.
- Chukwudebelu WO. Preventing maternal mortality in developing countries. Contemporary Obstetrics and Gynecology for developing countries. In Friday Okunofua and Kunle Odunsi, editors. Published by Women Health and Action Research Centre, Benin City, Nigeria 2003: 644-7.
- Irabor DO and Omonzejele P. Local attitudes, moral obligation, customary obedience and other cultural practices: their influence on the process of gaining informed consent for surgery in a tertiary institution in a developing country. Dev World Bioeth 2009; 9(1): 34-42.
- Ezeome ER and Marshall PA. Informed consent practices in Nigeria. Dev World Bioeth 2009; 9(3): 138-48.
- Maine D: Too far to walk: maternal mortality in context. Soc Sci Med 1994; 38: 1091-110.
- Mairiga AG, Kawuwa MD and Kyari O. A fourteen year review of maternal mortality at the University of Maiduguri Teaching Hospital, Maiduguri, Nigeria. Nig Hosp Pract 2008; 2(5): 115-9.
- Bukar M, Audu BM, Yahaya UR and Melah GS. Anemia in pregnancy at booking in Gombe, North-eastern Nigeria. J Obstet Gynaecol 2008; 28(8): 775-8
- Ehrenstein V. Association of Apgar scores with death and neurologic disability. Clin Epidemiol 2009; 1: 45–53.
- World Health Organisation (WHO). Neonatal and perinatal mortality: country, regional and global estimates. World Health Organization, Geneva 2006.
- Leclercq WKG, Keulers BJ, Scheltinga RM, Spauwen PHM, and Wilt GJ. A Review of Surgical Informed Consent: Past, Present, and Future. A Quest to Help Patients Make Better Decisions. World J Surg 2010; 34(7): 1406–15.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.