Intravenous Ketamine for Prevention of Post Anesthetic Shivering In Urological Procedures Done Under Spinal Anesthesia: A Randomized Triple Blinded Placebo Controlled Trial
Received: 06-Dec-2022, Manuscript No. amhsr-22-84695; Editor assigned: 26-Dec-2022, Pre QC No. amhsr-22-84695 (PQ); Reviewed: 28-Dec-2022 QC No. amhsr-22-84695; Revised: 13-Jan-2023, Manuscript No. amhsr-22-84695 (R); Published: 30-Jan-2023
Citation: Pushparani A, et al. Intravenous Ketamine for Prevention of Post Anesthetic Shivering in Urological Procedures Done under Spinal Anesthesia: A Randomized Triple Blinded Placebo Controlled Trial. Ann Med Health Sci Res. 2023;13: 425-430
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background and Aim: Post anesthetic shivering is one of the common complications following spinal anaesthesia. Adding to patient discomfort, it also causes increase in oxygen consumption, metabolic rate, carbon-dioxide production, hinderance in monitoring. The aim of this study is to compare the efficacy of prophylactic intravenous ketamine with 0.9% saline (placebo) in prevention of postoperative shivering in patients undergoing urological procedures under spinal anaesthesia.
Methods: 60 patients between ages 18-65 years, ASA status I–II, scheduled for urological procedures were prospectively studied. In this double-blind, randomized controlled trial, patients were randomly divided into group K(Ketamine 0.3 mg/kg) and group P(0.9% saline). After induction of SA, patients were observed for the incidence and intensity of shivering using a four-point scale by a blinded outcome assessor who is unaware of the drug given. Data collection was done by observation and measurement of various parameters.
Results: Incidence of shivering was increased in group P (93%) compared to group K(60%), with P value >0.0001. The result was very statistically significant. Time of onset of shivering was earlier in group P (29.30 ± 5.35) compared to group K (43.03 ± 4.3). P value equals >0.0001, the result was extremely statistically significant. 13% patients developed hallucination and 20% patients developed delirium and hypersalivation and 6.6% of patients had nystagmus with ketamine.
Conclusion: Incidence of shivering was increased in group P (93%) compared to group K(60%), with P value >0.0001. The result was very statistically significant. Time of onset of shivering was earlier in group P (29.30 ± 5.35) compared to group K (43.03 ± 4.3). P value equals >0.0001, the result was extremely statistically significant. 13% patients developed hallucination and 20% patients developed delirium and hypersalivation and 6.6% of patients had nystagmus with ketamine.
Keywords
Anesthesia; Spinal; Delirium; Hallucinations; Ketamine; Shivering; Tachycardia
Introduction
Shivering is involuntary, rapid, repeated oscillatory muscular contractions augmenting metabolic heat production. Post anesthetic shivering has deleterious effects like hypoxia, metabolic acidosis, hypercarbia. Neuraxial anesthesia does not inhibit central thermoregulation[1,2]. Vasoconstriction and shivering above the level of the neuraxial block is inadequate as muscle mass cephalad to the block is small [3]. NMDA receptor modulates noradrenergic and serotoninergic neurons in locus coeruleus and interferes with thermoregulatory control mechanisms in brain. Ketamine, competitive N-Methyl-DAspartate (NMDA) receptor antagonist, may have effect on shivering. So, we intend to compare the efficacy of prophylactic intravenous ketamine (0.5 mg/kg) with 0.9% saline in this study.
Materials and Methods
After obtaining institutional ethical committee clearance and informed consent (CTRI/2022/10/046406), 60 patients between the age group of 18-65 who were to undergo urological procedures under subarachnoid block were included. Patients not fit for spinal anaesthesia. Hypertensive patients, Patients with raised intra cranial pressure, patients with Coagulopathy and Seizure disorder were excluded. Informed consent written in their own language was obtained from all the patients. Fasting was advised for 6 hours. Baseline vitals were recorded. Baseline axillary temperature was recorded with thermometer. IV line was secured with 18 G IV cannula and pre warmed crystalloids were kept on flow. Under aseptic precautions, sub arachnoid block was administered using 25 gauge Quincke’s needle at L3-L4 intervertebral space by midline approach. Hyperbaric bupivacaine 2.8 ml of 0.5% solution was injected intrathecally.
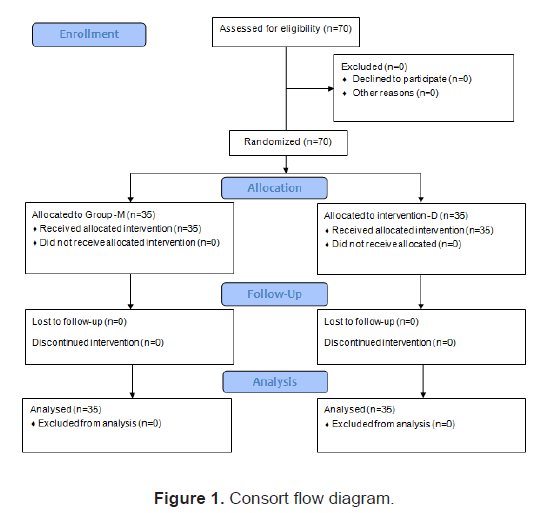
Patients were randomly allocated into two groups by computer generated random assignment prior to the start of the study (Figure 1).
The patient, the anaesthetist who administer the agent and the principal investigator were not aware of the group allocation. Group K received 0.5 mg/kg of injection ketamine intravenously and Group P received normal saline. The drugs were given by an anaesthetist who was not involved in the management of patients. Study drugs were prepared and diluted to a volume of 5 ml and were presented as coded syringes. Supplemental oxygen (5 L/min) was administered by face mask during the operation and recovery period. All intravenous fluids and irrigation fluids were pre-warmed to 37℃. The operating room temperature was maintained at 24℃-28℃. Patients were kept under close observation for the incidence and intensity of shivering. Axillary temperature was recorded at 10 min intervals during the perioperative period. Heart Rate (HR), systolic blood pressure, diastolic blood pressure, oxygen saturation (SpO2) and sedation score were monitored every 5 min for initial 30 min and subsequently for every 15 min till the end of surgery. Side-effects such as nausea, vomiting, hypotension, bradycardia, tachycardia, hallucinations, sedation, and nystagmus were noted. Time from SA to the beginning of shivering and duration of surgery were recorded. Patients were covered with one cotton blanket and no active warming were used. Presence of shivering was graded by using Tsai and Chu validated shivering scale by the attending anaesthetist who is not aware of the patient group[4]:
• No shivering.
• Piloerection or peripheral vasoconstriction, but no visible shivering.
• Muscular activity in only one muscle group.
• Muscular activity in more than one muscle group, but not generalized.
• Shivering all over the body.
If shivering grade 3 and 4 occurred was considered as severe shivering and a rescue intravenous Tramadol 100 mg with Ondansetron 4 mg was given and prophylaxis was considered ineffective. Incidence of shivering was assessed by a blinded outcome assessor who is unaware of the group the patient is allocated to. At the end of the surgery, patients were transferred to postoperative ward/ PACU. Assessment of side effects and other study outcome variables were continued for 24 hours. The ambient temperature of PACU was maintained at 24℃ to 28℃. Hypotension and bradycardia were defined as decrease in mean arterial pressure and heart rate of more than 20% from baseline. Hallucination was defined as an experience in which patient’s report that they see, hear, feel or smell something that does not exist. The depth of sedation will be quantified according to Ramsay sedation score as.
• Agitated.
• Tranquil and calm
• Sleeping but responds to verbal.
• Sleeping, but brisk responds to glabellar tap.
• Sleeping with sluggish respond to glabellar tap or loud auditory stimulus.
• Asleep not responding to glabella tap or loud auditory stimulus.
If the patient’s HR decreased below 60 beats/min, 0.5 mg atropine was administered by the intravenous route. If the Mean Arterial Pressure (MAP) decreased more than 20% from baseline, 6 mg ephedrine through an intravenous bolus was administered and further intravenous infusion of lactated Ringer’s solution was required. If the patients developed nausea and vomiting, 10 mg metoclopramide was administered through the intravenous route.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS, Version 25) for Microsoft windows. Descriptive statistics (mean, standard deviation and frequency) were included. To compare categorical data, chi-square test was used and to compare the non-categorical data student t-test was used. Non normally distributed data was analysed using Mann U Whitney test. The results were expressed in 95% confidence interval. A p- value<0.05 was considered statistically significant.
Results
Distribution of age, gender, weight, height, BMI, ASA classification and duration of surgery was comparable between the two groups without any statistical significance. The preoperative hemodynamic parameters and temperature were compared and there was no statistical significance between the two groups. While comparing the mean heart rate in the intra operative period, increase in heart rate was noted in group K. The difference in heart rate between 5 to 30 minutes in Group K and Group P was found to be statistically very significant with a P value<0.0001 and the difference in the heart rate at 45 minutes was found to be statistically significant with P value of<0.05 (Table 1).
| HR | Group K mean | Group K Standard deviation | Group P mean | Group P Standard deviation | Confidence interval | P value |
|---|---|---|---|---|---|---|
| 5 min | 88.46667 | 7.959957 | 64.66667 | 6.914918 | 19.946 to 27.653 | 0.0001 * |
| 10 min | 97.26667 | 8.784521 | 60.9 | 6.661003 | 32.337 to 40.396 | 0.0001 * |
| 15 min | 105.1333 | 7.815693 | 64.03333 | 4.895341 | 37.729 to 44.470 | 0.0001 * |
| 20 min | 93.3 | 8.749975 | 65.7 | 4.094993 | 24.069 to 31.131 | 0.0001 * |
| 25 min | 89.5 | 11.0882 | 65.36667 | 3.995543 | 19.826 to 28.441 | 0.0001 * |
| 30 min | 82.17241 | 5.874089 | 73.46667 | 7.185874 | 5.314 to 12.098 | 0.0001 * |
| 45 min | 76.42308 | 6.191433 | 72.64286 | 5.18698 | 0.828 to 6.732 | 0.013 ** |
| 60 min | 74.32 | 6.644045 | 72 | 5.43493 | -0.817 to 5.457 | 0.1442 |
Table 1: Comparison Herat rate between the groups
Note: *Non-significant,†Significant, ‡ Very highly significant.
Other intra operative hemodynamic parameters were comparable without any statistical significance. Group P had a significantly higher shivering score between 10–60 minutes compared to group K (Table 2).
| Shivering Score | Group K | Group P | U test | P value |
|---|---|---|---|---|
| 0 | 12(40%) | 2(6.6%) | 160.5 | <0.0001‡ |
| 1 | 6(20%) | 1(3.3%) | ||
| 2 | 11(36.6%) | 14(46.6%) | ||
| 3 | 1(3.3%) | 13(43%) | ||
| 4 | 0(0%) | 0(0%) | ||
| Median (Q3-Q1) | 2(3-2) | 2(2.25-2) |
Table 2: Comparison of Shivering score between the groups
Note: *Significant, †Significant, ‡Very highly significant
Group K had significantly higher sedation score between 15 and 30 minutes (Table 3).
| Sedation Score | Group K | Group P | U Test | P value |
|---|---|---|---|---|
| 1 | 0(0%) | 0(0%) | 302.5 | 0.03* |
| 2 | 14(46%) | 22(73%) | ||
| 3 | 10(33%) | 8(26%) | ||
| 4 | 6(20%) | 0(6%) | ||
| 5 | 0(0%) | 0(0%) | ||
| 6 | 0(0%) | 0(0%) | ||
| Median(Q3-Q1) | 2(3-2) | 2(2-2) |
Table 3: Comparison of Sedation score between the groups
Note: *Significant, † Significant
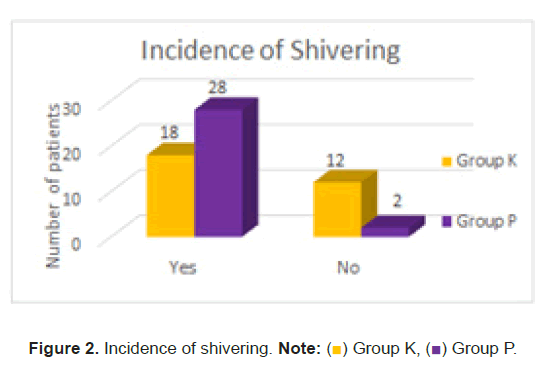
All the post-operative hemodynamic parameters were without any statistical significance except heart rate which was increased in group K compared to group P. Post-operative temperature showed a P value>0.0001 and was statistically very significant. Group P had a higher shivering score (Figure 2) and higher incidence of shivering (Figure 3).
Compared to patients in group K with extreme statistical significance at P<0.05. Post-operative sedation score was statistically significant with patients in group K had a higher sedation score. P value was 0.03. 60% of patients (18/30) had shivering in group K and 93% of patients (28/30) had shivering in group P. 13% patients developed hallucination and 20% patients developed delirium and hyper salivation and 6.6% of patients had nystagmus with the administration of ketamine.
Discussion
Although different drugs like 5-Hydroxytryptamine receptor (5-HT) antagonists and Tramadol have been, only Intravenous (IV) pethidine has shown promising result. However, in limited resource setting pethidine is not readily available and can cause respiratory depression, hypotension, sedation, itching, nausea, and vomiting. Respiratory depression and hypotension can lead to decreased oxygen delivery to body tissues which may result in organ damage. Itching, nausea, and vomiting can cause patient discomfort and distress. The use of readily available drugs even in non-operating room settings such as ketamine (NMDA receptor antagonist) has a wide safety margin, may serve as an alternative in both preventing and management of shivering after spinal anesthesia and results in reduced morbidity and discomfort associated with post spinal shivering.
There are many studies that compare the efficacy of various drugs in treating shivering after its incidence, but knowing the many deleterious effects of shivering, particularly in vulnerable population like the geriatrics and paediatrics, this study aimed in finding a drug that can be used prophylactically, with minimal side effects, easily available and cost effective.
Gecaj-Gashi, et al., reported that prophylactic low-dose IV ketamine 0.5 mg/kg was effective in preventing postoperative shivering, and no complications were noticed in their study, but with 0.75 mg/kg of ketamine undesired psychological reactions like vivid dreaming, floating sensation, visual and auditory hallucinations was noticed [5].
Arafath, et al., combined ondansetron 4 mg with Ketamine 0.25 mg/kg was advantageous compared to ondansetron 8 mg or Ketamine 0.5 mg/kg with minimal possible side effects[6]. This may be attributed to synergistic effect of both drugs by dual mechanisms of action when given prophylactically for prevention of PAS.
Therefore, a dose of 0.5 mg/kg of intravenous ketamine was used in this study.
Our study revealed a decrease incidence of shivering among the patients who received prophylactic ketamine by 1.5-fold when compared with those that received saline as placebo, with 60% incidence in ketamine group and 93% in placebo group. In the study done by Dal, et al. shivering rate was 57% in the control group [7]. In the study by Sagir, et al., the shivering rate was 55% in the control group [8]. Rabi, et al., did a similar study with similar dose of ketamine and found that the incidence of shivering was 42.50% in the control group [9]. Shivering was observed in 36% in Kose, et al., study. In the study of Sagir and Dal, no premedication was used, as was in our study [10]. However, Kose, et al., and Rabi, et al., administered 10 mg of diazepam as premedication. The relatively low incidence of shivering in the control group may be attributable to anti shivering property of diazepam. In a study conducted by Mohammadzadeh, et al., 12 53.5% of patients who received low dose of ketamine had shivering compared to 64.6% of patients who had shivering in the placebo group [11].
The incidence of shivering was found to be only 13.79% in the study conducted by Ramyavel, et al. in which a bolus dose of 0.2 mg/kg of ketamine was given followed an infusion of 0.1 mg/ kg/hr throughout the surgery [12]. The reduced incidence may be due to the fact that continuous infusion would maintain a steady state plasma concentration and also show a steady decline after stopping the drug.
The higher incidence of shivering in our study compared to the other studies maybe due to the type of surgery included. Ureteroscopy is usually performed with continuous fluid irrigation to improve the visibility, either for clearance of calculi and debris or to clear small venous blood. This results in hypothermia and shivering which becomes pronounced further when the patient is under neuraxial blockade.
Han, et al., did a study in which he compared 0.2 mg/kg vs. 0.4 mg/kg of ketamine given via epidural catheter along with 0.75% ropivacaine [13]. It was shown that the incidence of shivering in patients who received epidural ketamine 0.2 mg/kg or 0.4 mg/ kg was 3.1% and 0%, respectively.
In our study, none of the patients in ketamine group experienced grade four of shivering, whereas, three patients in the placebo group had grade four shivering.
In a study conducted by Wason, et al., intravenous ketamine, clonidine and tramadol were compared and they found out that in the control group, 27 patients (54%) exhibited grade 3 shivering; however, only five patients (10%) in the ketamine group exhibited grade 3 shivering, which was significantly more than our study in which only 3.3% of the patients experienced grade 3 shivering in ketamine group and 43% in the control group [14].
Mohammadzadeh, et al., compared ketamine, tramadol and ondansetron and found that 9 patients who received ketamine (7% compared to 3.3% in our study) experienced grade 3 shivering and none exhibited grade 4 shivering compared to placebo group in which 29 patients experienced grade 3 shivering and 6 patients experienced grade 4 shivering. This increase in the incidence of grade 3 shivering maybe attributed to the fact that they used only 0.2 mg/kg of ketamine.
In the study conducted by Arafath, et al., where the efficacy of ketamine, ondansetron and ketamine with ondansetron were compared to prevent shivering in patients under general anaesthesia, 20% of the patients developed grade 3 shivering in placebo group and only 3.3% of patients developed grade 3 shivering with ketamine. Addition of ondansetron with ketamine did not produce significant reduction in the intensity of shivering.
Rabi, et al., showed that only 7.3% of patients who received ketamine showed grade 3 shivering and none experienced grade four compared to 41.5% in the placebo group and 4.8% patients showed grade 4 shivering.
Honarmand, et al., did a study comparing the efficacy of saline, ketamine, midazolam and ketamine with midazolam. Grade 4 shivering was observed in one patient in Group M and in one patient in Group C [15]. 37% patients (11/120) experienced Grade 3 shivering and requested treatment. In Group C, eight out of 30 patients experienced shivering at Grade 3. This was significantly higher than Groups K and KM
On reviewing these studies, it has become evident that ketamine not only reduces the incidence of shivering but also the intensity.
In our study, 33% patients exhibited grade three and 20% exhibited grade four sedation. None of the patients showed sedation grade 5 or 6. With 0.1 mg/kg/hr of ketamine infusion, Ramyavel et al., showed that there was 100% sedation of grade more than 3 in her study compared with only 19.35% in the placebo group.
Wason, et al., showed in her study that sedation score (grades 3 and 4) was significantly higher in the ketamine group than compared to clonidine and tramadol with 48% showing grade three and 6.4% showing grade 4 sedation, but a different scale was used to quantify the degree of sedation on a 5-point scale. 1=fully awake, 2=drowsy, 3=eyes closed, arousable to command, 4=eyes closed, arousable to mild physical stimulation and 5=eyes closed, unarousable to mild physical stimulation.
Kumar, et al., compared the efficacy of ketamine, tramadol and dexmedetomidine and showed that ketamine had sedation score superior to tramadol and similar to dexmedetomidine without the benefit of conscious sedation provided by dexmedetomidine [16].
Arafath, et al., showed higher postoperative sedation grades in the immediate recovery period and none had deep sedation, delay in recovery and time to discharge.
Sagar, et al., compared two doses of ketamine in the prevention of shivering and revealed that 15.6% of patients who received 0.5 mg/kg of ketamine showed grade 4 of shivering compared to the 6.3% of patients who received 0.25 mg/kg ketamine [17].
In Ramyavel’s study, bolus dose of 0.2 mg/kg ketamine followed by infusion of 0.1 mg/kg/hr was given and showed no difference in HR and MAP. The results were similar to the studies conducted by Shakya and Sagir who also showed no difference in hemodynamics parameters [18]. However, Rabi et al., showed that there was an increase in HR and SBP with ketamine as was the case in our study.
SBP and DBP and heart rate were significantly lower in group that received only 0.75% ropivacaine than in the other groups, but there was no significant difference in hemodynamic change between groups that received 0.2 mg/kg or 0.4 mg/kg of ketamine along with ropivacaine.
Rabi et al., showed that 2 patients had hallucinations and four patients developed delirium with ketamine. In our study, 13% patients developed hallucination and 20% developed delirium and hypersalivation and 6.6% of developed nystagmus with the ketamine.
Ramyavel, et al., showed that despite the use of continuous infusion of 0.1 mg/kg.hr of ketamine, no adverse effects were seen.
Sharma, et al., demonstrated with ketamine (0.5 mg/kg) 2 out of 30 patients developed hallucinations and 4 patients developed delirium. Han’s study showed that 2 patients experienced hallucinations with 0.4 mg/kg of epidural ketamine and no complications were noted in patients who received 0.2 mg/kg of ketamine epidurally [19].
Arafath showed that 3.3% of patients developed hallucinations and 6.6% of patients developed nystagmus with the administration of 0.5 mg/kg of ketamine.
Honarmand, et al., showed that 10% of patients developed hallucinations with ketamine and 6.7% of patients developed hallucinations with ketamine and midazolam.
Mohammadzadeh, et al., compared ketamine, tramadol and ondansetron and found that 9 patients who received ketamine (7% compared to 13% in our study) experienced hallucinations, 10.2% of patients had nystagmus and 3.9% had headache.
Conclusion
We conclude that ketamine 0.5 mg/kg reduces the incidence of shivering and also the intensity of shivering. Patients who did not received ketamine developed shivering earlier than those who received ketamine. Despite reducing the incidence of shivering, complication associated with the administration of ketamine like tachycardia, nystagmus, hallucinations, delirium, hypersalivation were seen in patients who received ketamine.
References
- de Witte J, Sessler DI. Perioperative shivering: Physiology and pharmacology. Anesthesiology. 2002;96:467-84.
[Crossref], [Google Scholar], [Indexing]
- Bhattacharya P, Bhattacharya L, Jain R, Agarwal R. Postanaesthesia Shivering (PAS): A review. Indian J Anaesth. 2003;47:88-93.
- Díaz M, Becker DE. Thermoregulation: Physiological and clinical considerations during sedation and General Anesthesia. Anesth Prog. 2010;57:25-32.
[Crossref], [Google Scholar], [Indexing]
- Tsai YC, Chu KS. A comparison of tramadol, amitriptyline, and meperidine for postepidural anesthetic shivering in parturients. Anesth Analg. 2001;93:1288-92.
[Crossref], [Google Scholar], [Indexing]
- Gecaj-Gashi A, Hashimi M, Sada F, Salihu S, Terziqi H. Prophylactic ketamine reduces incidence of postanaesthetic shivering. Niger J Med. 2010;19:267-70.
[Crossref], [Google Scholar], [Indexing]
- Arafath AA. Use of ondansetron, ketamine or their combination for prevention of post-anesthetic shivering. 2014.
- Dal D, Kose A, Honca M, Akinci SB, Basgul E, et al. Efficacy of prophylactic ketamine in preventing postoperative shivering. Br J Anaesth. 2005;95:189-92.
[Crossref], [Google Scholar], [Indexing]
- Sagir O, Gulhas N, Toprak H, Yucel A, Begec Z, et al. Control of shivering during regional anaesthesia: Prophylactic ketamine and granisetron. Acta Anaesthesiol Scand. 2007;51:44-49.
[Crossref], [Google Scholar], [Indexing]
- Mb R, Ado S, B C. Prophylactic ketamine for prevention of post-spinal shivering: Randomised controlled trial. Anesth Crit Care. 2019;01: 039-047.
- Kose EA, Honca M, Dal D, Akinci SB, Aypar U. Prophylactic ketamine to prevent shivering in parturients undergoing Cesarean delivery during spinal anesthesia. J Clin Anesth. 2013 Jun;25(4):275-80.
[Crossref], [Google Scholar], [Indexing]
- Mohammadzadeh Jouryabi A, Sharami SH, Mansour Ghanaie M, Sedighinejad A, et al. Comparing the effects of low dose of ketamine, tramadol, and ondansetron in prevention of post spinal anesthesia shivering in Cesarean section. Anesthesiol Pain Med. 2021;11:e116429.
[Crossref], [Google Scholar], [Indexing]
- Thangavelu R, George SK, Kandasamy R. Prophylactic low dose ketamine infusion for prevention of shivering during spinal anesthesia: A randomized double blind clinical trial. J Anaesthesiol Clin Pharmacol. 2020;36:506-10.
[Crossref], [Google Scholar], [Indexing]
- Han DY, Jeong HJ, Lee C, Choi DH. The efficacy of epidural ketamine on shivering during transurethral resection of the prostate under epidural anesthesia. Int Neurourol J. 2010;14:105-11.
[Crossref], [Google Scholar], [Indexing]
- Wason R, Jain N, Gupta P, Gogia AR. Randomized double-blind comparison of prophylactic ketamine, clonidine and tramadol for the control of shivering under neuraxial anaesthesia. Indian J Anaesth. 2012;56:370-75.
[Crossref], [Google Scholar], [Indexing]
- Honarmand A, Safavi MR. Comparison of prophylactic use of midazolam, ketamine, and ketamine plus midazolam for prevention of shivering during regional anaesthesia: A randomized double-blind placebo controlled trial. Br J Anaesth. 2008;101:557-62.
[Crossref], [Google Scholar], [Indexing]
- Kumar RA, Ammu S. Comparing the efficacy of tramadol, ketamine and dexmedetomidine in the prevention of intraoperative shivering in patients undergoing surgery under subarachnoid blockade. Indian J Clin Anaesth. 2021;8:446-51.
[Crossref], [Google Scholar]
- Samimi Sadeh S, Hashemi E, Aminnejad R, Bastanhagh E. The impact of optimal dose of ketamine on shivering following elective abdominal hysterectomy: A randomised comparative study. Anesthesiol Pain Med. 2020;10:e106220.
[Crossref], [Google Scholar], [Indexing]
- Shakya S, Chaturvedi A, Sah BP. Prophylactic low dose ketamine and ondansetron for prevention of shivering during spinal anaesthesia. J Anaesthesiol Clin Pharmacol. 2010;26:465-69.
[Google Scholar], [Indexing]
- Sharma DR, Thakur JR. Ketamine and shivering. Anaesthesia 1990;45:252 53.

 ) Group K, (
) Group K, ( ) Group P.
) Group P.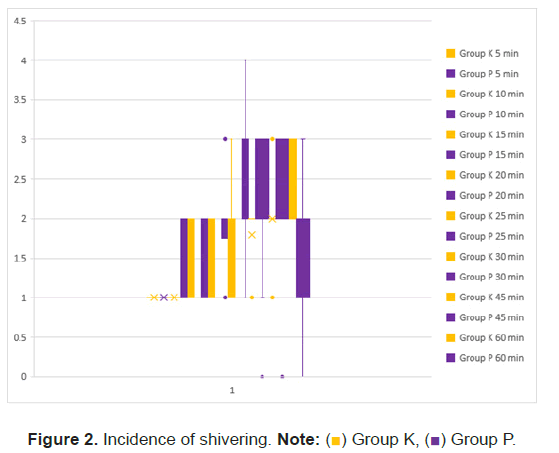



 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.