Knowledge and Attitude of Nurses in the Tamale Metropolis toward Kangaroo Mother Care (KMC)
2 University for Development Studies, School of Allied Health, Department of Nursing, Box TL 1350, Tamale, Ghana
3 University for Development Studies, Faculty of Agriculture, Department of Animal Science, P. O. Box TL 1882, Tamale, Ghana
Citation: Adzitey SP, et al. Knowledge and Attitude of Nurses in the Tamale Metropolis toward Kangaroo Mother Care (KMC). Ann Med Health Sci Res. 2017; 7: 454-459
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
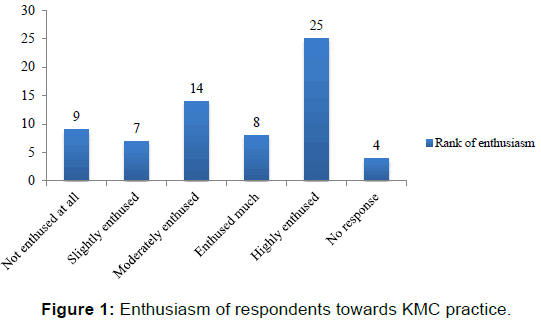
Background: The benefits of kangaroo mother care (KMC) will remain untapped if nurses do not demonstrate adequate knowledge and positive attitude toward it. Aim: The aim of this study was to assess the knowledge and attitude of nurses in the Tamale Metropolis of Ghana towards KMC and its practice. Materials and Methods: A cross-sectional descriptive study was conducted on 67 nurses selected from the four main hospitals in the Tamale Metropolis. A structured questionnaire comprising of both open and close ended questions was used. Data obtained was analysed using SPSS version 17.0. Results: Most of the nurses interviewed were between the ages of 21-30 years (71.6%) and had 1-5 years (76.1%) work experience. Sixty six (98.5%) of the nurses have heard about KMC, 51 (76.1%) had an idea about what KMC is and 16 (23.9%) were able to define KMC correctly. According to the nurses KMC can be given by mothers 66 (98.5%), fathers 42 (62.7%) and other family members 37 (55.2%). Also the group of babies requiring KMC are low birth weight babies 56 (83.6%), preterm babies 65 (97.0%), overweight babies 4 (6.0%), sick babies 10 (14.9%) and others 6 (9.0%). Twenty five (37.3%) of the nurses are usually highly enthused when assisting mothers to practice KMC, 8 (11.9%) are enthused much, 14 (20.9%) are usually moderately enthused, 7 (10.4%) are slightly enthused, 9 (13.5%) are not enthused at all in assisting mothers practice KMC and 4 (6.0%) did not answer the question. Fifty three (79.1%) of the nurses persuade mothers with preterm/low birth weight babies to practice KMC, 11 (16.4%) do not persuade them and three persons did not answer the question. Thirty four (50.7%) of the respondents do insist mothers practice KMC if they do not respond to persuasion, 30 (44.8%) do not insist that mothers practice KMC if persuasion fails and three of them did not answer the question. Conclusion: A good number of nurses in the Tamale Metropolis have a positive attitude towards KMC but lack adequate knowledge on its benefits and how to ensure a successful implementation. There is therefore the need
Keywords
Attitude; Kangaroo mother care; Knowledge; Nurses
Introduction
Kangaroo mother care (KMC), also called kangaroo care or skin-to-skin care is a method of care for preterm babies in which babies are carried skin-to-skin with their mother and sometimes the father. [1] It was developed in 1979 by Rey and Martinez in Bogota, Colombia in order to augment the shortage of incubators and to help reduce hospital infections. [1,2] Kangaroo mother care was developed to serve as alternative to care for preterm and low birth weight (LBW) babies who were stable and did not require continuous medical care. [3] It has proven to be effective in meeting a baby’s needs of warmth, breastfeeding, protection from infection, stimulation, safety and love. [1] According to WHO. [1] the key features of kangaroo mother care include early, continuous and prolonged skin-to-skin contact between the mother and the baby, exclusive breastfeeding, early discharge of small babies, the need for follow up and support for mothers, and it is a gentle and effective method that avoids the agitation routinely experienced in a busy ward with preterm infants.
Beck et al. [4] reported that approximately 13 million babies are born prematurely worldwide, of which 11 million are born in Asia and Africa. Global Action Report on preterm birth indicated that, about 15 million babies were born too soon worldwide representing 1 out of 10 babies born prematurely. [5] Prematurity is considered to account for 27% of four million neonatal deaths annually. [4] Prematurity is now the second-leading cause of death worldwide in children under age 5 and preterm birth rates is increasing in almost all countries with reliable data. [6] The report released in May 2012 indicated that the figure for preterm births in 2010 for Ghana was 111,500 constituting 14.5% of live births recorded in Ghana. [5] Out of this number, 7,800 died from complications related to preterm birth. [5] There is therefore the need to employ simple and inexpensive methods such as kangaroo mother care to help reduce these deaths.
About twenty years of implementation and sufficient research have proved that the benefits of kangaroo mother care are more than just an alternative to incubator care. [7] According to Conde- Agudelo and Díaz-Rossello. [8] Kangaroo mother care reduces morbidity and mortality of low birth weight infant. Liyanage. [3] recommended in his work that countries with scarce resources should adopt kangaroo mother care to minimize problems associated with the management of preterm and low birth weight infants. Kangaroo mother care is beneficial for temperature regulation, bonding (mother/father and baby) and breastfeeding of all neonates irrespective of weight, gestational age and clinical condition. [1] Despite the importance of kangaroo mother care, no research has been conducted about the knowledge and attitude of Nurses in the Tamale Metropolis and thus the reason for carrying out this study.
Materials and Methods
The study was conducted in four hospitals in the Tamale Metropolis namely Tamale Teaching Hospital, Central Hospital, West Hospital and SDA Hospital. Tamale Teaching Hospital has a bed capacity of 465 and its neonatal intensive care unit (NICU) has a bed capacity of 35; Central hospital has a bed capacity of 186 and a NICU with a bed capacity of 8; West and SDA hospitals have bed capacities of 150 and 120, respectively have no NICUs.
These facilities were purposively selected since they are the four main hospitals in the Tamale Metropolis. However, nurses sampled from these facilities were selected randomly. A crosssectional descriptive design was used to obtain both quantitative and qualitative data. Using Cochran’s formula for sample size calculation, a sample size of sixty eight (67 respondents) was used. [9] Cochran’s formula defines sample size as n= t2x p (1- p)/m2, where n=required sample size, t=the z score associated with the confidence level required (e.g. a confidence level at 90% has a standard value of 1.64), p=the population prevalence of the attribute being studied (use 50% if you are not sure of the population prevalence), m= margin of error. A confidence level of 90% and 10% margin of error was used; t=1.64, p=50% (0.5), 10% (0.1). Hence n=1.642 × 0.5 (1-0.5)/0.12; n=2.69 × 0.25/0.01, n=67.25; Therefore n=67. A structured questionnaire comprising both open and close ended questions was designed and used for data collection. The questionnaire was validated by all authors and pre-tested prior to administration using seven nurses. Appendix 1 shows a sample of the questionnaire used in this study. Data was analyzed using Statistical Package for the Social Sciences (SPSS) version 17.0.
Results
Gender, age, education and experience of respondents
The sex, age, educational level and work experience of the respondents (nurses) are shown in Table 1. Majority of the nurses were females 53 (79.1%), aged between 21-30 yrs, 48(71.5%), are diploma holders 36 (53.7%) and had 1-5 years’ working experience 51 (76.1%). Thirty (44.8%) of the nurses work in the neonatal intensive care (NICU), whereas 37 (55.2%) were non-NICU staff, these non-NICU staff work in antenatal clinic (ANC) (7), child welfare clinic (CWC) (2), maternity ward (20) and children’s ward (8).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Females | 53 | 79.1 |
| Males | 14 | 20.9 |
| Age | ||
| 21-30 | 48 | 71.6 |
| 31-40 | 11 | 16.4 |
| 41-50 | 6 | 9 |
| 51-60+ | 2 | 3 |
| Educational level | ||
| Certificate | 22 | 33 |
| Diploma | 36 | 53.7 |
| Bachelor degree | 9 | 13.4 |
| Experience (years) | ||
| 1-5 | 51 | 76.1 |
| 6-10 | 5 | 7.5 |
| 11-15 | 5 | 7.5 |
| 16+ | 6 | 9 |
Table 1: Age, work experience and educational status of respondents.
Knowledge, attitude and enthusiasm of respondents toward KMC practice
Sixty six (98.5%) of the nurses have heard about KMC, while only 1 (1.5%) did not respond to the question. The definition of KMC as given by the respondents is presented in Table 2. Most of the respondents 16 (23.9%) define KMC as placing baby in skin to skin contact with mother in between the mother’s breast to provide warmth, breastfeeding and bonding.
| Definition of KMC by respondents | Frequency | Percentage (%) |
|---|---|---|
| Placing baby in skin to skin contact with mother in between the mother’s breast to provide warmth, breastfeeding and bonding | 16 | 23.9 |
| Skin to skin contact between mother and baby | 12 | 17.9 |
| Care given to low birth weight and premature babies by parents/family | 6 | 9.0 |
| A way of handling premature babies by mother or father to provide warmth | 5 | 7.5 |
| Positioning baby on mother’s chest in between breast to provide warmth | 12 | 17.9 |
Table 2: Definitions of KMC by respondents.
The features/components of KMC as indicated by the nurses are shown in Table 3. From Table 3, the main features/ components of KMC include skin to skin contact 64 (95.5%) and family support to mother in practicing KMC 34 (50.7%); and exclude exclusive breastfeeding 35 (52.2%) and early discharge 46 (68.7%). Four nurses also indicated that, there are other feature(s) of KMC, 2 (3%) of them stated temperature regulation and the other 2 (3%) stated good personal hygiene as being other feature(s) of KMC.
| Variables | Yes | No | No response |
|---|---|---|---|
| Skin to skin contact | 64 (95.5%) | 2 (3.0%) | 1 (1.5%) |
| Exclusive breastfeeding | 31 (46.3%) | 35 (52.2%) | 1 (1.5%) |
| Early discharge | 20 (29.9%) | 46 (68.7) | 1 (1.5%) |
| Family support to mother in practicing KMC | 34 (50.7%) | 32 (47.8%) | 1 (1.5%) |
| Others (Specify) | 4 (6.0%) | 61 (91.0%) | 2 (3.0%) |
Table 3: Components/features of KMC.
Table 4 depicts the responses of the nurses regarding the category of babies that require KMC. Majority stated preterm babies 65 (97.0%) and low birth weight babies 56 (83.6%). Majority also stated that Overweight babies 63(94.0%) and sick babies 57 (85.1%) do not require KMC. It was noted by the respondents that KMC can be given by the mother 66 (98.5%), father 42 (62.7%) and other family members 37 (55.2%) to preterm/LBW babies.
| Variables | Yes | No |
|---|---|---|
| Low birth weight babies | 56 (83.6%) | 11(16.4%) |
| Preterm babies | 65 (97.0%) | 2 (3.0%) |
| Overweight babies | 4 (6.0%) | 63(94.0%) |
| Sick babies | 10 (14.9%) | 57 (85.1%) |
| Others | 6 (9.0%) | 61 (91.0%) |
Table 4: Group of babies requiring KMC.
Most of the respondents agreed that KMC helps in preventing hypothermia in newborns while transporting them to higher centers 58 (86.6%), can be practiced at home 66 (98.5%) and can safely be provided by HIV positive mothers to their babies 2(92.5%). Sixty two (92.5%) said KMC is beneficial to both mother and infant, 4 (6.0%) said it benefits only the infant and 1 person indicated it benefits only the mother. All the nurses 67 (100%) think KMC training is essential. Twenty eight (41.8%) of the nurses have been trained on KMC and more than half of the nurses 39 (58.2%) have not received any form of training on KMC.
Table 5 further depicts the nurses’ responses to questions regarding their knowledge of KMC as assessed using a 3-point Likert scale. Some responses include 47 (70.1%) of the nurses agree KMC can be initiated immediately after birth, 14 (20.9%) disagree it can be started immediately after birth. Sixty six (98.5%) agree KMC increases bonding between mother and baby. Thirty eight (38) (56.7%) agrees KMC reduces the rate of infections in newborns whereas 16 (23.9%) disagrees and 12 (17.9%) have no idea.
| No. | Variables | I agree | I disagree | I don’t know | No response |
|---|---|---|---|---|---|
| 1 | KMC can be initiated immediately after birth | 47 (70.1%) | 14 (20.9%) | 5 (7.5%) | 1 (1.5%) |
| 2 | KMC increase bonding between mother and baby | 66 (98.5%) | 0 (0%) | 0 (0%) | 1 (1.5%) |
| 3 | KMC enhances breast feeding | 57 (85.1%) | 4 (6.0%) | 5 (7.5%) | 1 (1.5%) |
| 4 | Family members should support mother in giving KMC | 62 (92.5%) | 1 (1.5%) | 3 (4.5%) | 1 (1.5%) |
| 5 | KMC increases self-confidence of the mother | 58 (86.6%) | 4 (6.0%) | 4 (6.0%) | 1 (1.5%) |
| 6 | KMC increases growth and development of the baby | 60 (89.6%) | 4 (6.0%) | 2 (3.0%) | 1 (1.5%) |
| 7 | KMC leads to reduce infection rate in the newborn babies | 38 (56.7%) | 16 (23.9%) | 12 (17.9%) | 1(1.5%) |
| 8 | KMC leads to early discharge and reduces hospital stay and cost to the family | 51 (76.1%) | 10 (14.9%) | 4 (6.0%) | 2 (3.0%) |
| 9 | KMC is beneficial to all babies despite birth weight | 40 (59.7%) | 21 (31.3%) | 5 (7.5%) | 1 (1.5%) |
Table 5: Benefits of KMC.
Figure 1 represents the enthusiasm of nurses towards assisting mothers to practice KMC assessed using a 5-point Likert scale, where 1 is not enthused at all, 2 is slightly enthused, 3 moderately enthused, 4 enthused much and 5 being highly enthused. Twenty five (37.3%) respondents said they are usually highly enthused when assisting mothers to practice KMC, 8 (11.9%) are enthused much, 14 (20.9%) are usually moderately enthused, 7 (10.4%) are slightly enthused and 9 (13.5%) are not enthused at all in assisting mothers practice KMC.
Twenty (29.9%) of the nurses talk to new mothers on the practice of KMC every day, 5 (7.5%) do it once a week and 2 (3.0%) did not answer the question. Out of the remaining 40 (59.7%) nurses, 24 (60%) of them do not talk about KMC to new mothers and the remaining 16 (40%) nurses only talk about KMC when necessary or when a preterm/LBW baby is born. Fifty three (79.1%) nurses persuade mothers with preterm/LBW babies to practice KMC, 11 (16.4%) do not persuade them and three persons did not answer the question. Thirty four (50.7%) nurses do insist mothers practice KMC if they do not respond to persuasion, 30 (44.8%) do not insist that mothers practice KMC if persuasion fails and three of them did not answer the question.
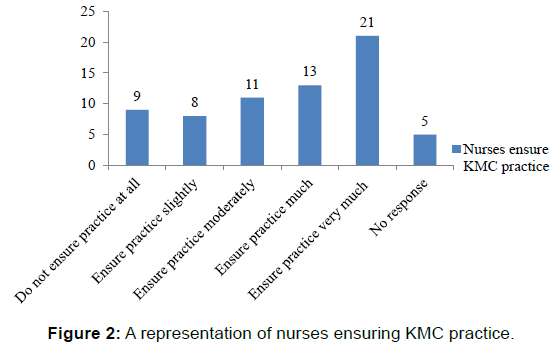
Figure 2 is a representation of nurses ensuring the practice of KMC ranked using a 5-point likert scale where 1 is do not ensure practice at all, 2 is ensure practice slightly, 3 is ensure practice moderately, 4 is ensure practice much and 5 is ensure practice very much. Twenty one (31.3%) nurses ensure the practice of KMC very much, 13 (19.4%) ensure the practice much, 11 (16.4%) and 8 (11.9%) ensure the practice moderately and slightly, respectively. Nine (13.4%) do not ensure the practice of KMC at all and 5 (7.5%) did not answer the question.
Discussion
The nurses who provided information for the study were composed of 53 (79.1%) females and 14 (20.9%) males. Majority of them were in an age bracket of 21-30 years, were diploma holders and had 1-5 years working experience. Kangaroo mother care (KMC) has consistently proven to be a safe and cost effective method of care of preterm/low birth weight (LBW) infants [10] and can be common among pregnant teenagers. [11] It is mainly a nursing procedure and its practice is usually ensured and supervised by nursing staffs in most health facilities where it is being practiced. For this reason, knowledge and attitude of nurses is important in the promotion of KMC. It was impressive to find that, almost all participants (98.5%) have heard about KMC. A good number of participants (16) were able to define KMC as “a method of placing baby in skin-to-skin contact with mother in between the mother’s breast to provide warmth, breastfeeding and bonding”. Most of the participants also stated that skin-to-skin contact 64 (95.5%) was a major component of KMC and KMC should start (70.1%) immediately after birth for every newborn to ensure that all babies stay warm in the first hours of life. The rest of the participants in this study have a fair idea of what KMC is. WHO [1] reported that skin-to-skin contact promotes lactation and facilitates the feeding interaction thus the baby on KMC is breastfed exclusively. In this study some nurses did not know that exclusive breastfeeding 35 (52.2%) and early discharge 46 (68.7) are among the components of KMC, this indicates that most nurses in the Tamale Metropolis think skin-to-skin contact is the only most important component of KMC. This idea is because they think the essence of KMC is only for thermoregulation and bonding as seen in the various definitions offered by participants (Table 2).
Preterm/LBW babies requiring incubator care for thermoregulation have an alternative in meeting their thermal needs which is KMC, in this study majority of participants indicated that preterm/LBW babies require it. The current findings has also shown that babies born at term and have a normal birth weight (2.5 kg to 4.2 kg) but suffer hypothermia can also benefit from KMC. Earlier studies by WHO [1] and Charpak et al. [7] pointed out that KMC is an important method for ensuring bonding, breast-feeding and thermal control of all new-born infants, regardless of weight, gestational age and clinical condition. This study has also found that quite a number of nurses (16.4%) do not know that babies with LBW require KMC. Low birth weight is a birth weight of a live born infant of less than 2.5 kg irrespective of gestational age. [1] In this study, 47 (70.1%) know that LBW is a birth weight less than 2.5 kg and 19 (28.4%) think a birth weight ranging from 1 kg to 2.5 kg is LBW. There is a little gap in knowledge regarding LBW among those who said LBW is 1 kg to 2.5 kg. Preterm on the other hand is defined as babies born alive before 37 completed weeks of gestation. [1] In this present study, 47 (70.1%) know that a baby that is born before 37 completed weeks of gestation is preterm, 14 (20.9%) think preterm babies are ones born from 1 week to 28 weeks whiles 5 (7.5%) said less than 40 weeks gestation. Sometimes the father or other family members can help the mother, replacing her for skin-to-skin contact with the baby so that she can get some rest. [1] In a study by Dalal et al. [12] 20 (13.8%) of participants knew that other family members can replace the mother for KMC. In the current study, 66 (98.5%) know KMC can be given by the mother, 42 (62.7%) know the father can offer KMC and 37 (55.2%) also know that other family members like grandmother, aunties etc can give KMC. In this regard, a baby requiring KMC whose mother is sick and cannot offer KMC, other family members can be asked to do it.
Studies have shown that continuous and prolonged skin-to-skin contact between a mother and her preterm/LBW infant, as seen in KMC is effective in providing instant physiological benefit such as thermoregulation. [1,7,13] In the present study, 58 (86.6%) know KMC helps in preventing hypothermia in newborns while transporting them to higher or referral centers. Also, 66 (98.5%) nurses know KMC can be practiced at home and 62 (92.5%) nurses agree that HIV positive mothers can safely provide KMC to their babies; one person out of the 62 nurses further added that provided there are no lesions on the mother’s skin. According to Udani and Nanavati [14] KMC is initiated in the hospital and continued at home as long as the baby needs and likes it. In this study, nurses were in a 100% support of training on KMC, stating that all nurses and midwives should be adequately trained on the subject. Twenty eight (41.8%) nurses who have had training on KMC were all NICU staffs and were trained by their ward incharges. Although most of the nurses (92.5%) know KMC is beneficial to both mother and infant, there is still quite a number (13.4%) who are not enthused in assisting mothers practice it. Engler et al. [15] reported that nurses, who perceived the practice of KMC to be beneficial to them (by decreasing their workload) and the infant, were more willing to implement KMC in their units. Nurses (29.9%) talk about KMC to mothers’ daily while 35.8% of nurses do not talk to mothers about KMC because they themselves (nurses) do not have adequate knowledge in the technique. Also they believe that talks on KMC are the preserve of NICU nurses since they are the ones who handle preterm/ LBW babies. Nurses (23.9%) talk to new mothers about KMC when a preterm/LBW baby is born. Nurses talk to mothers on KMC only when a preterm is born which suggest that there is no continuous education on KMC to mothers. For the technique to be effectively practiced, nurses who work with preterm/LBW infants should make it a daily routine to emphasize the benefits of KMC and also evaluate their knowledge.
Feldman et al. [16] reported that there is less depression reports among mothers who provide KMC for their premature babies in the neonatal unit and felt more confident, competent and more responsible in the care they provide for their infants. In the current study, nurses reported that mothers say KMC boost their self-confidence, they felt comfortable with the practice and the technique enables them to be closer to their babies’ whiles in the hospital. Other contrasting concerns expressed by mothers as reported by NICU nurses are; KMC is new to them and are afraid their babies will fall due to their fragile small body size. Most of the mothers do not like KMC as it is time wasting, some of them are petty traders and also peasant farmers who have to resume their trade in order to support the family. Nurses (79.1%) persuade mothers to practice KMC and some nurses in the NICU insist mothers practice KMC on their stable babies due to fewer incubators. As shown in Figure 2, 31.3% of nurses ensure very much the practice of KMC; whiles 13.4% do not ensure the practice of the technique at all. Since a good number of nurses have shown a positive attitude towards the practice of KMC, it is important that they are well equipped with the requisite information and practice guidelines. Furthermore, 37.3% of mothers practice KMC moderately as reported by nurses, 20.9% practice it slightly, 19.4% practice much and 16.4% do not accept to practice KMC. Nurses of this study reported that workload on staff prevents them from helping mothers to practice KMC. This study also found that mothers’ lack of knowledge on the technique and inadequate family support hinders its implementation. Charpak et al. [17] reported that the main reason for resistance to KMC is almost always due to local cultural factors; another reason is that the mother does not have enough privacy. In this study, absence of conducive environment or space, lack of privacy for the mother (absence of individual rooms), and local cultural factors are some of the factors hindering KMC implementation. The main reason for resistance to KMC implementation as found in this study is inadequate knowledge on KMC and its benefits. The absences of strong institutional policy, protocol or practice guidelines on KMC practice are challenges to KMC implementation. Other factors challenging KMC implementation as found in this study includes;
• Lack of follow up to ensure KMC practice at home after discharge.
• Babies under special therapies e.g. oxygen therapy and phototherapy.
• Mothers have low self-confidence because their babies are small.
• Multiple roles of mothers do not enhance continuous practice of KMC.
Various authors emphasized the need for staff education in promoting and facilitating KMC practice. [17-19] Nurses in this study suggested KMC should be part of nursing curricula and all healthcare providers should periodically be given in-service training on KMC especially newly appointed staff. Contrary to findings by Solomons and Rosant [20] stating that ANC nurses did not need KMC training, equipment and support because they were not directly involved in carrying out KMC, nurses in this study suggested that nurses at ANC be trained so they can educate expectant mothers on the technique. Nurses who work in the NICU particularly suggested that KMC rooms should be well equipped (with beds, reclining chairs, KMC materials etc) to make it comfortable for the mothers. This is confirmed by earlier findings by Solomons and Rosant [20] who reported that adequate resources such as beds, cupboards, and dining and leisure areas, should be available wherever KMC is implemented in order to accommodate the mothers and their infants, and to make their stay as pleasant as possible. Nurses in the current study suggest strong policies to support KMC implementation, a well-documented protocol on KMC practice and KMC nurses should be appointed and trained. Other suggestions are:
• Mothers should be educated on KMC practice and its benefits.
• Involve spouse and family members in KMC education.
• KMC should be part of NICU protocols/written practice guidelines.
• Follow ups after a preterm/LBW is discharged.
• NICU nurses suggested that KMC rooms should be made conducive for KMC practices i.e., provide reclining chairs and beds. Pattinson et al. [21] reported that successful KMC implementation requires commitment from site managers and their personnel, as well as from dedicated trained nursing staff. It also requires the provision of adequate space and other resources, including written protocols. [21]
Conclusion
Kangaroo mother care is a safe and effective tool that can be used to ensure the well-being of preterm/LBW as well as term infants. A good number of nurses in the Tamale metropolis have a positive attitude towards KMC but lack adequate knowledge on its benefits and how to ensure a successful implementation. There is therefore the need for creating training opportunities and regular in-service training should be conducted to enhance their knowledge.
Acknowledgements
The authors wish to thank all the participants of the study for their active participation and precious time. We are also grateful to the In-Charges of the four main Hospitals in Tamale Metropolis for their support during data collection and Dr. Terry Ansah for his assistance with the analysis of the data.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- World Health Organization (WHO). Kangaroo mother care: A practical guide. Geneva, Switzerland; 2003.
- Strand H. Knowledge of and attitudes to the practice of kangaroo mother care (KMC) among staff in two neonatal units; 2011.
- Liyanage G. Kangaroo mother care. Sri Lanka J Child Health. 2005; 34: 13-15.
- Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010; 88: 31-38.
- Mamaye Y. Factsheet for preterm birth in Ghana: World Prematurity Day; 2013.
- World Health Organization, March of Dimes, The Partnership for Maternal, Newborn & Child Health, Save the Children. The global action report on Preterm Birth; 2012.
- Charpak N, Ruiz-Pelaez JG, Zupan J, Cattaneo A, Figueroa Z, Tessier R, et al. KMC: 25 years after. Acta Paediatr. 2005; 94: 514-522.
- Conde-Agudelo A, Díaz-Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birth weight infants; 2014.
- Omer IM, Hassan HA. The prevalence and risk factors of retinopathy of prematurity among preterm babies admitted to Soba Neonatal Intensive Care Unit. Sud J Paediatr. 2014; 14: 17-21.
- George OB. Effect of ‘Kangaroo Mother Care’ training on knowledge, attitude and practice of health care providers in selected district hospitals in North Rift Region, Kenya; 2013.
- Adzitey PS, Adzitey F, Suuk L. Teenage pregnancy in the Builsa District: A focus study in Fumbisi. J Life Sci Biomed. 2013; 3(3): 185-188.
- Dalal A, Bala DV, Chauhan S. A cross-sectional study on knowledge and attitude regarding kangaroo mother care practice among health care providers in Ahmedabad district. Int J Med Sci Pub Health. 2014; 3: 253-256.
- Bergman N, Linley L, Fawcus S. Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for psychological stabilization in 1200- to 2199-gram newborns. Acta Paediatr. 2004; 93: 779-785.
- Udani RH, Nanavati RN. Training manual on kangaroo mother care. Published by the Department of Neonatology, KEM Hospital and Seth GS Medical College, Mumbai; 2004.
- Engler JA, Ludington-Hoe SM, Cusson RM, Adams R, Bahnsen M, Brumbaugh E, et al. Kangaroo care: national survey of practice, knowledge, barriers, and perceptions. J Maternal and Child Nur. 2002; 27: 146-153.
- Feldman R, Eidelman AI, Sirota L, Weller A. Comparison of skin-to-skin (Kangaroo) and traditional care: Parenting outcomes and preterm infant development. Paediatr. 2002; 110: 16-26.
- Charpak N, Ruiz-Pelaez JG. Resistance to Implementing Kangaroo mother care in developing countries, and proposed solutions. Acta Paediatr. 2006; 95: 529-534.
- Victor L, Persoon J. Implementation of Kangaroo Care: A parent-health care team approach to practice change. Cri Care Nur Clin North Am. 1994; 6: 891-895.
- Bell RP, McGrath JM. Implementing a Research-based Kangaroo Care Program in the NICU. Nur Clin North Am. 1996; 31: 387-403.
- Solomons N, Rosant C. Knowledge and attitudes of nursing staff and mothers towards kangaroo mother care in the eastern sub-district of Cape Town. South Afr J Clin Nut. 2012; 25: 33-39.
- Pattinson RC, Arsalo I, Bergh AM, Malan AF, Patrick M, Phillips N. Implementation of kangaroo mother care: A randomized controlled trial of two outreach strategies. Acta Paediatr. 2005; 94: 924-997.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.