Knowledge and Practice of Emergency Contraception Among Female Undergraduates in South Eastern Nigeria
- *Corresponding Author:
- Dr. Ifeanyichukwu U Ezebialu
Department of Obstetrics and Gynecology, Faculty of Clinical Sciences, Anambra State University Awka, Nigeria
E-mail: anyi_ezebialu@yahoo.com.
Abstract
Background: Unintended pregnancy remains a major challenge to the reproductive health of women especially in the developing countries. It is a major reason for unsafe abortion, a major contributor to maternal mortality. Aim: This study was designed to assess the knowledge and practice of emergency contraception among female non‑medical undergraduates. Subjects and Methods: In this cross sectional observational study, 675 female non medical undergraduates were interviewed using pretested semi structured questionnaire to assess their knowledge and experience with emergency contraception. Data was analysed using SPSS version 17 (SPSS, Chicago, IL, USA). Data were presented as percentages and tables. Associaton between variables was tested using the χ2 test. Results: Only 51.6% (348/675) of the respondents reported knowledge of emergency contraception. Being sexually active, use of regular family planning methods and having an extra risk for unintended pregnancy were factors that significantly influenced knowledge. Only 45.7% (159/348) knew the correct methods (Postinor‑2, combined oral contraceptive and intra uterine contraceptive device), 37.9% (132/348) practiced any method with about half of them using the correct methods. Conclusions: There is poor basic knowledge of emergency contraception among these female undergraduates in south eastern Nigeria. A sizeable number of them depend on unconventional methods for emergency contraception. We recommend the introduction of formal lessons on emergency contraception and other reproductive health issues into the Nigerian undergraduate curriculum.
Keywords
Africa, Emergency contraception, Female, Knowledge, Practice
Introduction
Unintended pregnancy is a major challenge to the reproductive health of young adults especially, in developing countries with roughly one in every five pregnancies in Nigeria being unplanned.[1,2] Recent reports even show it is increasing.[3] Many young women with unintended pregnancies resort to abortions which are mainly performed in unsafe conditions. Those who carry their pregnancies are likely to have increased risks of morbidity and mortality more than those for adult women.[4] In the developing world as a whole, an estimated five million women are admitted for treatment of complications from induced abortions each year, equating to an average rate of 5.7 per 1000 women per year in all developing regions.[5] With decreasing age of menarche and coitarche, recent findings suggest that young people engage early in unplanned and unprotected sexual intercourse, which in most cases will lead to unwanted pregnancy.[6] In Nigeria, it has been noted that unintended sexual intercourse is the leading cause of unintended pregnancy and induced abortions.[7]
The use of effective contraceptive methods has been shown to be beneficial in timing one’s pregnancy. Available reports show that many Nigerian women do not use any form of contraception for various reasons. About 32% of married women and 54% of unmarried sexually active women in Nigeria have an unmet need for contraception.[3] The contraceptive prevalence rate according to the National Demographic Health Survey of 2008 is 15% with the male condom being the most used method. The most commonly used method among currently married women is the injectable. This poor utilization of contraception may be due to poor contraceptive knowledge and cultural or religious beliefs. Unintended pregnancy arises when there is an unprotected sexual intercourse as occurs in cases of rape, condom accidents as well as contraceptive failure.
Emergency contraception is the use of a drug or device to prevent pregnancy after an unprotected sexual intercourse.[8] It is primarily a female method, so its use and success rests mainly on how women perceive and practice it. A variety of methods exists for emergency contraception but levonorgestrel-only pills (Postinor-2) and combined oral contraceptives appear to be the most common methods practiced in Nigeria since, they can be obtained over the counter from patent medicine and pharmacy shops. Unconventional techniques (some common drugs used for other health problems as well as some traditional or herbal preparations) of emergency contraception are also practiced. Up to 75% of sexually active (13-19) teenage girls have been reported to use some form of perceived contraceptive devices such as laxatives, local potash, “white quinine”, and mestrogen pills in the south-west geopolitical zone of the country.[9]
Large proportions of school girls are adolescents (aged between 10 years and 19 years) and are a vulnerable group for unwanted pregnancy. This is because of their poor knowledge and usage of routine contraception despite their regular sexual activity. Some of them may even engage in commercial sex to augment their finances.[10] They are also exposed to rape and other forms of sexual assault. In the developing countries, studies have evaluated the knowledge of emergency contraception among female undergraduates. In Port Harcourt, Nigeria, Akani, and co-workers assessed 600 non-medical students and reported that 50.7% of them were aware of emergency contraception.[6] In Benin City, Nigeria, a study of 880 female undergraduates revealed that 58% were aware of emergency contraception.[4] Similarly, in Lagos, former federal capital of Nigeria, 67.8% of 480 female university students had knowledge of emergency contraception.[11]
The figures are not too different in other parts of Africa. In Ghana, a survey of randomly selected 2292 undergraduates revealed that 51.4% had heard of emergency contraception.[12] Apart from general poor basic knowledge, detailed knowledge regarding the timing and dosage of the drugs was even poorer.[4,6,11,12] Even in more developed countries, the knowledge of emergency contraception among adolescents is also poor.[13] However, in America, college students at the University of Michigan had a very good knowledge of emergency contraception.[14] On the other hand, a survey of young women in United States showed that only 33% were aware of emergency contraception with less than one-tenth of them knowing the correct timing.[15]
Despite the increase in sexual activity among young adults, there is no formal means of sexual education for the adolescents except perhaps those in medical education. This, therefore, leaves this high risk group with insufficient and sometimes wrong knowledge of emergency contraception. This study was designed to assess the knowledge and practice of emergency contraception among female non-medical undergraduates.
Subjects and Methods
Between July 1st and August 20th, 2009, we conducted a cross-sectional observational study of 750 female non-medical students of Anambra State University. Anambra State University is located in South Eastern Nigeria and has three campuses each located at Uli, Igbariam and Awka. It has a total of 10 faculties, excluding the medical school. Respondents were obtained from non-medical students at Uli and Igbariam campuses using multistage sampling technique. Sampling frames comprising list of all the departments in each of the ten faculties at the Anambra State University were obtained and two departments were selected from each faculty by simple random sampling using computer generated random numbers. A total of ten departments were selected. A level or year of study was then selected from each department by simple random sampling. Each level selected was approached just before the start of a lecture and their consent was obtained after the nature of the study was explained to them. Those to participate in the study were then selected using systematic random sampling technique by selecting every third female student seated after randomly selecting a starting point.
The questionnaires were pretested among non-medical students of Nnamdi Azikiwe University who were not included in the main study. The questionnaire assessed information on the socio-demographic characteristics of the respondents, knowledge and use of emergency contraceptives. Sources of information were also assessed as well their potential risk for unintended pregnancy. Knowledge of correct indications for emergency contraception and their correct timing were also assessed. Informed consent was obtained from all respondents before being interviewed, and ethical approval was also obtained from the authorities.
Data were coded and analyzed using SPSS statistical package version 17 (SPSS, Chicago, IL, USA). The χ2 test was used for statistical analysis and P < 0.05 was considered significant (providing 95% confidence interval).
Results
Out of the 750 questionnaires distributed, 675 questionnaires were properly completed and available for analysis, giving a recovery rate of 90%.
The mean (SD) age of the respondents was 21.8 (2.9) years. The socio-demographic characteristics of the respondents are shown in Table 1.
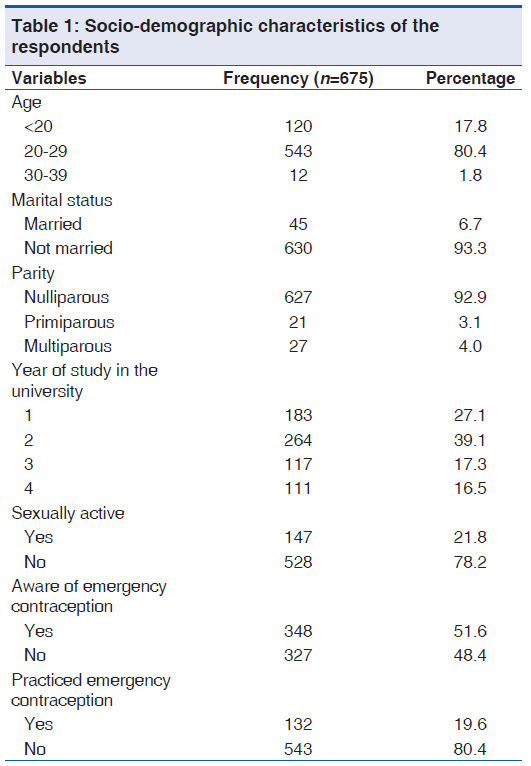
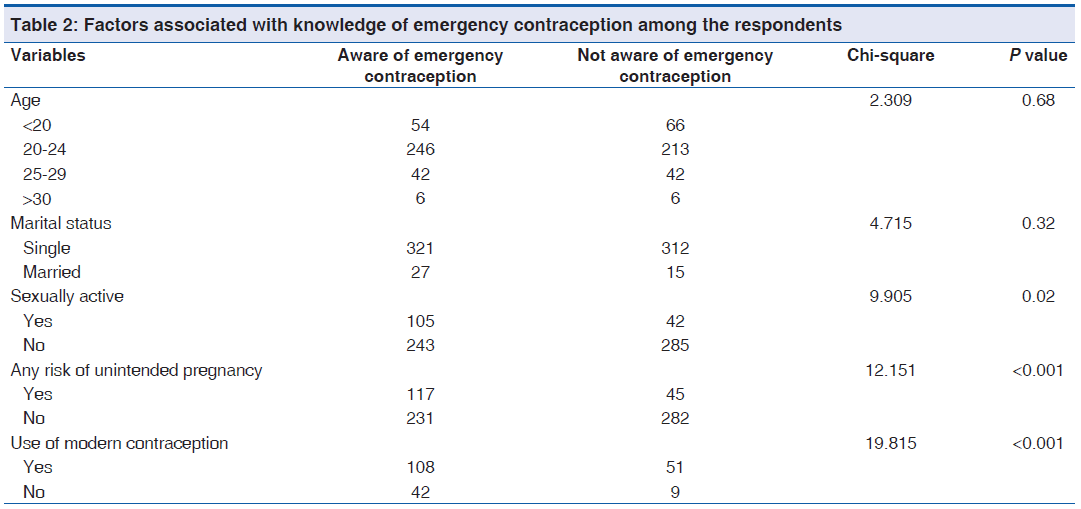
A little more than half of the respondents, 51.6% (348/675), reported that they have heard about emergency contraception. Factors significantly associated with knowledge of emergency contraception among the respondents were being sexually active (P = 0.02), use of conventional family planning methods (P < 0.001) and having an additional risk for unwanted pregnancy (P < 0.001) [Table 2].
Out of the 348 respondents who were aware of emergency contraception, 21.5% (75/348) got their information from a health care worker, 18.1% (63/348) from the media, 28.4% (99/348) from books, 11.2% (39/348) from their sexual partners and 51% (177/348) from their peers and friends. Table 3 displays the different methods the respondents considered to be emergency contraceptives.
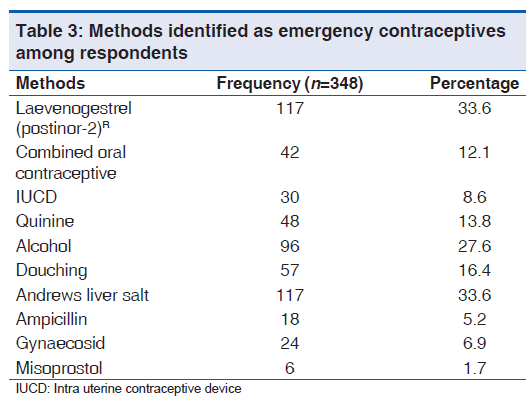
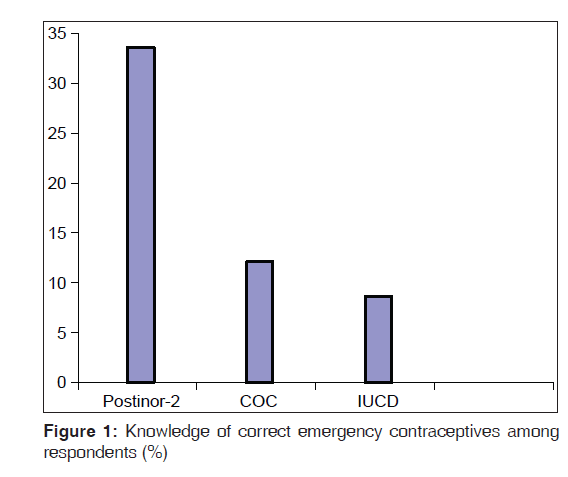
Only 45.7% (159/348) of the respondents reported knowledge of the correct methods of emergency contraception [Figure 1]. However, a large proportion of them (88.8%, 309/348) knew the correct indications for emergency contraception. More than half of the respondents who were aware of emergency contraception (59.5%, 207/348) felt that emergency contraception should be used routinely after every sexual intercourse as long as the woman does not want to be pregnant. Total respondents who were aware of emergency contraception, 41.4%, (144/348) reported that emergency contraceptives should be used within 24 h of exposure to unprotected sexual intercourse. The timing of emergency contraception as suggested by the respondents is represented in Table 4.
| Timing | Frequency | Percentage** |
|---|---|---|
| Within 24 h | 156 | 44.8 |
| Within 72 h | 33 | 9.5 |
| After a missed period | 24 | 6.9 |
| I do not know | 144 | 41.4 |
**The total is more than 100% because respondents were allowed to choose more than one
Table 4: Knowledge of timing of emergency contraception among the respondents
Concerning practice, 37.9% (132/348) of the respondents reported that they had ever practiced emergency contraception. However, only about half of them, 52.3% (69/132) used the correct methods. Factors significantly, associate with use of emergency contraception are use of regular contraceptives (P < 0.001), being sexually active (P < 0.001) and having a risk of unintended pregnancy (P < 0.001). Religion was not significantly associated with use of emergency contraception among the respondents (P = 0.63).
Discussion
More than 80% of the respondents were aged 20-29 years, which adequately represents the study population. In the present study, awareness of emergency contraception appears below average as only 51.6% of the respondents were aware of emergency contraception. This figure is lower than that obtained from a similar population in Lagos, South-Western Nigeria and Enugu, South-Eastern Nigeria.[11,16] Significant factors that influenced their knowledge were being sexually active and use of regular contraceptives. Similar factors were also identified by Aziken and his group in Benin City, Nigeria.[4] This finding is interesting because it does appear that women would not know about such contraceptive measure until they are exposed to the risk of unintended pregnancy.
This study has identified peers and friends as the commonest source of information on emergency contraception. These women do not have any formal means of learning about such reproductive health matters as they are not in the medical school. Therefore, they rely mainly on information they get from friends who do not have medical knowledge and so are likely to be wrong most times. This may also explain the fact that a sizeable proportion of those who reported knowledge of emergency contraception did not know the correct methods. This poor knowledge of correct methods has also been demonstrated in other studies.[4,6,17] This has far reaching implications as women who genuinely desire to use emergency contraceptives may end up using non-conventional methods and subsequently face the risk of unintended pregnancy and unsafe abortion. The most commonly known correct method of emergency contraception in this study was Postinor-2. This method appears to be the most commonly available in Nigeria and can be obtained over the counter. A study conducted in the United Kingdom showed that medically related students were significantly more knowledgeable on emergency contraception than their non-medical counterparts.[18] This may be a pointer to the fact that formal lessons are needed to improve knowledge of this matter among women. Apart from the poor basic knowledge of emergency contraception, knowledge of correct methods and timing of the agents was also poor. This may be a reflection of inadequate information. The fact that only about 50% of those who reported knowledge of emergency contraception knew the conventional method has a great impact in the practice. Similar to findings by Aziken in Benin,[4] majority of the respondents (41.4%) agreed that emergency contraceptives should be used within 24 h while only 1.7% knew that intra uterine contraceptive device can be used even within 7 days. It is true that the agents will be effective when used within 24 h of unprotected sexual intercourse but such response needs to be carefully interpreted. Such information may prevent someone who could still prevent a pregnancy from taking emergency contraceptives because she thought she had missed the period of effectiveness. The practice of emergency contraception was also low as only 37.9% (n = 132) had practiced one form or the other. More worrisome however, is the fact that only half of this number used a conventional method.
The major limitation of this study was that it depended on self-report by the respondents. Although, the respondents were asked not to exchange ideas when they were answering the questions, strict compliance to this instruction will be difficult to guarantee. However, the questions were pre-tested to be sure there were no ambiguities.
Conclusion
There is a poor basic knowledge of emergency contraception among these female non-medical undergraduates in South Eastern Nigeria. A sizeable number of them depend on unconventional methods for emergency contraception. We recommend the introduction of formal lessons on emergency contraception and other reproductive health issues will enhance knowledge and practice. Future research should focus on identifying effective methods of disseminating information to improve knowledge among women.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Bankole A, Oye-Adenira BA, Singh S, Adewole IF, Wulf D, Sedgh G, Hussain R. The Alan Guttmacher Institute. Facts on unwanted pregnancy and induced abortion in Nigeria. New York: Allan Guttmacher Institute; In Brief 2006. p. 1-2.
- Sudhinaraset M. Reducing unsafe abortion in Nigeria. In Brief, New York: Guttmacher Institute; 2008. p. 1-3.
- Hussain R, Bankole A, Singh S, Wulf D. Reducing unintended pregnancy in Nigeria. New York: The Alan Guttmacher Institute; Research in Brief 2005 series, No. 4. p. 1-8.
- Aziken ME, Okonta PI, Ande AB. Knowledge and perception of emergency contraception among female Nigerian undergraduates. Int Fam Plan Perspect 2003;29:84-7.
- Singh S. Hospital admissions resulting from unsafe abortion: Estimates from 13 developing countries. Lancet 2006;368:1887-92.
- Akani C, Enyindah C, Babatunde S. Emergency contraception: Knowledge and perception of female undergraduates in the Niger delta of Nigeria. Ghana Med J 2008;42:68-70.
- Society for Family Health. Emergency contraception in Nigeria. Report of an Exploratory Research Project Lagos. Soc Fam Health 1998: 1-2.
- Glasier A. Emergency postcoital contraception. N Engl J Med 1997;337:1058-64.
- Haspels AA. Emergency contraception: A review. Contraception 1994;50:101-8.
- Ilika A, Igwegbe A. Unintended pregnancy among unmarried adolescents and young women in Anambra State, south east Nigeria. Afr J Reprod Health 2004;8:92-102.
- Ebuehi OM, Ekanem EE, Ebuehi OA. Knowledge and practice of emergency contraception among female undergraduates in the University of Lagos, Nigeria. East Afr Med J 2006;83:90-5.
- Addo VN, Tagoe-Darko ED. Knowledge, practices, and attitudes regarding emergency contraception among students at a university in Ghana. Int J Gynaecol Obstet 2009;105:206-9.
- Calabretto H. Emergency contraception-knowledge and attitudes in a group of Australian university students. Aust N Z J Public Health 2009;33:234-9.
- Vahratian A, Patel DA, Wolff K, Xu X. College students’ perceptions of emergency contraception provision. J Womens Health (Larchmt) 2008;17:103-11.
- Foster DG, Ralph LJ, Arons A, Brindis CD, Harper CC. Trends in knowledge of emergency contraception among women in California, 1999-2004. Womens Health Issues 2007;17:22-8.
- Ikeme AC, Ezegwui HU, Uzodimma AC. Knowledge, attitude and use of emergency contraception among female undergraduates in Eastern Nigeria. J Obstet Gynaecol 2005;25:491-3.
- Abasiattai AM, Umoiyoho AJ, Bassey EA, Etuk SJ, Udoma EJ. Misconception of emergency contraception among tertiary school students in Akwa Ibom State, South-south, Nigeria. Niger J Clin Pract 2007;10:30-4.
- Khalid AK, Abd Halim H, Kenny L. Usage of emergency contraception between medical related and non-medical related students. Ir Med J 2009;102:104-8.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.