Knowledge, Attitude, and Practice of Undergraduate Senior Dental Students and General Dental Practitioners toward Resin Bonded Bridges in the Asir Region, Saudi Arabia
Department of Prosthetic Dental Science, College of Dentistry, Abha, Saudi Arabia
- *Corresponding Author:
- Mohammad A Zarbah
Department of Prosthetic Dental Science
College of Dentistry
Abha, Saudi Arabia
Tel: 918067549920
E-mail: zrbah@kku.edu.sa
Citation: Zarbah MA. Knowledge, Attitude, and Practice of Undergraduate Senior Dental Students and General Dental Practitioners toward Resin Bonded Bridges in the Asir Region, Saudi Arabia. Ann Med Health Sci Res. 2020;10: 889-894.
This is an open access article distributed under the terms of the Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Resin bonded bridges (RBBs) are cost-effective, simple to use, and minimally-invasive compared to other fixed options for the replacement a short span or single tooth. Objective: The aim of this study was to assess the knowledge, attitude, and practice of undergraduate senior dental students (USDSs) and general dental practitioners (GDPs) toward resin bonded bridges in the Asir region of Saudi Arabia. Methods: In this cross-sectional study, a questionnaire was used to assess the knowledge and practice of RBBs. The attitudes of the participants toward continuous education were evaluated. Chi-square and Fisher’s exact tests were used to compare the responses of the two groups of participants. Results: The overall response rate was 78.9% (300/380). Less than half of the participants in both groups considered RBB as a successful conservative approach for restoring missing teeth. More than 50% of both the USDSs and GDPs selected fixed–fixed as the most successful RBB design. Only half of the participants demonstrated confidence in offering RBBs to their patients due to lack of education and training regarding the use of RBBs. About 50% of the GDPs and 25% of the USDSs were exposed to the process of replacing missing teeth using RBBs during their clinical undergraduate studies. Conclusion: The lack of skill and training on the use of RBBs was consistent in both groups. Improvements in the undergraduate dental curriculum and clinical skills of the students and continuing education opportunities for the GDPs are required to increase their exposure to RBBs.
Keywords
Knowledge; Attitude; Clinical application; Resin bonded bridges
Introduction
Resin bonded bridges (RBBs) are minimally-invasive and costeffective fixed prosthetic tooth replacement options compared to the conventional bridgework. They were initially used by Rochette for periodontal splinting in the 1970s; subsequently, Howe and Denehy used them as perforated cast retainers to temporarily replace missing teeth. [1] Even though the initial RBBs demonstrated poor longevity, recent scientific evidence indicates that they have achieved predictable long term success and patient satisfaction. [2,3]
In spite of issues such as debonding, a systematic review conducted by Balasubramaniam revealed that the predicted 5- and 10-year survival rates of RBBs are 83.6% and 64.9%, respectively. [4] In another systematic review on the survival and complication rates of RBBs over a 5-year period, an estimated survival rate of 87.7% was reported. [5]
RBBs are cost-effective, simple to use, and minimally-invasive with reduced biological consequences when compared to other fixed options for replacing a short span or single tooth. [6] They play an important role in restorative dentistry, with their indications extending beyond the temporary replacement of teeth; they can be used as both an interim or definitive tooth replacement option. Careful patient selection, appropriate treatment planning, and consideration of all the major factors such as framework design, maximum enamel coverage by retainers, use of sandblasted and non-perforated retainers, and minimal (or no) tooth preparation with the preservation of the enamel thickness-will aid in the development of successful treatment options with longer survival rates. [6] In addition, proper occlusal management, a minimum retainer thickness of 0.7 mm, and a minimum connector height of 2 mm have been reported as essential factors to minimize complications such as debonding, which is one of the most common concerns of RBBs. [4,7]
The prevalence of dental caries and missing teeth are 72.9% and 5.9%, respectively, in the Asir region, Saudi Arabia; [8] RBBs could be used as a valid conservative tooth replacement option in these cases. The exposure of students at dental schools to RBBs could have a significant impact on the selection of this treatment when discussing tooth replacement options with patients. The aim of the present study was to evaluate the knowledge, attitude, and practice of undergraduate senior dental students (USDSs) and general dental practitioners (GDPs) towards resin bonded bridges in the Asir region, Saudi Arabia.
Methods and Materials
This cross-sectional study comprised USDSs and GDPs from the Asir region in Saudi Arabia. The USDSs and GDPs were considered as two distinct strata when stratified random sampling was performed. The study was conducted in compliance with the protocol; ethical approval was obtained from the ethical committee at King Khalid University, College of Dentistry (Approval No. SRC/ETH 2017-18/069). Informed consent was obtained from the subjects participating in the study. The participation was on a voluntary basis and no incentives were provided to the participants. Data protection and anonymity were guaranteed.
An online well-structured questionnaire containing three parts was attached to the study description along with the consent form for participation and sent as an electronic link to 380 participants via different WhatsApp groups. The first part of the questionnaire contained questions related to gender, age, and number of years of experience, percentage of RBBs performed in the clinical practice, and the attitude and knowledge about RBBs as a treatment option. The second part of the questionnaire involved questions related to the success factors of RBBs, such as the tooth surface, area of the mouth where the RBB is placed, bridge design, retainer fitting surface treatment, retainer thickness, connector height, retentive features, type of cement, and tooth isolation. The third segment of the form included general questions that were designed to analyze the impact of teaching and providing practical experience to students in dental schools. The knowledge of the participants with regard to the survival and complications of RBBs, and their attitude toward continuous education as an important tool for the utilization of this type of conservative treatment were assessed.
All the returned forms were analyzed by a single operator. Data were analyzed using the Statistical Package for Social Sciences (SPSS) program (version 25; Chicago, Illinois, USA). The Chi‐square and Fisher’s exact tests were used to compare the responses of the participants. A p-value <0.05 was considered statistically significant.
Results
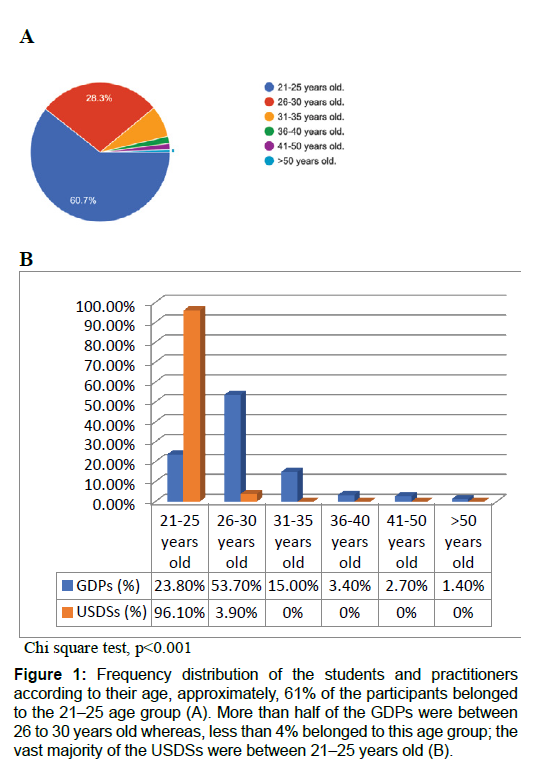
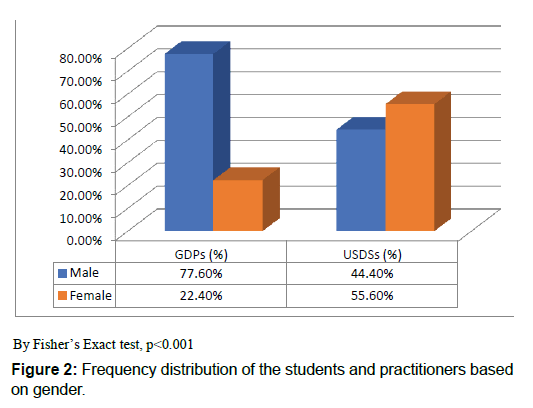
On the basis of the returned questionnaires, the overall response rate was 78.9% (300/380); the response rate for the USDSs was 80.5% (153/190) and for the GDPs was 77.4% (147/190). The responses were divided almost equally between the two groups of participants. Furthermore, 60.7 % of the participants belonged to the 21–25 age group, 28.3% belonged to the 26- 30 age group, and the remaining 11% were >30 years of age [Figure 1A]. As seen in Figure 1B, more than half of the GDPs were between 26 to 30 years old whereas, among the USDSs, less than 4% belonged to this age group; the vast majority of the USDSs were between 21–25 years old. More than 60% of the participants were males-almost two-thirds of them were GDPs-and the remaining (39.3%) were females [Figure 2].
Figure 1: Frequency distribution of the students and practitioners according to their age, approximately, 61% of the participants belonged to the 21-25 age group (A). More than half of the GDPs were between 26 to 30 years old whereas, less than 4% belonged to this age group; the vast majority of the USDSs were between 21-25 years old (B).
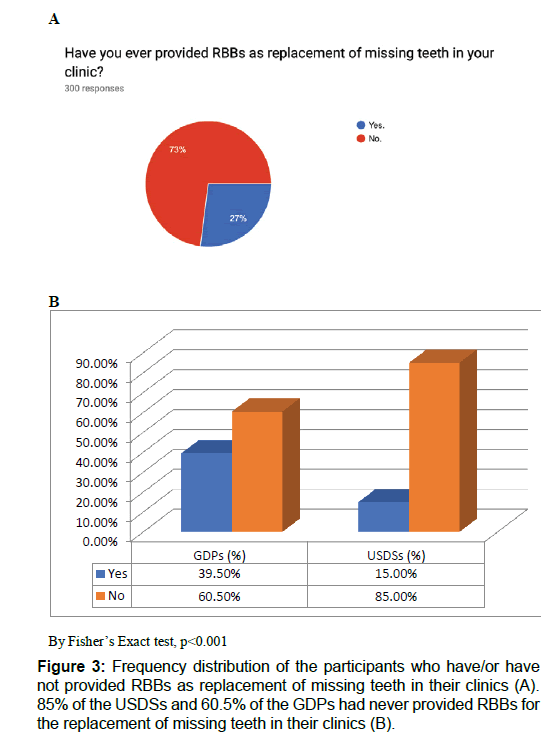
As seen in Table 1, almost half of the GDPs (48.3%) had practiced dentistry for less than five years, whereas the proportion of dentists with more than 15 years of experience was 4.8% (p<0.001; Table 1). Furthermore, 73% of the participants [Figure 3A] - 85% of the USDSs and 60.5% of the GDPs [Figure 3B]—had never provided RBBs for the replacement of missing teeth in their clinics. The anterior maxilla was considered the most favorable location for achieving a successful RBB (USDSs, 57.8%; GDPs, 69.3%).
| Question No. | Questions | Answers | GDPs (%) | USDSs (%) | p-Value |
|---|---|---|---|---|---|
| 1 | How long have you been practicing dentistry? | Nil | 0 (0) | 153 (100.0) | 0.000** |
| <5 years | 71 (48.3) | 0 (0) | |||
| 6?10 years | 58 (39.5) | 0 (0) | |||
| 11?15 years | 11 (7.5) | 0 (0) | |||
| >15 years | 7 (4.8) | 0 (0) | |||
| 2 | Have you ever provided RBBs as replacement of missing teeth in your clinic? | Yes | 58 (39.5) | 23 (15.0) | 0.000* |
| No | 89 (60.5) | 130 (85.0) | |||
| 3 | In what percentage of tooth replacement cases have you used RBBs? | Nil | 89 (60.5) | 130 (85.0) | 0.000** |
| <5% | 18 (12.2) | 10 (6.5) | |||
| 5?25%. | 20 (13.6) | 3 (2.0) | |||
| 25?50%. | 13 (8.8) | 5 (3.3) | |||
| 50?75%. | 6 (4.1) | 5 (3.3) | |||
| >75%. | 1 (0.7) | 0 (0) | |||
| 4 | What type of restoration do you think RBBs provide? | Permanent | 42 (28.6) | 56 (36.6) | 0.287 |
| Temporary | 33 (22.4) | 34 (22.2) | |||
| Both | 72 (49.0) | 63 (41.2) | |||
| 5 | In which areas of the mouth are RBBs the most successful? | Anterior maxillary teeth | 85 (57.8) | 106 (69.3) | 0.082 |
| Posterior maxillary teeth | 13 (8.8) | 16 (10.5) | |||
| Anterior mandibular teeth | 26 (17.7) | 15 (9.8) | |||
| Posterior mandibular teeth | 23 (15.6) | 16 (10.5) | |||
| 6 | Which RBB design provides maximum longevity? | Fixed-fixed | 93 (63.3) | 83 (54.2) | 0.249 |
| Cantilever | 26 (17.7) | 37 (24.2) | |||
| No significant difference | 28 (19.0) | 33 (21.6) | |||
| 7 | Does the amount of enamel structure play an important role in the success of RBBs? | Yes | 99 (67.3) | 119 (77.8) | 0.052 |
| No | 48 (32.7) | 34 (22.2) | |||
| 8 | Does preparing teeth for retentive features improve longevity? | Yes | 94 (63.9) | 105 (68.6) | 0.396 |
| No | 53 (36.1) | 48 (31.4) | |||
| 9 | Does tooth isolation enhance the bonding? | Yes | 109 (74.1) | 121 (79.1) | 0.341 |
| No | 38 (25.9) | 32 (20.9) | |||
| 10 | Does retainer fitting surface treatment enhance RBB bonding? | Yes | 89 (60.5) | 109 (71.2) | 0.052 |
| No | 58 (39.5) | 44 (28.8) | |||
| 11 | What is the minimum thickness of the RBB retainer? | 0.5 mm | 55 (37.4) | 52 (34.0) | 0.806 |
| 0.7 mm | 37 (25.2) | 45 (29.4) | |||
| 1 mm | 37 (25.2) | 40 (26.1) | |||
| 1.2 mm | 18 (12.2) | 16 (10.5) | |||
| 12 | What is the minimum height for RBB connector? | 1 mm | 56 (38.1) | 59 (38.6) | 0.500 |
| 2 mm | 64 (43.5) | 57 (37.3) | |||
| 3 mm | 21 (14.3) | 26 (17.0) | |||
| 4 mm | 6 (4.1) | 11 (7.2) | |||
| 13 | What is the best cement type to be used? | Resin cement | 73 (49.7) | 72 (47.1) | 0.327 |
| Glass ionomer cement | 41 (27.9) | 48 (31.4) | |||
| Zinc oxide eugenol cement | 22 (15.0) | 15 (9.8) | |||
| Does not affect | 11 (7.5) | 18 (11.8) | |||
| 14 | What is the survival rate of RBBs in 5 years? | <50% | 55 (37.4) | 53 (34.6) | 0.524 |
| 51?80% | 58 (39.5) | 70 (45.8) | |||
| >80% | 34 (23.1) | 30 (19.6) | |||
| 15 | What is the most common complication reported in the literature? | Biological complications such as caries and endodontic and periodontal diseases related to the abutment teeth. | 52 (35.4) | 69 (45.1) | 0.229 |
| Mechanical complications such as ceramic fracture and chipping | 41 (27.9) | 36 (23.5) | |||
| De-bonding of the retainer | 54 (36.7) | 48 (31.4) | |||
| 16 | Are you confident to offer RBBs to your patient when they are indicated? | Yes | 76 (51.7) | 81 (52.9) | 0.908 |
| No | 71 (48.3) | 72 (47.1) | |||
| 17 | If (No), why? | No enough education and training | 37 (52.1) | 41 (56.9) | |
| Technique-sensitive procedure | 17 (23.9) | 21 (29.2) | |||
| RBB is only short-term replacement | 9 (12.7) | 6 (8.3) | |||
| Patient may not like it | 7 (9.9) | 4 (5.6) | |||
| Others | 1 (1.4) | 0 (0) | |||
| 18 | Do you usually consider RBBs as one of your treatment options to replace single missing tooth? | Yes | 62 (42.2) | 56 (36.6) | 0.346 |
| No | 85 (57.8) | 97 (63.4) | |||
| 19 | Are you convinced that RBBs could be the first line of permanent treatment in some selected cases? | Yes | 73 (49.7) | 77 (50.3) | 1.000 |
| No | 74 (50.3) | 76 (49.7) | |||
| 20 | Do you consider RBB as a successful conservative approach for restoring missing teeth? | Yes | 63 (42.9) | 71 (46.4) | 0.023** |
| No | 31 (21.1) | 15 (9.8) | |||
| Not sure | 53 (36.1) | 67 (43.8) | |||
| 21 | Do you think RBB is cost-effective? | Yes | 52 (35.4) | 37 (24.2) | 0.049** |
| No | 39 (26.5) | 38 (24.8) | |||
| Not sure | 52 (38.1) | 37 (51.0) | |||
| 22 | Have you ever been involved in or observed any clinical procedure involving RBBs? | Yes | 59 (40.1) | 30 (19.6) | 0.000* |
| No | 88 (59.9) | 123 (80.4) | |||
| 23 | In the preclinical sessions during undergraduate studying, had you ever been exposed to the process of replacing missing teeth with RBBs? | Yes | 65 (44.2) | 52 (34.0) | 0.076 |
| No | 82 (55.8) | 101 (66.0) | |||
| 24 | In the clinical sessions during undergraduate study, have you ever been exposed to the process of replacing missing teeth with RBBs? | Yes | 72 (49.0) | 40 (26.1) | .000* |
| No | 75 (51.0) | 113 (73.9) | |||
| 25 | Do you think that you have not been given enough education/practicing of RBBs during undergraduate studying? | Yes | 96 (65.3) | 114 (74.5) | 0.101 |
| No | 51 (34.7) | 39 (25.5) | |||
| 26 | If you hear about a lecture/ workshop regarding RBBs to be organized, would you be willing to attend? | Yes | 80 (54.4) | 73 (47.7) | 0.473 |
| No | 23 (15.6) | 30 (19.6) | |||
| Not sure | 44 (29.9) | 50 (32.7) |
*, P<0.05 (Fisher’s Exact Test). **, P<0.05 (Chi-Square Test).
Table 1: Frequency distribution of respondents according to their responses to the questionnaire.
With regard to the design and mechanical factors associated with RBBs, more than 50% of both the USDSs and GDPs selected fixed–fixed as the most successful RBB design. More than two-thirds of the participants in both groups believed that the amount of enamel structure play an important role in the success of RBBs. Furthermore, approximately 64% of GDPs and 69% of USDSs were of the opinion that preparing the tooth for the retentive features improves the longevity of the RBB treatment. According to three-fourth of the participants in both groups, tooth isolation does enhance the bonding of the RBB [Table 1]. About 60% of the GDPs and 71% of the USDSs agreed that retainer surface treatment improves the longevity of the treatment. About one-third of the participants in both groups selected 0.5 mm as the minimum thickness of the RBB retainer. The percentages of GDPs and USDSs who selected 1 mm and 2 mm as the minimum heights required for the RBB connector almost similar. Nearly half of the participants thought that resin cements were the most appropriate for use with RBBs. The survival rate of RBBs in 5 years was considered to be <50% by nearly one-third of the participants and between 51–80% by a little more than one-third of the participants.
Only half of the participants demonstrated confidence in offering RBBs to their patients when required. The main reason for the lack of confidence was the lack of education and training regarding the use of RBBs [Table 1]. With regard to the attitude of the participants, about half of them were convinced that RBBs could be the first line of permanent treatment in some selected cases, while the remaining half held the opposite opinion. Furthermore, nearly 43% of the GDPs considered RBB as a successful conservative approach for restoring missing teeth compared to 21% who did not, while the remaining 36% were not sure; the approximate values among the USDSs were 46%, 10%, and 44%, respectively (p<0.05). Only 35% of the GDPs and 24% of the USDSs thought that RBBs were costeffective; the remaining participants were either not sure or of the opinion that this treatment is not cost-effective. About 60% of the GDPs and 80% of the USDSs had been involved in or observed a clinical procedure involving RBBs (p<0.001). Furthermore, a vast majority of the USDSs had not been exposed to this procedure during their preclinical and clinical studies at the university. Approximately 50% of the participants in both groups demonstrated an interest in attending a lecture or workshop on RBB use.
Discussion
In this study, we evaluated and compared the knowledge, attitude, and perception of GDPs and USDSs toward RBBs. The overall response rate was 78.9% (80.5% among the USDSs and 77.4% among the GDPs). This was similar to that reported by Vohra and Qahtani, [9] but lower than that reported in another study. [10]
Some of the advantages of using RBBs include tooth preservation, treatment reversibility, good success rates, reduced costs, preservation of the pulp, and insignificant soft tissue interaction. [11,12] The awareness of the use of RBBs as a definitive treatment option has increased over the years. However, in this study, more than 80% of the USDSs had not used RBBs for tooth replacement; the corresponding number among the GDPs was 60%. Interestingly, more than 20% of the GDPs did not consider RBB as a successful option for tooth replacement when compared to about 10% in the USDS group, which may have contributed to the significant difference with regard to this question (p<0.05). Adequate knowledge about the factors that affect the performance of RBBs is key to its successful application.
Similar to the results of a previous study in Saudi Arabia, more than half of the participants in both groups were of the opinion that the anterior maxillary teeth were most successfully treated by RBBs and that the fixed-fixed design provides maximum longevity. [9]. As explained in a recent review, [4] the survival rates of RBBs for anterior teeth are higher than those for the posterior teeth. Alternatively, with regard to the design of the RBBs, the cantilever design has been shown to be associated with better survival rates compared to the fixed-fixed design. [13,14] Furthermore, a minimum retainer thickness of 0.7 mm and a minimum connector height of 2 mm have been recommended in previous studies. [15] However, about one-third of the participants in both groups selected a thickness of 0.5 mm and a connector height of 1 mm in this study. About 67% of the GDPs and 78% of the USDSs believed that adequate enamel structure was required for the success of the RBB. Studies have shown that resin cements are the most common type of cements used for RBBs; [4,12,15] however, in the present study, less than 50% of the participants in both groups selected this as the best option.
Debonding is one of the most common concerns of RBBs and could adversely affect the reliability of this treatment. [5] The isolation of the tooth along with enhancements for retention can increase the longevity of RBBs. [16] About 26% of the GDPs and 21% of the USDSs were of the opinion that tooth isolation did not enhance the bonding of RBBs. Furthermore, nearly 40% of the GDPs and 30% of the USDSs did not think that treatment of the retainer surface could enhance its bonding. Surface treatment of retainers has been shown to improve the success rates of the RBBs. [4] Several studies have shown that tooth preparation can enhance the resistance of RBBs. [14,17] In the present study, more than 30% of the participants in both groups did not believe that preparing the tooth for retentive features can improve the longevity of the treatment. These findings indicate the low levels of knowledge and the lack of skills and training among both the USDSs and GDPs in this study.
About 50% of the GDPs and USDSs were not confident about providing RBBs to the patients; lack of education and training were cited as the main reasons by the participants. Less than half of the participants in both groups considered RBB as a successful conservative approach for the restoration of missing teeth. RBBs are not widely used in clinical practice due to concerns regarding the reliability of this treatment. Identification of the reasons for the lack of use of RBBs and taking appropriate measures to address these concerns may increase their use in the clinics.
Approximately 40% of the GDPs had been involved in the provision of RBBs to the patients, whereas in the case of the USDSs, less than 20% of them had been involved in or observed any clinical procedure involving RBBs. About 44% of the GDPs and 34% of the USDSs had been exposed to the process of replacing missing teeth using RBBs during their pre-clinical undergraduate studies. Similarly, about 50% of the GDPs were exposed to the process of replacing missing teeth using RBBs during their clinical undergraduate studies; on the other hand, only about one-fourth of the USDSs had been exposed to the procedure. This indicates the lack of awareness and knowledge among the undergraduate students. However, the majority of the participants in both groups believed that they need to be provided with more information about RBBs during their undergraduate studies. The importance of continuing dental education in providing dentists with knowledge about new dental technologies, particularly resin-bonded prosthesis, has been emphasized in a recent study. [18]
Conclusion
In general, the knowledge, attitudes, and practices with regard to RBBs appeared to be similar between the GDPs and the USDSs in this study. Based on our findings, there is a need to improve the knowledge and attitude toward RBB use for the replacement of missing teeth. This may be achieved by improving the undergraduate dental curriculum and the clinical skills of the students. Furthermore, the use of continuing education programs for practicing dentists can improve the outcomes of treatment provided in dental clinics.
Competing Interests
The authors declare that they have no competing interests.
References
- Howe DF, Denehy GE. Anterior fixed partial dentures utilizing the acid-etch technique and a cast metal framework. J Prosthet Dent. 1977;37:28-31.
- Creugers NHJ, De Kanter RJAM. Patients’ satisfaction in two long-term clinical studies on resin-bonded bridges. J Oral Rehabil. 2000;27:602-607.
- Ketabi AR, Kaus T, Herdach F, Groten M, Axmann-Krcmar D, Pröbster L, et al. Thirteen-year follow-up study of resin-bonded fixed partial dentures. Quintessence Int. 2004;35:407-410.
- Balasubramaniam GR. Predictability of resin bonded bridges-A systematic review. Br. Dent. J.2017; 222:849.
- Pjetursson BE, Tan WC, Tan K, Brägger U, Zwahlen M, Lang NP. A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin Oral Implants Res. 2008;19:131-141.
- Gulati JS, Tabiat-Pour S, Watkins S, Banerjee A. Resin-bonded bridges - The problem or the solution? Part 1: Assessment and design. Dent. Update 2016;43:506-521.
- Nair A, Regish KM, Patil NP, Prithviraj DR. Evaluation of the effects of different groove length and thickness of the retainers on the retention of maxillary anterior base metal resin bonded retainers - An in vitro study. J Clin Exp Dent. 2012;4:91-96.
- Alshahrani I, Tikare S, Meer Z, Mustafa A, Abdulwahab M, Sadatullah S. Prevalence of dental caries among male students aged 15–17 years in southern Asir, Saudi Arabia. Saudi Dent. J. 2018;1;30:214-218.
- Vohra FA, Al-Qahtani MA. Attitude and awareness of dentist towards resin bonded bridges in Saudi Arabia. Saudi Dent J. 2014;26:96-102.
- AI-Hamzi MA, Madfa AA, Al-Sanabani FA, Al-Anesi Waled. EC Dental science research article knowledge of Yemeni dental practitioners towards resin bonded prosthesis. EC Dent. Sci. 2017;2:46-52.
- Ramteke S, Sathe S, Godbole SR, Rawat A. Resin bonded bridges: from crust to the core–a review article. International Journal of Contemporary Medical Research. 2016;3:503-506.
- Durey KA, Nixon PJ, Robinson S, Chan MFWY. Resin bonded bridges: Techniques for success. Br Dent J. 2011;211:113-118.
- Kern M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J Dent. 2017;56:133-135.
- Botelho MG, Chan AWK, Leung NCH, Lam WYH. Long-term evaluation of cantilevered versus fixed–fixed resin-bonded fixed partial dentures for missing maxillary incisors. J Dent. 2016;45:59-66.
- Vohra F, Baloch HR. Article • January 2013. 2014;22:147-53.
- Audenino G, Giannella G, Morello GM, Ceccarelli M, Carossa S, Bassi F. Resin-bonded fixed partial dentures: Ten-year follow-up. J Prosthet Dent. 2006;96:223.
- Miettinen M, Millar BJ. A review of the success and failure characteristics of resin-bonded bridges. Br Dent J. 2013;215.
- Landesman HM, Zimmerman JL, Bilan JP, Clark MA. How dentists learned about resin-bonded prostheses. J Prosthet Dent. 1986;56:493-497.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.