Large Vesico‑Vaginal Fistula Caused by a Foreign Body
Citation: Massinde AN, Kihunrwa A. Large vesico-vaginal fistula caused by a foreign body. Ann Med Health Sci Res 2013;3:456-7.
Abstract
Foreign body is a rare cause of vesico‑vaginal fistula most often reported in developed countries. In developing countries obstructed labor is the commonest cause of fistula. A nulliparous 19‑year‑old female presented with a 3‑week history of a foreign body in the vagina causing urinary incontinence and offensive vaginal discharge. Her guardian allegedly inserted the foreign body after she refused a pre‑arranged marriage. A plastic container was removed from the vagina under general anesthesia. A large vesico‑vaginal fistula was discovered, which was successfully surgically repaired. We recommend urgent removal of the foreign body, preferably under general anesthesia. However, if the history or physical examination reveals prolonged exposure, repair of the fistula should be delayed to allow for adequate debridement in order to prevent any life‑threatening complications.
Keywords
Developing countries, Fistula, Foreign body, Vagina
Introduction
Vesico‑vaginal fistula is commonly caused by obstructed labor, gynecological surgery, occasionally due to malignancy and rarely foreign body; in most cases being ring pessaries.[1] Cases of a foreign body in the vagina have been reported mostly in developed countries.[1‑4] Foreign body within the vagina can result in major complications if left unmanaged for a long period of time.[5,6] We present a case of forcefully inserted foreign body within the vagina that resulted in extensive vesico‑vaginal fistula.
Case Report
A nulliparous 19‑year‑old female presented with a 3 week history of a foreign body in the vagina. Her uncle allegedly forcefully inserted the foreign body after she refused a pre‑arranged marriage. The presence of this foreign body was associated with purulent and offensive vaginal discharge, dysuria and leakage of urine from the vagina.
On examination she was afebrile with stable vital signs. The patient was found to have suprapubic tenderness on palpation.
Examination of the genitalia could not be performed due to severe pain.
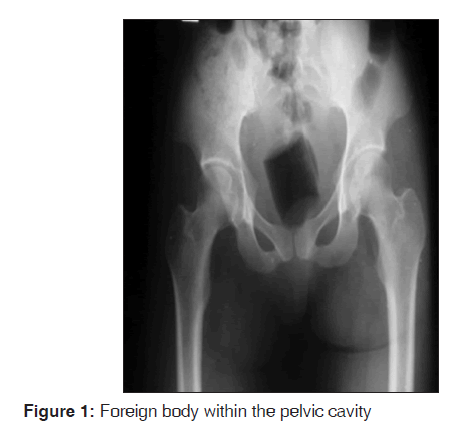
A plain pelvic radiograph showed an opacified object within the pelvic cavity [Figure 1].
The clinical radiographic impression was a foreign body in the vagina with associated bladder injury.
The patient was examined in theatre under general anaesthesia. The findings were perineal excoriation and clearly identifiable leakage of urine from the vagina. A plastic container approximately 4 cm in diameter was found invading into the vaginal musculature. With the successful removal of the container, a mid‑sized vesico‑vaginal fistula was noted measuring 2 cm in diameter with significant surrounding fibrosis and debris. A small stone was visualized in the bladder and removed vaginally through the fistula. The patient was then transferred to the ward for interim treatment of a Sitz bath to clean the fistula for later repair.
After 10 days the fistula was deemed operable. A 4 cm vesico‑vaginal fistula and considerable associated fibrotic tissue were identified [Figure 2].[5] The ureteric orifices were far from the fistula margins. Hydro‑dissection was performed using a specially formulated solution (jungle juice). Fistula margins were dissected with scalpel, then scissors to separate the bladder from the vaginal tissue. Some scarred tissues were excised. Bladder tissue was freed from tension. Repair of the bladder was commenced in a transverse direction, inverting the tissue inward using interrupted sutures (polysorb #2‑0). Water‑tight repair of the bladder was achieved by single layer closure and confirmed by negative dye test (methylene blue). Then the repair of the vaginal wall with polysorb suture #0 was performed in a transverse direction. The post‑operative course was unremarkable. The Foley catheter was removed on day 14 with no leakage of urine through the vagina. Despite involvement of a counselor, psychiatrist and hospital social worker, the patient chose not to initiate legal proceedings.
She was discharged with advice to abstain from intercourse for 3 months and we have recommended elective caesarean section should she fall pregnant in the future.
Discussion
Similar cases have been described by other institutes.[2‑6] In these cases foreign bodies in the vagina have been noted to not only cause fistulas, but have also resulted in ureteric obstruction due to formation of bladder stones and ascending infection with possible peritonitis.[4‑7]
Since our patient presented late, the foreign body embedded deep within the vaginal tissue causing significant fibrosis. This increased the difficulty of repair.[2,3] During the initial examination under anesthesia the fistula appeared to be small, but we subsequently discovered the actual deformity to be more than twice the anticipated size after clearing of debris and desquamation.
This incident has significant implications for the patient physically, psychologically and socially. We have endeavored to provide support for her psycho‑social rehabilitation but with limited engagement. In future pregnancy we have recommended elective caesarean section as the mode of delivery. As a nulliparous woman, predicting the outcome of her vaginal delivery would be uncertain (untried pelvis). Even an uncomplicated vaginal delivery may result in the breakdown of tissue and recurrence of this fistula. First repair of fistula has a significantly better outcome than repeated repair.[8] The finding of fibrotic tissue in this case means that if one had to perform a repeat repair, successful closure is not guaranteed.
When a physician is faced with a case of the foreign body within the vagina, we recommend urgent removal of the foreign body, preferably under general anesthesia. However, if the history or physical examination reveals prolonged exposure, repair should be delayed to allow for adequate debridement in order to prevent any life‑threatening complication.
References
- Hilton P. Vesico-vaginal fistulas in developing countries. Int J Gynaecol Obstet 2003;82:285-95.
- Fourie T, Ramphal S. Aerosol caps and vesicovaginal fistulas. Int J Gynaecol Obstet 2001;73:275-6.
- Puppo A, Naselli A, Centurioni MG. Vesicovaginal fistula caused by a vaginal foreign body in a 72-year-old woman:Case report and literature review. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:1387-9.
- Sinha A, Olah KS. Vesicovaginal fistula caused by a foreign body: Delayed presentation and repair with martius graft. J Obstet Gynaecol 2005;25:223-4.
- Goh JT. A new classification for female genital tract fistula. Aust N Z J Obstet Gynaecol 2004;44:502-4.
- Chapman GW Jr. An unusual intravaginal foreign body. J Natl Med Assoc 1984;76:811-812.
- Heintz J, Chason J, Kramer A. Bilateral ureteral obstruction caused by vaginal foreign body: A case report. Can J Urol 2009;16:4870-2.
- Genadry RR, Creanga AA, Roenneburg ML, Wheeless CR. Complex obstetric fistulas. Int J Gynaecol Obstet 2007;99:S51-56.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.