Local Risk Factors in Genital Human Papilloma Virus Infection in Cervical Smears
- *Corresponding Author:
- Dr. EC Ojiyi
Department of Obstetrics and Gynecology, Imo State, University Teaching Hospital, Orlu, Imo State, Nigeria
E-mail: ojiyiemeka@yahoo.com
Abstract
Background: Infection with human papilloma virus (HPV) is the main cause of cervical cancer, but the local risk factors have not been sufficiently assessed. Aim: The study is aimed at determining the prevalence and to evaluate the local risk factors of HPV infection in cervical smears at the Imo State University Teaching Hospital, Orlu, Nigeria. Subjects and Methods: The participants involved 445 randomly selected sexually active women attending the antenatal, postnatal, gynecology and family planning clinics in the Department of Obstetrics and Gynecology of the university between April 2004 and May 2012. A questionnaire assessing various socio‑demographic characteristics of the participants was administered. The pap smears of the participants were examined microscopically for evidence of HPV infection. The SPSS version 17.0 (Chicago, Illinois, USA) was used to compute and analyze the results. The results were presented in tables as simple percentages. Tests of significance using the Chisquare and fisher exact tests were applied where appropriate. Results: The prevalence rate of HPV was 10.3%. The peak age‑specific prevalence of 11.7% occurred in the 15‑19 years age group. There were significant associations between the occurrence of HPV and multiple sexual partners, coital frequency, multiparity, contraceptive use, marital status, low socio‑economic status, abnormal vaginal discharge, irregular menstruation, post‑coital and post‑menopausal bleeding, (P < 0.05). Conclusion: All sexually active women including teenagers should be screened for cervical HPV infection in an organized systematic program equipped with a good call and recall system. There is, therefore, a need to move emphasis from the current practice of opportunistic screening to a systematic screening of the whole population at risk despite cost implications.
Keywords
Genital human papilloma virus, Pap smear, Risk factors
Introduction
Cervical cancer is a preventable disease, but has continued to pose a huge management challenge to the modern day gynecologist. It is the leading cause of death per annum in women aged 35-45 years.[1]
On worldwide basis, cervical cancer constitutes approximately 6% of all cancers in women.[2] An estimated 500,000 new cases are diagnosed every year with about 234,000 deaths.[2] It is the principal cancer of women in most developing countries, where 80% of cases occur, and which have only 5% of global cancer resources.[2,3] It was the most common malignancy amongst women in Nigeria and the rest of sub-Saharan Africa with a very poor survival rate.[1-5] It accounted for 63.1% and 66.2% of histologically confirmed gynecological cancers in Ilorin [2] and Zaria,[4] respectively, in Nigeria.
In 1842, Rigoni-Stern formally hypothesized that cervical cancer had an infective sexually transmitted etiology.[6] Many studies since then confirmed the veneral nature of cervical cancer and identified other risk factors. Molecular epidemiologic evidence clearly indicates that certain types of HPV are the principal cause of invasive cancer and cervical intraepithelial neoplasia.[3]
The HPV has been shown to be a determinant of the natural history of cervical intraepithelial neoplasia (CIN). The progression rate to cervical cancer when HPV co-exists with CIN is about 21% but only 5.6% when CIN lesions occur alone.[7]
Many studies have tried to show some kind of association between age, reproductive factors, marital factors, educational level, religion, occupation, and sexual behaviors with the risk of developing HPV and cervical cancer.[8] Such socio-demographic factors may be useful in risk scoring. This is important because risk scoring systems have the potential for assisting the targeting of screening resources, as broad-risk targeting of all sexually active women is not a viable option for developing countries due to paucity of both human and financial resources. Even in the industrialized nations of the West, the need for more precise targeting of high-risk groups in order to improve the efficiency of cytology programs and conserve funds has become a major issue.[9]
Sub-clinical HPV infections of the cervix may be diagnosed by colposcopy, viral DNA hybridization, polymerase chain reaction (PCR) amplification, histology or by the characteristic HPV changes on Papanicolaou smear.[8,10] The Papanicolaou smear for cervical cytology fulfills all the criteria for an ideal screening test. Not only is it cost-effective, acceptable to most patients, and adoptable to wide-spread screenings, it is specific enough to detect changes and subsequent progression to CIN resulting in decreased morbidity and mortality from invasive cervical cancer.[11] DNA hybridization and PCR amplification can detect both productive and non-productive infection but appear to be of limited value in predicting the risk of developing CIN or invasive carcinoma.[10]
Although cervical cytology, histology and colposcopy are less sensitive, they are capable of detecting significant pathological changes associated with productive HPV infection. The newer HPV detection procedures like the PCR, viral load, DNA hybridization, etc. merely detect the presence of the HPV virus in the tissues, but do not show whether the virus has started causing cellular changes that will eventually culminate in cervical cancer, unlike cytology, histology and colposcopy.[7,8] The aim of this study was to determine the prevalence of human papilloma virus infection in cervical smears taken in women attending gynecological, antenatal, postnatal, and family planning clinics at the Imo State University Teaching Hospital, Orlu and also to determine the epidemiological factors predictive of human papilloma virus infection of the cervix.
Subjects and Methods
This was a Prospective descriptive study involving 445 randomly selected sexually active women attending the antenatal, postnatal, gynecology and family planning clinics in the Department of Obstetrics and Gynecology of the Imo State University Teaching Hospital, Orlu, Nigeria between April 2004 and May 2012. They were recruited after consenting to participate, and a formal approval had been given by the institution’s Ethics and Research Committee. The recruitment continued until a sample size of 445 was reached.
This was calculated using the WHO Epi Info Version 6 program for population sampling.
It was based on a population of 4,261 patients/clients attending the recruiting clinics from April 2004 to May 2012. The expected frequency was 2.34%, the mean of reported studies from other parts of Nigeria.[10,11,12] The minimum acceptable result was taken to be 1.0%. The sample size required at 95% confidence interval was 439 using the formula:
Sample size = n/[1-(n/population)], where n = z*z [P {1-P}]/ (D*D).
The inclusion criteria were all sexually active women attending the above clinics and who consented to participate in the program were included until a sample size was reached. The exclusion criteria were women who declined to consent were exempted, so were those who had never been sexually exposed. In addition, those with obvious cervical warts, fungating, or ulcerative lesions of the cervix from which biopsy may be grossly directed were excluded.
Methods
The purpose, value of the procedure was explained to each prospective patient and her consent sought. All consenting patients had their Pap smears taken using a moistened and unlubricated Cusco’s bivalve speculum and an Ayre’s wooden spatula after a questionnaire on socio-demographics and sexual attitudes had been filled. The smears were transported to the histopathology laboratory immersed in 95% ethanol for preparation, staining and microscopy reading. The HPV produces characteristic cellular changes when it starts multiplying within the cells of the cervix. These inclusion bodies are called koilocytes and their presence within the cells of the cervix on microscopic examination after proper staining is pathognomic of HPV infection.[7,8]
Statistical analysis
The Statistical package for social sciences Version 17.0 (Chicago, Illinois, USA) was used to compute and analyze the results. These included frequency distribution and tests of significance using Chi-square (χ2). The Fisher Exact test was applied where appropriate.
Results
Four hundred and forty-five sexually active women attending various clinics at the Department of Obstetrics and Gynecology, of the Imo State University Teaching Hospital had their Pap smears taken and questionnaires on sexual attitudes, socio-demographics, and symptomatology filled.
Abnormal smears occurred in 238 (53.5%) of the patients screened. Forty-six women (10.3%) had HPV associated with changes, constituting 19.3% of all abnormal smears.
The ages of the participants ranged between 15 and 59 years, with a mean of (SD) 25.8 (4.6). Majority of the patients (65.9%) [293/445] were aged between 20-29 years. They were mostly married (66.1%) [294/445] and parous (69.7%) [310/445], but 24.9% [111/445] had no formal education. There were 429 (96.4%) Christians, while 33% [147/445] either had no occupation or were simply housewives.
Most (69.7%) [301/445] of the participants did not practice any form of contraception; the 30.3% [144/445] who did virtually used hormones (combined pills, progesterone only pills, implants, injectables) or intra-uterine contraceptive device only.
When the various factors studied were individually matched with HPV-associated changes, variable patterns of association were observed. Table 1 shows that there was no significant association between the participants’ age and HPV infection (P = 0.91).
| Age (years) | Positive | Negative | Total |
|---|---|---|---|
| 15-19 | 7 | 53 | 60 |
| 20-24 | 17 | 140 | 157 |
| 25-29 | 13 | 123 | 136 |
| 30-34 | 5 | 47 | 52 |
| =35 | 4 | 36 | 40 |
| Total | 46 | 399 | 445 |
?2 for linear trend=0.07, df=6, P=0.91
Table 1: Association between age and human papilloma virus infection of the cervix
Table 2 shows the association between various sexual attitudes and HPV infection. There was a statistically significant association between multiple sexual partners, coital frequency per week, and the occurrence of genital HPV infection. In Table 3, statistically significant association is shown to exist between multiparity (P = 0.01), contraceptive use (0.02), duration of contraceptive use (P = 0.04), and genital HPV infection.
| Variable | Positive | Negative | Total |
|---|---|---|---|
| Age (years) at first coitus | |||
| 12-15 | 9 | 131 | 140 |
| 16-19 | 25 | 200 | 225 |
| ≥20 | 12 | 68 | 80 |
| Total | 46 | 399 | 445 |
| χ2 for linear trend=0.01, df=1, P=0.92 | |||
| Duration (years) of sexual | |||
| exposure | |||
| ≤10 | 21 | 241 | 262 |
| 11-20 | 14 | 123 | 137 |
| ≥21 | 11 | 35 | 46 |
| Total | 46 | 399 | 445 |
| χ2 for linear trend=0.39, df=6, P=0.53 | |||
| Coital frequency per week | |||
| 1-2 | 23 | 289 | 312 |
| 3-4 | 17 | 101 | 118 |
| ≥5 | 6 | 9 | 15 |
| Total | 46 | 399 | 445 |
| χ2=6.80, df=2, P=0.03 | |||
| Number of sexual partners | |||
| 1 | 8 | 124 | 132 |
| ≥2 | 38 | 275 | 313 |
| Total | 46 | 399 | 445 |
| χ2=4.39, df=2, P=0.03 | |||
| Previous PID*/STD** treatment | |||
| Yes | 30 | 285 | 315 |
| No | 16 | 114 | 130 |
| Total | 46 | 399 | 445 |
| χ2=4.29, df=2, P=0.41 | |||
*Pelvic inflammatory disease, **Sexually transmitted disease, HPV: Human papilloma virus,
Table 2: Association between sexual attitudes and HPV infection of the cervix
| Variable | Positive | Negative | Total |
|---|---|---|---|
| Parity | |||
| Non-parous | 5 | 138 | 143 |
| Parous | 41 | 261 | 302 |
| Total | 46 | 399 | 445 |
| χ2=3.34, df=1, P=0.01 | |||
| Contraception | |||
| None | 8 | 302 | 310 |
| Hormones | 21 | 86 | 107 |
| Intrauterine | 15 | 9 | 24 |
| contraceptive device | |||
| Others | 2 | 2 | 4 |
| Total | 46 | 399 | 445 |
| χ2 for linear trend=83.22, df=3, P=0.02 | |||
| Duration (years) of | |||
| contraceptive use | |||
| <1 | 3 | 59 | 62 |
| 1-5 | 15 | 23 | 38 |
| ≥6 | 18 | 8 | 26 |
| Total | 36 | 90 | 126 |
| χ2 for linear trend=34.20, df=1, P=0.04 | |||
HPV: Human papilloma virus
Table 3: Association between reproductive factors and HPV infection of the cervix
Table 4 shows that there was a statistically significant association between marital status (P < 0.001), occupation (P < 0.001), and genital HPV infection.
| Variable | Positive | Negative | Total |
|---|---|---|---|
| Marital status | |||
| Single | 18 | 10 | 28 |
| Married | 6 | 288 | 294 |
| Widowed | 8 | 24 | 32 |
| Divorced | 14 | 77 | 91 |
| Total | 46 | 399 | 445 |
| χ2 for linear trend=76.68, df=2, P=0.01 | |||
| Number of marriages | |||
| First marriage | 4 | 118 | 122 |
| Two and more marriages | 7 | 164 | 171 |
| Total | 11 | 282 | 293 |
| Fisher exact test=0.59, df=2, P=0.42 | |||
| Type of marriage | |||
| Monogamy | 3 | 107 | 110 |
| Polygamy | 8 | 175 | 183 |
| Total | 11 | 282 | 29 |
| Fisher exact test=1.74, df=2, P=0.22 | |||
| Educational level | |||
| None | 9 | 104 | 113 |
| Primary | 8 | 59 | 67 |
| Secondary | 18 | 168 | 19 |
| Post-secondary | 11 | 68 | 79 |
| Total | 46 | 399 | 445 |
| χ2 for linear trend=0.86, df=2, P=0.41 | |||
| Religion | |||
| Christianity | 41 | 388 | 429 |
| Islam | 5 | 11 | 16 |
| Total | 46 | 399 | 445 |
| χ2=2.99, df=2, P=0.01 | |||
| Occupation | |||
| Single, unemployed | 2 | 14 | 16 |
| Civil servant | 4 | 97 | 101 |
| Petty trader | 13 | 59 | 72 |
| Housewife | 3 | 128 | 131 |
| Student | 11 | 20 | 31 |
| Professional | 4 | 39 | 43 |
| Apprentice | 8 | 16 | 24 |
| Business executive | 1 | 26 | 27 |
| Total | 46 | 399 | 445 |
χ2 for linear trend=26.11, df=5, P=0.01 |
|||
HPV: Human papilloma virus
Table 4: Association between marital status, number of marriages, educational level, religion, occupation, and HPV infection of the cervix
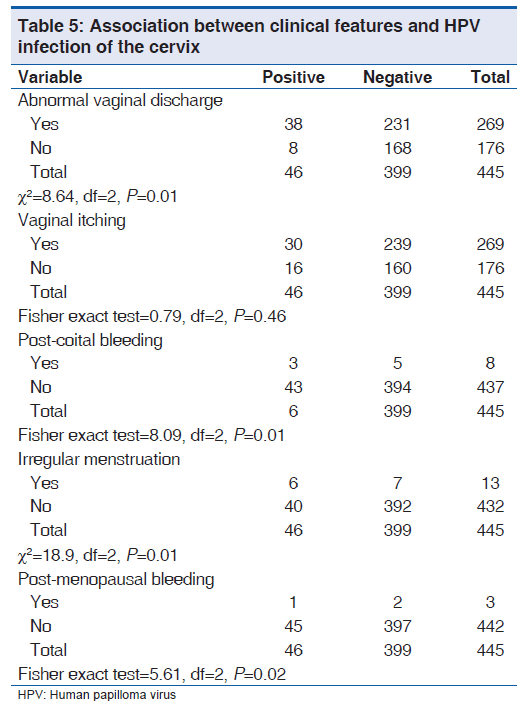
HPV infection was significantly associated with abnormal vaginal discharge (P < 0.001) and irregular menstruation (P = 0.01), as well as post-menopausal (P = 0.02) and post-coital bleeding (P < 0.001) as shown in Table 5. There was no significant association with vaginal itching (P = 0.46).
Discussion
The prevalence rate of HPV infection of the cervix of 10.3% (103 per 1000) in this study is fairly high. It is higher than the 4.01%,[12] 1.8%,[13] and 1.2% [14] reported in Ibadan, Maiduguri, and Enugu, respectively, but lower than the 48% [15] and 32% [16] reported in Brazil and Tanzania, respectively. The differences in all these prevalence rates may be due to differences in the socio-cultural factors of the studied populations and the different diagnostic methods employed.
The absence of any significant difference in the prevalence of HPV between the age groups in this study may be accounted for by the fact that the study population was predominantly young, 79.2% being 29 years or below. However, the peak age-specific prevalence of 11.7% which occurred in the 15-19 years age bracket and the high prevalence of 20.4% [30/293] in the 20-29 years age bracket is in keeping with the findings of other authors, which showed that the rates of cervical human papilloma virus infection were high in teenagers at the onset of their sexual experience [17] and in young adults who belonged to the most sexually active group.[12,17-19] This age range also corresponds to that of other sexually transmitted diseases like gonorrhea and non-gonococcal infections.[11]
Sexual attitudes may influence the occurrence of cervical human papilloma virus infection. Multiple sexual partners and coital frequency were the coital factors significantly associated with HPV infection in this study. These two factors, especially multiple sexual partners, increase the probability of having sexual contact with a male partner harboring the virus since not all men carry the agent. It is hence understandable why all the other sexual attitudes may turn out not to be associated with cervical HPV infection in the absence of multiple sexual partners. This is also the observation of other authors.[11,17-19] Since the duration of infectiveness of HPV is unknown and genital HPV is very common among persons who have been sexually active,[20] the absence of any significant association between HPV and past sexually transmitted diseases might be accounted for by the fact that most women are very reluctant to disclose the details of previously sexually transmitted diseases or their treatment.[16]
There was significant association between contraception, duration of contraception use, and cervical HPV infection. Hormones and their metabolites have been implicated as co-factors in HPV proliferation and the cervical cancer pathogenesis.[21,22] In their work, Von Kenbel Doeberitz, et al.[22] suggested an association between HPV infection and the long-term use of oral contraceptives in the genesis of cervical cancer. Progesterone- and estrogen-responsive elements were identified in the upstream regulatory region (URR) of HPV 18 transgenic mice and in other anogenital HPV types, particularly the high-risk types, which mediate the response of the enhancer to steroid hormones. Progesterone can also suppress the class I human leukocyte antigen surface expression in HPV-positive cervical cells.[23] The effect of contraception might also be secondary to multiple sexual partners due to the ‘safety’ proffered against pregnancy.[24] Those who had used contraceptives for ≥ 6 years had ten times risk than those using contraceptives for less than one year irrespective of the method used, probably buttressing increased sexual promiscuity with contraceptives. There was virtually total absence of use of barrier contraception and hence of any theoretical protection they might provide. Barrier contraceptives such as condoms are less likely to be effective in preventing infections such as genital HPV, which can involve skin not covered by a barrier contraceptive. Studies which have attempted to assess male condom benefit for women have generally found no evidence of protection against infection.[25-30] There is data suggesting a benefit of condom use for men although the studies have not adequately assessed consistency and correctness of condom use. Therefore, condoms should be used if only for prevention of other sexually transmitted diseases.[20]
Multiparous patients in this study stand a statistically significant risk of acquiring genital HPV infection compared to their non-parous counterparts. Multiparity probably reflects early sexual exposure. Early age of first pregnancy, early marriage, early sexual exposure, marital instability, and subsequent multiple sexual partners through remarriages or otherwise are all closely related with synergistic effects. They all increase the chances of acquiring sexually transmitted diseases, including HPV.[4,31] This is in agreement with the works of Schiffman, et al.,[32] and Lorenzato, et al.,[33] who found multiparity to be a risk factor for cervical HPV infection.
There was a statistically significant association between marital status, occupation, and cervical HPV infection. Among occupation groups, those with secured means of livelihood such as housewives (2.3%), business executives (3.7%), and civil servants (4.0%) were at least risk of HPV infection compared to students (37.5%), apprentices (33.3%), and petty traders (18.9%). The underlying factor might be multiple sexual partners as those who engage in sexual promiscuity do so for economic reasons.[11] Married women, probably due to marital stability with only one sexual partner hence less likelihood of exposure to a male carrier of HPV, were 25 times less likely to develop HPV infection of the cervix compared to single sexually active women who would probably have multiple sexual partners and have greater chances of encountering a male carrier of the infection. This is in keeping with the host donor agent theory,[34] which states that every act of coitus has a separate and fixed probability that one or more cells will become available to the carcinogen inoculated within the act of coitus. The significant association between religion and HPV infection is a study bias because almost all the population studied were Christians.
The significant association between cervical HPV infection and the clinical features of abnormal vaginal discharge, irregular menstruation, post-menopausal bleeding is in keeping with the sexually transmitted nature of the virus and its association with the pre-malignant cells and malignant lesions of the cervix as these clinical features are those of lower tract infection since HPV infection might be superimposed with bacterial infection.
This study will help to establish the prevalence of human papilloma virus infection of the cervix in the study population, thereby giving a measure of the potential for the development of pre-invasive cervical lesions in our environment as well as establishing the magnitude of the problem, especially in reference to identifiable epidemiological variables. It would also facilitate an early and appropriate management of such lesions. The study will also serve as part of a database for future studies on HPV infection in our environment. It is hoped that this work will re-kindle interest in the cytology of the cervix on the part of all concerned and facilitate the establishment of an organized cervical cytology program in our center. The required personnel and facilities to run an organized screening program are also available in our center.
Limitations
The two major limitations are that it is a hospital-/clinic-based study, and it is opportunistic. Because of both reasons, the patients may not necessarily represent the general population of women in the larger community. Being a fee-paying teaching hospital, there may be a larger concentration of more privileged and educated women that is representative of the community. Opportunistic screening also tends to be associated with a higher proportion of women of the young age group. In view of these, generalizations regarding the whole community must be made with caution. There is also a limitation in the methodology in that the ultimate diagnosis of HPV infection is based on the detection of viral DNA. Also, the relative contribution of each of the risk factors was not assessed. In addition, cytological diagnoses are fraught with errors. Errors can be made in the interpretation of the smears. Such errors may arise due to the presence of other genital tract infections causing, inflammatory cell exudation and cell degeneration, or cell reaction due to trauma or healing. These can result in false negative or positive results. There is also the problem of sensitivity, specificity, and HPV typing. These are what future researches on the subject will tend to explore.
Conclusion
There is a high prevalence rate of HPV infection among women attending the various clinics of the Department of Obstetrics and Gynecology of the Imo State University teaching hospital, Orlu. This is reflected even among teenagers. There is an association with multiple sexual partners, coital frequency, multiparity, contraceptive use, marital status, abnormal vaginal discharge, post-coital bleeding, and menopausal bleeding. These associations may allow for targeting of a high-risk group in an organized systematic cervical screening program, without discriminating other sexually active women.
This is a very cost-effective way of incorporating HPV testing in the current cervical screening programs in low resource settings such as ours where the newer and better methods of detecting genital HPV infection are not currently available. Multicenter research collaboration using these newer research methods that detect viral DNA is needed to further strengthen the validity of these associations.
The Null Hypothesis is hereby discarded, and the Alternate hypothesis adopted.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Papdopoulus AG, Devaja O, Cason J, Raju KS. The clinical implications of human papilloma virus infection in cervical cancinogenesis and emerging therapies. In: Studd J, editor. Prorgess in Obstetrics and Gynaecology. Vol. 14. Edinburgh: Churchhill Livingstone Publications; 2000. p. 281-93.
- Ijaiya MA, Aboyeji PA, Buhari MO. Cancer of the cervix n Ilorin, Nigeria. West Afr J Med 2004;23:319-22.
- Munoz N, Bosch FX, Sanjosẻ S, Herrero R, Castellsaguẻ X, Shah KV, et al. Epidemiologic classification of human papilloma virus types associated with cervical cancer. N Engl J Med 2003;348:518-27.
- Emebolu JO, Ekwempu CC. Carcinoma of the cervix uteri in Zaria; Aetiological factors. Int J Gynaecol Obstet 1988;26:265-9.
- Rogo KO, Omany J, Oyango JN, Ojwang SB, Stendahl. Carcinoma of the cervix in the African setting. Int J Gynaecol Obstet 1990;33:249-25.
- Rigoni-Stern D. Fatti statistici relativialle malaria cancerose. G Serv Prog Pathol Therap 1842;2;507-17.
- Syrjanen KT, Mantyrvi R, Vayrnen M. Cervical smears in assessment of the course of human papilloma virus infection in prospectively followed men. Act Cytol 1995;31;855-65.
- Koss LG, Durfee GR. Unusual patterns of squamous epithelium of uterine cervix: Cytological and pathologic study of koilocytotic atypia. Ann NY Acad Sci 1956;63:1245-61.
- Wikinson CE, Peters TJ, Harvey IM, Scott NH. Prospective evaluation of a risk scoring system for cervical neoplasia in primary care. Br J Gen Pract 1994;44:341-4.
- Ngokere AA, Ofordile PM. Cytological Evaluation of Cervical Smers in the University of Nigeria teaching hospital, Enugu and environs; A 5-year study. Orient J Med 1996;8:49-52.
- Okesola AO, Fawole OI. Prevalence of Human papilloma virus genital infections in sexually transmitted diseases clinic attendes in Ibadan. W Afr J Obstet Gynaecol 2001;21:622-5.
- Audu BM, El-Nafaty AU, Khali M, Otubu JM. The Influence of Reproductive and marital factors on cervical dyscaryosis. J Obstet Gynaecol 2001;21:622-5.
- Armbruster ME, Loshimoto LM, Leao E, Zugaib M. Prevalence of ‘high risk’ human papilloma virus infection in the lower genital tract of Brazilian gravids. Int J Gynaecol 2000;69:223-7.
- Okeke TA, Okafor J, Akpala CO. Epidemological studies of a cervical cancer screening programme population. Sahel Med J 1999;2:30-3.
- Ter Meulen J, Eberhardt HC, Luande J, Mgaya HN, Chang-Claude J, Mtiro H, et al. Human papilloma virus infection, HIV infection and cervical cancer in Tanzania, East Africa. Int J Cancer 1992;51:515-21.
- Chief Medical Officer, Sexually transmitted disease. Extract from the Annual report of the Chief Medical officer of the Department of health and social security for the year 1980. Br J Vener Dis 1983;50:120-3.
- Blonifield PI, Lancashire RJ, Woodman CB. Can women at risk of cervical abnormality be identified? Br J Obstet Gynaecol 1998;105:486-42.
- Tabrizi SN, Fairley CK, Chen S. Epidemiological characteristics of women with high grade CIN who do and do not have human Papilloma virus. Br J Obstet Gynaecol 1999;106:252-7.
- Koutsky L. Epidemiology of genital human papilloma virus infection. Am J Med 1997;102:3-8.
- Human papilloma viruses and cancer. Cancer Facts. National Cancer Institute. USA: National Institutes of Health; 2002.
- Von Knebel Doebritz M, Spitkovsky D, Ridder R. Interactions between steroid hormones and viral oncogens in the pathogenesis of cervical cancer. Verh Dtsch Ges Pathol 1997;81:233-9.
- Monsonego J, Magdelenat H, Catalan F, Coscas Y, Zerat L, Satre X. Estrogen and progesterone receptors in cervical human papilloma virus related lesions. Int J Cancer 1991;48:533-9.
- Bartholomew JS, Glenville S, Sarkar S, Burt DJ, Stanley MA, Ruiz Cabello F. Integration of high-risk human papilloma virus DNA is linked to the down-regulation of class 1 human leukocyte antigens by steroid hormones in cervical tumour cells. Cancer Res 1997;57:937-42.
- Singer A, Shearman E. Contraception and cervical cancer. Br Med J 1969;4:341-4.
- Cates W. American social health association panel. Estimates of the incidence and prevalence of sexually transmitted diseases in the United States. Sex Transm Dis 1999;26(Suppl):52-7.
- Ho G, Bierman R, Beadsley L, Chang C, Burk R. Natural history of cervico vaginal papilloma virus infection in young women. N Engl J Med 1998;338:423-8.
- Baken L, Koutsy L, Kuypers J. Genital human papilloma virus infection among male and female sex partners: Prevalence and type-specific concordance. J Infect Dis 1995;171:429-32.
- Svare E, Kjaer S. Risk factors for HPV Infection in women from sexually transmitted disease clinics: Comparison between two areas with different cervical cancer incidence. Cancer 1998;75:1-8.
- Strickler H, Kirk G, Figueroa J. HPV 16 antibody prevalence in Jamaica and the United States reflects differences in cervical cancer rates. Int J Cancer 1999;80:339-44.
- Karlsson R, Jonsson M, Edlund K. Life time number of partners as the only independent risk factor for human papilloma virus infection: A population-based study. Sex Transm Dis 1995;22:119-26.
- Burk RD, Kelly P, Feldman J. Declining prevalence of cervico vaginal human papilloma virus infection with age is independent of other risk factors. Sex Transm Dis 1996;23:333-41.
- Harris RW, Brinton LA, Cowdell RH. Characteristics of women with dysplasia or carcinoma in-situ of the cervix uteri. Br J Cancer 1980;42:359-69.
- Schiffman MH, Bauer HM, Hoover RN. Epidemiological evidence showing that human papilloa virus infection causes most cervical intraepithelial neoplasia. Int J Cancer 1996;60:222-34.
- Lorenzato F, Singer A, Moud T, Santos LC, Maia A, Cariri L. Cervical cancer detection by hybrid capture and valuation of local risk factors. Int J Gynecol Obstet 2001;73:41-6.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.