Mass Counseling: Effective Tool to Improve Knowledge, Attitude and Behavior Regarding Blood Donation
- *Corresponding Author:
- Dr. Priya Y Kulkarni
5, Shanti Sadan, Tarte Colony, Erandawane, Pune - 411 004, Maharashtra, India.
E-mail: dr_pdkulkarni@yahoo.co.in
Abstract
Background: Annually, India meets only half of its blood requirement and half of it from unsafe blood donors. There is a need to increase blood donations from safe and voluntary blood donors. Recruitment and retainment of voluntary blood donors are key challenges for blood agencies. Aim: The aim of this study is to assess the impact of mass counseling in the creation of voluntary blood donor. Subjects and Methods: Interventional study with intervention of mass counseling of relatives of patients admitted in the wards of Tertiary Care Hospital attached to medical college in Pune. It was carried out during 1st May 2010 to 31st May 2010. 110 relatives were randomly selected for the study. Mass counseling of cases regarding voluntary blood donation was carried out by trained persons. Pre‑counseling and post‑counseling knowledge, attitude, and behavior (KAB) scores regarding blood donation were assessed using a pre‑tested semi‑structured questionnaire. Results: Counseling improved knowledge, attitude and behavior score (KAB) regarding blood donation significantly. Pre‑counseling and post‑counseling KAB scores difference was statistically significant (P < 0.001) and was not merely by chance. Counseling helped to improve behavior of cases regarding blood donation, too. Conclusion: Continuous counseling sessions for blood donation may serve the purpose for institutes dealing with a large number of people every‑day. Establishment of mobile counseling units by blood banks may help to create a voluntary blood donor. Changes in motivation and the development of self‑identity as a blood donor are needed to retain voluntary blood donors. Incentive's offered for voluntary blood donation card should be strengthened.
Keywords
Africa, Blood donation, Counseling, Voluntary blood donor
Introduction
Blood transfusion saves lives during critical situations, but millions of patients needing transfusion do not have timely access to safe blood.[1] There is only one amazing factory, which makes the blood-human body. Safe blood donor is a blood donor who donates blood voluntarily, without knowing the beneficiary, without any expectation and without being under pressure of a direct or indirect nature. They are from low-risk populations and are the safest blood donors than paid, forced or replacement blood donor from family. Despite this notion, paid/family/replacement donors still provide more than 45% of the blood collected in India.[2]
Blood from unsafe blood donors can cause transmission of dreaded diseases like human immunodeficiency virus-acquired immune deficiency syndrome (HIV-AIDS).[2] Various studies indicate that professional blood donors have little knowledge about HIV-AIDS and represent a high risk group.[3] Such donors are supposed to be associated with a significantly high prevalence of transfusion-transmissible infections (TTIs) including HIV, hepatitis B, hepatitis C, syphilis, and malaria.[4] HIV test-seekers may hide HIV risk behavior and complicate the problem.[5] Transfusion of unsafe blood and blood products accounted for 2.1% of the HIV infections in India in 2004-2005.[6]
There is ever-increasing demand for blood donation from safe donors to meet the deficiency. India requires 8 million units blood per year, but total collection is only 4 million units. 2 million units by voluntary blood donors, 2 million units by relative and exchange donors.[2] Shortage of voluntary blood donors and myths regarding the blood donation are the main reasons behind inadequate blood supply.[7]
Ensuring the widespread availability of safe and quality blood is a critical component of the National AIDS Prevention and Control Program.[2] To ensure safe and adequate blood supply, blood donations from voluntary blood donors are needed to be increased. Voluntary blood donors’ recruitment and retainment is a key challenge before the program.[8].
A pleasant environment in the blood bank, good donor care, polite and effective communication between staff and donors are all important factors for the retention of blood donors. Furthermore, key to recruit and retain safe blood donors is effective donor education and motivation.
To be a safe donor one should have a good awareness with proper knowledge regarding the importance of blood donation.[9] There are various misconceptions regarding blood donation among the population such as it adversely affects health, transmits HIV, etc., They are required to be corrected through proper education and motivation through dissemination of information regarding blood donation.[10]
Public attitudes regarding blood donation are needed to be improved so that they can voluntarily donate the blood.[11] It can be carried out using mass counseling of various groups such as employees of the same institution, college students, people gathered at common places such us hospital, parks, etc.
In the present study, we focused on relatives accompanying admitted patients in hospital. They can serve a huge pool of safe blood donors at the step of hospital if they are aware regarding the importance of blood donation and have good knowledge about it. Such awareness and knowledge can be increased by their mass counseling sessions at the hospital campus itself. It can help to remove misconceptions and make them to come forward to donate blood on their own.
Hence, present study is designed to assess the role of mass counseling as an intervention to create safe blood donors from relatives of patients admitted in one of the Tertiary Care Hospitals attached to medical college in Pune.
Materials and Methods
We designed interventional study with mass counseling as intervention. The study was carried out during 1st May 2010 to 31st May 2010 at one of the Tertiary Care Hospitals attached to medical college in Pune. Permission from the Dean and ethical clearance was obtained from Ethical Committee of the Medical College.
Hospital has out-patient and inpatient facilities with 12 wards. Relatives of patients admitted to these 12 wards, between 18-60 years of age, weighing 45 kg or more served as the study population. Pilot study was conducted on 12 subjects to test the questionnaire. Based on the pilot study, sample size was calculated for the difference in mean knowledge, attitude and behavior (KAB) scores before and after counseling during the pilot study. It came out to be approximately 100. Considering drop outs, it was assigned as 110.
Cases in the pilot study were excluded from further study. Suitable modifications were carried out accordingly in questionnaire [Annexure 1]. Cases were selected by convenient sampling. They were introduced to the study and verbal consent was taken for participation in the study. They were screened for KAB score regarding blood donation using a pre-tested structured questionnaire. Responses to the questionnaire were scored. Score ranged between minimum of 0 and maximum of 10. KAB score > 8 was taken as very good KAB, 6-8 was taken as good, 3-5 as poor and KAB score < 2 was taken as very poor. Cases with good and very good KAB score were grouped to have satisfactory KAB score.
Subjective error was eliminated as interviewer/investigator remained same throughout the study. Contact details of cases including ward of their patient, address, mobile number, landline phone number were noted down for further contact.
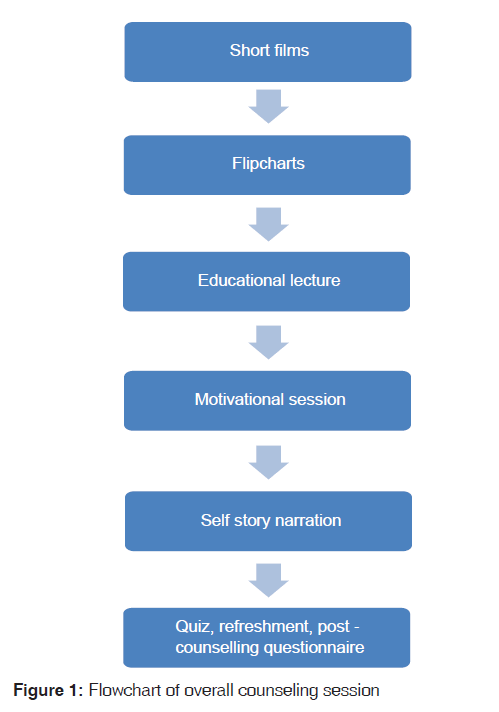
Mass counseling of cases was carried out by trained persons allowing two way interaction. During the session, flip charts, posters were also used to improve knowledge regarding the blood donation. Short films were shown to create awareness regarding the need and importance of blood donation Educational and informational session was held to eliminate fear complex and to create awareness. It included blood need for transfusion in India, harmlessness of blood donation, normal physiology of blood and recuperative power of the human body, principles of donor selection, safe blood transfusion, safety of blood donor, safety of the recipient, and need of self-exclusion by the intending donors when one is not fit to donate blood. It also stressed on how age-old superstitions and myths about blood donation in India are unfair and untrue. It was made illustrative using the power-point presentation and supported by distribution of short attractive reading materials in readers’ friendly language [Figure 1].
Motivational counseling was aimed to encourage, inspire and stimulate people to donate blood, to provide reason and logic to donate blood, develop a desire to solve a social problem and to instill pride for blood donation. Cases were actively involved in discussion by asking their views and believe regarding blood donation. They were corrected through appropriate illustrations and group discussion.
Motivational factors[9] used were:
• Sense of achievement of serving mankind after blood donation
• Certificate for recognition as a blood donor and its advantages
• Voluntary blood donor card for self-identity and its advantages
• Social Responsibility
• Blood donation is part of care they take for self and family.
Session included self-story narration by two people who survived only because of blood transfusion they got on time after having accident. Question and answer session was held lastly. All queries of the cases regarding blood donation were answered by Medical Officer from the blood bank.
Same pretested structured questionnaire was administered again to assess post-counseling KAB score regarding blood donation.
To assess change in behavior, all cases were asked before and after the counseling session whether they will be ready to donate blood in any emergency situation and to receive blood donation card.
Data were entered in a master-table using the SPSS-data editor. Percentages were enlisted for baseline characteristics of study subjects. Paired t test was used of significance used to assess improvement in KAB and Chi square test was used to assess probable change in behavior.
Results
Pre-counseling KAB score was assessed for 110 relatives. Only 6 (5.5%) male relatives had a good knowledge regarding blood donation. Their average score for the questionnaire was 8 out of 10. All of them had donated blood for relatives of the blood camps. Mass counseling session was held after introduction to the subject of blood donation and usual talk regarding blood donation.
Baseline characteristics of study subjects
Age: Majority of study subjects were 15-44 years of age [Table 1]. Only 6 were > 55 years of age. 35.5% were females and 64.5% were males. 9.09% never went to school, 49.09% attended some years of school, 10.91% were graduates 17 (36.54%) were unemployed. As shown in Table 1, unemployed, unskilled, and semiskilled workers, constituted 79.01% study subjects
| Characteristic | Number (n) | Percent |
|---|---|---|
| Gender | ||
| Male | 76 | 64.5 |
| Female | 34 | 35.5 |
| Marital status | ||
| Married | 81 | 73.6 |
| Single | 29 | 26.4 |
| Age (years) | ||
| 15-24 | 17 | 15.5 |
| 25-34 | 36 | 32.7 |
| 35-44 | 32 | 29.1 |
| 45-54 | 19 | 17.3 |
| ≥55 | 6 | 5.5 |
| Type of employment | ||
| Unemployed | 38 | 34.5 |
| Unskilled worker | 27 | 24.5 |
| Semi skilled worker | 23 | 20.9 |
| Skilled worker | 16 | 14.5 |
| Clerical | 05 | 4.5 |
| Semi-profession | 01 | 0.9 |
| Education | ||
| Illiterate | 10 | 9.1 |
| Primary and middle school | 54 | 49.1 |
| High school certificate | 25 | 22.7 |
| Post-high school diploma | 9 | 8.2 |
| Graduation | 12 | 10.9 |
| *Socio-economic status | ||
| I | 4 | 5.4 |
| II | 23 | 31.1 |
| III | 31 | 41.9 |
| IV and below | 16 | 21.6 |
*Socio-economic classification is carried out as per modified Prasad’s classification
Table 1: Baseline characteristics of study subjects
Pre-counseling KAB score
PPre-counseling mean of the score was 3.24 (1.03). 67.7% (74/110) cases had very poor KAB and total, 94.5% (104/110) had unsatisfactory KAB. Good KAB was associated with only educational status (P < 0.001). Good KAB was also associated with knowledge of blood group and previous history of blood donation (P < 0.001).
Post-counseling KAB score
Post-counseling KAB score was 8.65 (+2.74). Difference pre- and post counseling KAB score observed was statistically highly signifi cant (P < 0.001) by paired t test. Counseling improved percentage of study subjects with satisfactory KAB from 5.45% (6/110) to 91% (100/110). Difference was statistically significant by Chi square test [Table 2].
| KAB score | Total | ||
|---|---|---|---|
| Satisfactory | Unsatisfactory | ||
| Pre-counseling | 6 (5.45) | 104 (94.5) | 110 (100) |
| Post-counseling | 100 (91) | 10 (9) | 110 (100) |
*P<0.001 by χ2 test, OR=173.33, 95%, CI=55.30-583.16. KAB: Knowledge attitude and behavior
Table 2: Effect of counseling on KAB about blood donation
It shows counseling helped to improve KAB regarding blood donation significantly.
Change in behavior was assessed by readiness to donate blood. During pre-counseling phase, only 10.9% (12/110) subjects were ready to do so. After the counseling session, 90% (99/110) cases showed readiness to donate blood if an emergency situation arises in hospital Table 3. They registered as voluntary blood donor and accepted blood donation card. Their contact details were noted to contact if such need arises in the future. Difference was observed to be significant by Chi-square test (P < 0.001). Thus, counseling may help to improve behavior regarding blood donation, too.
| Readiness to donate | Total | ||
|---|---|---|---|
| blood | |||
| Yes | No | ||
| Pre-counseling | 12 | 98 (89.10) | 110 (100) |
| (10.9) | |||
| Post-counseling | 99 (90) | 11 (10) | 110 (100) |
*P<0.001 by χ2 test, OR=173.33, 95%, CI=55.30-583.16. KAB: Knowledge attitude and behavior
Table 3: Assessment of probable change in behavior
Discussion
In the present study, mass counseling of relatives of patients admitted in tertiary care hospital attached to one of medical colleges in Pune, Pune increased their knowledge, attitude, and most importantly behavior toward blood donation
We observed many inhibiting factors among the population for blood donation. They were fear of contracting an infection and other adverse health effects, including loss of vitality. Misconceptions about the effects of blood donation are widespread even among educated persons.[8,12] They are required to be corrected through educational activities.[13]
Shenga et al. found that as level of income and education increased, percent of voluntary blood donore increased.[14,15]
During pre-counseling administration of questionnaire, 80% cases gave various reasons for not donating blood such as fear of a needle, fear of getting HIV, weakness etc., All these fears were cleared during counseling session majority of them were ready to donate blood after counseling. In pre-counseling phase, majority of them were not in favor of accepting blood transfusion even if needed in the future because of the risk of acquiring infectious disease. After, counseling the attitude improved in favor of accepting blood donation if an emergency arises. Similar study conducted by Abdul Majeed, in Saudi Arabia reported only 20% of study subjects said that they will not accept blood transfusion.[12]
In one study, Shah et al. convinced regular donors regarding the importance of regular and repeat blood donor. They came forward to donate blood for the cause of humanity (80.6%) and the sense of pride (27.79%). First time donors were less motivated by the cause of humanity (56.21%) and volunteered because of peer pressure (26.03%) and motivated by relative or friend.[16] Blood donor may require some motivations and incentives.[9] Voluntary blood donor can be motivated through counseling sessions. Goncalez et al. classified motivations into three domains categorizing persons by HIV test-seeking behavior. Motivations, in descending order, and their significant associations were: “Altruism”: Female gender, volunteer donor and repeat donor status; “direct appeal”: Female gender, repeat donor status and age 21-50 years; “self-interest”: Male gender, age under 20 years, first-time donor status and lower education.[5] We have some incentives in our National Blood Policy, but they are required to be strengthened much more to get sufficient blood donations
Education had a significant effect on KAB score (P < 0.05). More the education of a person, KAB was good to some extent and its improvement after counseling was also more. Males were more to have good knowledge and during pre-counseling phase study subjects who were excluded from the study as they had a good or very good KAB were all males.
We selected a tertiary level hospital for the study as such hospital requires donated blood more because of a lot of casualties it is dealing with. Simultaneously, large number of inpatients is there with their relatives as they are from nearby villages or other districts. Such relatives reside in hospital campus till relatives are in-patients. They can form a pool of Voluntary Blood Donors in an emergency situation. Only requirement is they should be motivated and traceable. Such sessions can be repeated at other institutions having masses of the population, which can serve potential blood donors. Mobile units can be established for the screening of persons who are willing to donate blood and for blood donation procedure.
Further research is required to understand various other factors contributing to knowledge, attitudes and behavior regarding blood donations. It will help to plan future actions.
Further research is required to understand various other factors contributing to knowledge, attitudes and behavior regarding blood donations. It will help to plan future actions.
Prevention of TTIs depends upon proper pre-donation selection followed by proper serological testing. It assures safety of transfusion of blood minimizing the actual loss of blood units. If blood donor is found to be positive for TTI. Latha reports that out of 113 sero-positive donors studied, nearly 50% of them were aware of their sero-positive status.[17] Such blood donations by sero-positive donors can be avoided by pre-blood donation counseling.
Counseling centers for blood donation should be established in institutes dealing with a large number of people every-day. It will help to create a voluntary blood donor, enter the details in the list of voluntary blood donor and offer the person willing to donate blood with a voluntary blood donor card. Person may get some facilities from that voluntary blood donor card. Pre-donation counseling should be provided before donation in the private area maintaining confidentiality.
Behavior toward blood donation can be modified by changes in motivation and the development of self-identity as a blood donor through counseling. It may help to create first-time voluntary blood donors and then repeat donors.
Acknowledgments
We are grateful to patients and their relatives participated in the study. We are wholeheartedly thankful to the Dean of Medical College attached to the hospital who permitted us to carry out the study in the institution.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Blood safety and availability. Facts and figures from the 2007 WHO. blood safety survey. 2009.
- MOHFW, NACO. Voluntary blood donation programe-An operational guideline. 2007.
- Chattopadhya D, Riley LW, Kumari S. Behavioural risk factors for acquisition of HIV infection and knowledge about AIDS among male professional blood donors in Delhi. Bull World Health Organ 1991;69:319-23.
- WHO. Blood transfusion safety: Voluntary non-remunerated blood donation. 2011.
- Goncalez TT, Sabino EC, Chen S, Salles NA, Chamone DA, McFarland W, et al. Knowledge, Attitudes and Motivations Among blood donors in São Paulo, Brazil. AIDS behav 2008;12:39-47.
- HIV and AIDS in South Asia, an economic development risk. In: Haacker M, Claeson M. editors. The International Bank for Reconstruction and Development/The World Bank. Washingto DC; 2009.
- Sharma V. Tackling disinterest towards blood donation: Need for urgent action. Indian J Med Ethics 2010;7:175-6.
- Zaller N, Nelson KE, Ness P, Wen G, Bai X, Shan H. Knowledge, attitude and practice survey regarding blood donation in a Northwestern Chinese city. Transfus Med 2005;15:277-86.
- Association of Voluntary Blood Donors, West Bengal. National Guidebook on Blood Donor Motivation West Bengal. Ministry of Health and Family Welfare, National Aids Control Organization, Government of India; 2003.
- Alam M, Masalmeh Bel D. Knowledge, attitudes and practices regarding blood donation among the Saudi population. Saudi Med J 2004;25:318-21.
- Wang SS, Fridinger F, Sheedy KM, Khoury MJ. Public attitudes regarding the donation and storage of blood specimens for genetic research. Community Genet 2001;4:18-26.
- Majeed A. Attitude, belief and knowledge about blood donation and transfusion in Saudi Population. Pak Journal Med Sci 2008;24:74-9.
- Benjamin AI, Singh S, Sengupta P, Dhanoa J. HIV sero-prevalence and knowledge, behaviour and practices regarding HIV/AIDS in specific population groups in Ludhiana, Punjab. Indian J Public Health 2007;51:33-8.
- Shenga N, Pal R, Sengupta S. Behavior disparities towards blood donation in Sikkim, India. Asian J Transfus Sci 2008;2:56-60.
- Shenga N, Thankappan K, Kartha C, Pal R. Analyzing sociodemographic factors amongst blood donors. J Emerg Trauma Shock 2010;3:21-5.
- Shah R, Tiwari AK, Shah P, Tulsiani S, Harimoorthy V, Choudhury N. Knowledge about HIV-AIDS among first-time and regular voluntary non-remunerated blood donors. Indian J Pathol Microbiol 2007;50:896-900.
- Latha B. Efficacy of counseling for seropostive donors. Asian J Transfus Sci 2011;5:63-109.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.