Maternal Outcomes of Pre-eclampsia in an Ethiopian Gynecologic Hospital
2 Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
3 Department of gynecology and obstetrics, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
4 Department of Clinical Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia, Email: mb6767@gmail.com
Citation: Seid I, et al. Maternal Outcomes of Preeclampsia in an Ethiopian Gynecologic Hospital. Ann Med Health Sci Res. 2017; 7: 16-21
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Pre-eclampsia is one of the causes of maternal morbidity and mortality throughout the world. It is common problem in developing countries. This study was aimed to assess the maternal outcomes of pre-eclampsia management among pregnant women at Gandhi Memorial Hospital. Methods: A retrospective cross-sectional study was conducted on preeclamptic women who were admitted to maternity ward of Gandhi Memorial Hospital in a one year period. Data regarding patient characteristics and treatment outcome (eg. maternal death, maternal complication, hospital stay) were collected. Data was collected using data collection format from patient medical charts. Epinfo version 7 was used for data entry and data was analyzed using SPSS version 21. Descriptive statistics and logistic regression were used. All the statistical tests were significant at P-value < 0.05. Results: A total of 200 mothers’ medical charts were reviewed. One hundred sixty five (82.5%) pregnant women were diagnosed with severe preeclampsia. More than one third (35.5%) of the women developed complications. The most common maternal complication was HELLP syndrome. Mothers with gestational age less than 37 weeks were 5.2 times more likely to develop complication [AOR=5.22, 95% CI = 2.21- 12.3]. Mothers with antipartum preeclampsia were 8.7 times more likely to have prolonged hospital stay [OR=8.7 (95% CI=1.35- 10.02]. Conclusion: The commonly seen poor treatment outcomes in preclamptic mothers were magnesium sulphate toxicity, prolonged hospital stay and development of complications. Preeclampsia at gestational age of less than 37 weeks significantly increases the risk of developing maternal complication.
Keywords
Pre-eclampsia; Maternal outcome; Gestational hypertension; Ethiopia
Introduction
Pre-eclampsia is a pregnancy-specific syndrome observed after the 20th week of pregnancy with systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mmHg recorded twice 6 hours apart or a single measurement of ≥ 160/110 mmHg, accompanied by significant proteinuria. [1] preeclampsia may be mild or sever based on its presentation. Severe pre-eclampsia is a blood pressure of ≥ 160 mmHg (systolic) or 110 mmHg (diastolic) and associated proteinuria of 5 grams or more per day. Pre-eclampsia may also be regarded as severe in the presence of involvement of multiple organs including thrombocytopenia (platelet count < 100,000/uL), pulmonary edema, or oliguria. In contrast, mild Pre-eclampsia is characterized by an elevated blood pressure less than 160 mmHg (systolic) or 110 mmHg (diastolic) with proteinuria greater than 300 mg, but less than 5 g per day. [2]
Once the diagnosis of severe pre-eclampsia is established, admission to hospital is required for close surveillance of blood pressure and biochemical parameters, including a full blood count, liver and renal function tests and clotting studies based on the severity. As pre-eclampsia is a progressive disease, delivery will often be required within two to three weeks of admission. Women should also be carefully monitored in the postpartum period as highest blood pressure measurements often occur three to four days after delivery. All women should have their blood pressure taken and urinalysis done at their sixweek postnatal checkup. [3]
Antihypertensive treatment should be started in women with a systolic blood pressure ≥ 160 mmHg or a diastolic blood pressure ≥ 110 mmHg. Labetalol, nifedipine, hydralazine or methyldopa can be used for the acute management of severe hypertension. Magnesium Sulphate should be considered for women with pre-eclampsia if there is suspection that eclampsia will occur. This is usually in the context of severe pre-eclampsia once a delivery decision has been made and in the immediate postpartum period. [4]
Maternal complications of pre-eclampsia include cerebral complications like (seizures, cerebral hemorrhage, cerebral infarction, severe headache and blurred vision), and liver capsular rapture, renal failure, haemolysis, elevated liver enzymes and low platelets (HEELP syndrome) and death. [5]
Preeclampsia continues to be an important cause of maternal morbidity and mortality. 16% of direct maternal mortality and 10% of all maternal mortality (direct and in direct) was due to preeclampsia/eclampsia. [6] Preeclampsia occurs in 7-10% of pregnancies with a case fatality rate of 6-10% worldwide. It is more common in developing countries and it probably accounts for more than 40,000 maternal deaths worldwide each year. [7] WHO estimated the incidence of preeclampsia to be seven times higher in developing countries than developed countries? [8] According to a population based study in South Africa the incidence of hypertensive disorders of pregnancy (HDP) was 12%. Studies in Ethiopia showed that the incidence of HDP is around 5% of which majority were due to severe preeclampsia. [9]
A maternal mortality trend analysis showed an increasing trend of preeclampsia in Ethiopia. [10] A study done in Western Shoa found that 12.3% maternal mortality occurred from hypertensive disorder of pregnancy. [11] The case fatality rate of pre-eclampsia/eclampsia in two teaching hospitals in Addis Ababa (Tikur Anbessa and St Paul’s Hospitals), is 13%. [12]
A study done to evaluate the maternal and fetal outcome of pregnant woman with pre-eclampsia showed maternal morbidities were common in patients with severe pre-eclampsia. Pre-eclampsia related complications were placental abruption in 12%, eclampsia in 4% and renal failure seen in 2.7% of the women. [13]
A study done to evaluate the maternal and fetal outcome of pregnant woman with pre-eclampsia showed maternal morbidities were common in patients with severe pre-eclampsia. Pre-eclampsia related complications were placental abruption in 12%, eclampsia in 4% and renal failure seen in 2.7% of the women. [13]
Methods
Study setting
This study was conducted at Gandhi memorial hospital (GMH), Addis Ababa, Ethiopia. The hospital is a governmental, regional referral hospital, which provides gynecologic and maternity services. The hospital has 110 maternal beds and 15 neonatal beds. The labor and maternity wards are run by nurses, midwives, health officers, interns, resident physicians of obstetrics and gynecology specialty, and obstetrics and gynecology consultants. The hospital daily manages 25 -30 deliveries for mothers who come from Addis Ababa and its surroundings.
Study design and study subject
A retrospective cross-sectional study design was used to assess maternal outcomes of pre-eclampsia in Gandhi Memorial Hospital. The charts of two hundred pregnant mothers were selected by systematic random sampling technique. All Patient Medical records with the diagnosis of mild and severe preeclampsia were considered and Patient medical records with incomplete information for the research question were excluded.
Data collection and management
Data was collected using data collection format developed by the research authors after reviewing literatures. The format consists of maternal details (age, GA, gravidity, parity, previous history of preeclampsia and hypertension) , ANC follow up , type of diagnosis, time of occurrence of preeclampsia , admission status of the mother to the intensive care unit, duration of hospital stay, major maternal complications (Liver failure, renal failure, HELLP syndrome and oligouria).
Data was collected by two nurses from GMH after proper training for two days. Data was collected from the hospital delivery care register, admission/discharge registration book and patient medication charts. Prior to data collection each patient medication charts was coded and arranged in sequence to avoid confusion and repetition during data collection.
The data collection format was pre-tested on 5% of the sample population from Yekatit Asrahulet Hospital (Addis Ababa, Ethiopia) in order to check any inconsistencies. Necessary adjustments were made accordingly before the actual period of the study. The completeness, consistency, and accuracy of the data were checked every day by the principal investigator.
Data was coded and entered in to the Epinfo version 7 software. Then, data was exported to SPSS (version 21) for analysis. Descriptive statistics was done and results are presented in tables and figures. A test of association was done using binary and multivariate logistic regressions. All the statistical tests were significant at P-value less than 0.05.
Ethical considerations
The study was commenced after ethical clearance was secured from the Ethical Review Committee of School of Pharmacy, College of Health Sciences, Addis Ababa University and Addis Ababa Health Bureau. Concerned bodies at all levels, including the hospital medical director and Department of Obstetrics and Gynecology, were officially communicated and permission was granted. Any personally identifiable information (e.g. name and address) was not recorded on the data collection format to maintain confidentiality of the study participants.
Results
Socio-demographic characteristics
A total of 200 mothers medical charts were reviewed during the study period. The mean age of the study subjects was 27 years with a standard deviation of 4.5. As shown in Table 1 majority of them, 115 (57.5%) were in the age group of 25-34 years. One hundred eight (54%) of the pregnant women were primigravida. More than half of the patients 121 (60.5%) were nulli-parous.
| Variables | Group | N (%) |
|---|---|---|
| Age | 18-24 | 71 (35.5) |
| 25-34 | 115 (57.5) | |
| 35-49 | 14 (7.0) | |
| Gravidity | Pimigravida | 108 (54) |
| Multigravida | 92 (46) | |
| Parity | Nulli parous | 121 (60.5) |
| Primiparity | 50 (25) | |
| Multi para | 29 (14.5) |
Table 1: Socio-demographic characteristics of pregnant women admitted with the diagnosis of pre-eclampsia (n=200), GMH, Addis Ababa, Ethiopia.
Background characteristics
As shown in Table 2, majority of the study subjects (96.5%) had antenatal care follow up. One hundred thirty five (67.5%) of the pregnant women had gestational age at presentation ≥37 weeks. One hundred sixty five (82.5%) and 35 (17.5%) pregnant women were diagnosed with severe preeclampsia and mild preeclampsia respectively. Most of the pregnant women (98.5%) had no previous history of hypertension and (94.5%) had no history of preeclampsia. The time of occurrence of preeclampsia in most participants 172 (86%) were during antepartum period. Most of the referral 144 (72%) was from Primary health care centers. The main reasons for caesarean section were non-reassuring fetal heart rate pattern (NRFHRP) (33.6%), severe pre-eclampsia (19.5%) and NRBPP (15%).
| Variables | Category | N (%) |
|---|---|---|
| ANC follow up | Yes | 193 (96.5) |
| No | 7 (3.5) | |
| Diagnosis at admission | Severe pre-eclampsia | 165 (82.5) |
| Mild pre-eclampsia | 35 (17.5) | |
| Patient referred from | Hospital | 42 (21) |
| Private clinic | 14 (7) | |
| Primary health care | 144 (72) | |
| Previous history of Hypertension | Yes | 03 (1.5) |
| No | 197 (98.5) | |
| Previous history of Preeclampsia | Yes | 11 (5.5) |
| No | 189 (94.5) | |
| Gestational age at admission | ≥ 37 | 135 (67.5) |
| < 37 | 65 (32.5) | |
| Occurrence of Pre-eclampsia | Antepartum | 172 (86) |
| Intrapartum | 21 (10.5) | |
| Intrapartum | 7 (3.5) | |
| Mode of delivery | CS | |
| SVD | ||
| Forceps | ||
| Reason for C/S | NRFHRP | 38 (33.6%) |
| SPE | 22 (19.5%) | |
| NRBPP | 17 (15%) | |
| Others* | 36 (31.9 %) |
Table 2: Background characteristics of pregnant women admitted with the diagnosis of pre-eclampsia (n=200), GMH, Addis Ababa, Ethiopia.
Maternal outcomes
There was only one maternal death, accounting for a case fatality rate of 0.5%. As indicated in Table 3 more than one third (35.5%) of the women developed complications. There was no maternal admission to ICU and 82 (41%) of the women had a prolonged hospital stay (>7 days). Low urine output and depressed deep tendon reflex were the most common symptoms of magnesium sulphate toxicity that was observed in 45 (22.5%) and 30 (15%) of the pregnant mothers respectively.
| Variables | Category | N (%) |
|---|---|---|
| Maternal outcome | Improved | 199 (99.5) |
| Death | 1 (0.5) | |
| Hospital stay | < 7 | 118 (59) |
| ≥ 7 | 82 (41) | |
| Maternal Complication | Yes | 71 (35.5%) |
| No | 129 (64.5%) | |
| Magnisum sulphate -toxicity Symptoms | Low UOP | 45 (22.5) |
| Abnormal DTR | 30 (15) | |
| Low RR | 1 (0.5) |
Table 3: Maternal outcomes of pregnant women admitted with the diagnosis of pre-eclampsia (n=200), GMH, Addis Ababa, Ethiopia.
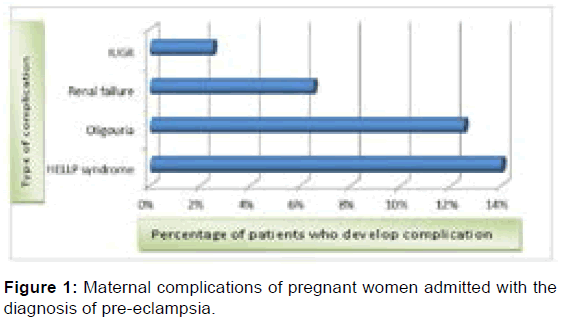
As shown in Figure 1, the most common maternal complication was HELLP syndrome developed in 28 (14%) of the women. 25 (12.5%) of the women developed oligouria and 13 (6.5%), 5 (2.5%) of the women also developed renal failure and IUGR.
Factors associated with maternal outcome
Out of the 200 mothers 71 (35.5%) had developed at least one complication. As depicted in Table 4 univariate logestic regression analysis showed GA, diagnosis at admission, SBP and DBP have statistically significant association with maternal complications. On multivariable logistic regression, it was found that GA was found to be independent predictors of complication. Accordingly, mothers with gestational age less than 37 weeks were 5.2 times more likely to develop complication [AOR=5.22, 95% CI = 2.21-12.3].
| Factors | Group | Complication | COR | AOR | |
|---|---|---|---|---|---|
| No | Yes | (95 %CI) | (95 %CI) | ||
| GA | <37 | 46 (70.8) | 19 (29.2) | 5.14 (2.16-12.89) | 5.22 (2.21-12.3) † |
| ≥ 37 | 125 (92.6) | 10 (7.4) | 1.00 | 1.00 | |
| Diagnosis | mild PE | 34 (97.1) | 01 (2.9) | 1.00 | 1.00 |
| Sever PE | 137 (83) | 28 (17) | 6.95 (0.91-52.90) | 1.17 (0.07-20.03) | |
| SBP | <160 | 37 (97.4) | 01 (2.6) | 1.00 | 1.00 |
| ≥ 160 | 134 (82.7) | 28 (17.3) | 7.73 (1.02-58.73) | 5.37 (0.28-03.61) | |
| DBP | <110 | 68 (91.9) | 06 (8.1) | 1.00 | 1.00 |
| ≥ 110 | 103 (81.7) | 23 (18.3) | 2.53 (0.98-6.54) | 1.43 (0.48-4.28) | |
Table 4: Factors associated with maternal complications of pregnant women admitted with the diagnosis of pre-eclampsia (n=200), GMH, Addis Ababa, Ethiopia.
As indicated in Table 5, from all the mothers 82 (41%) had a prolonged hospital stay. most of the mothers who had a prolonged hospital stay developed preeclampsia in the antepartum period. Accordingly, mothers with antipartum PE were 8.7 times more likely to have prolonged hospital stay [AOR=8.7 (95% CI=1.35- 10.02].
| Factors | Group | Hospital stay | COR | AOR | |
|---|---|---|---|---|---|
| <7 days | ≥7 days | (95 %CI) | (95 %CI) | ||
| Types of PE | Antepartum | 94 (54.7) | 78 (45.3) | 1.80 (1.33-10.00) | 8.7 (1.35- 10.02) † |
| Intrapartum | 19 (90.5) | 02 (9.5) | 0.13 (0.03-0.56) | 0.25 (0.03-2.23) | |
| Post-partum | 05 (71.4) | 02 (28.6) | 1.00 | 1.00 | |
CI: Confidence Interval
Table 5: Factors affecting hospital stay of pregnant women admitted with the diagnosis of pre-eclampsia (n=200), GMH, Addis Ababa, Ethiopia.
Discussion
Preeclampsia is a leading cause of maternal morbidity and mortality throughout the world [14] and it is common problem in developing countries because of illiteracy, poor ANC follow up and lack of health awareness. [15] As compared to women in developed countries a women in developing countries is seven times more likely to develop preeclampsia. 10-25% of preeclampsia cases in developing countries will result in death of the mother. [16]
Majority of preclamptic mothers in our study were primigravidic (54%) and nulliparous (60.5%). Similarly a study conducted in India showed that primigravidas accounted for majority of preeclampsia groups as compared to multigravidas [17] and a study in Jimma showed that 66.5% of the mothers were nulliparous. [9]
Almost all patients (96.5%) had antenatal care (ANC) followup. Similar studies conducted in Jimma University Specialized Hospital showed about three fourth of mothers had antenatal care follow-up. [9,18] Another study in Nigeria showed 76.6% of the pregnant mothers received antenatal care at the study center. [19] In the contrary a study in India shows 82% of the mothers had no antenatal care follow up [15] and another study done by Sultana and Aparna found that most of the pregnant women did not receive antenatal care with incidence of 62.5%. [17] The higher rate of antenatal care follow up in the current study could be because of the awareness created by the current governmental interventions and improvement in antenatal care coverage.
Many of the mothers (82.5%) in this study were admitted because of sever preeclampsia. A study in India showed among the 200 cases of pre-eclampsia, (55.5%) were diagnosed as severe Preeclampsia. [17] Large number of severe preeclampsia cases in this study could be due to the fact that the study was undertaken in a referral hospital which serves more advanced cases which were difficult to be managed at a lower level. In the current study the type of occurrence for preeclampsia in most of the cases were antepartum (86%). Similarly a study in India showed that 80.4% of the mothers have antepartum preeclampsia. [15]
Caesarean section was a common mode of delivery for mothers with pre-eclampsia (56.5%) and NRFHRP was the common indication for Caesarean section. The reason for the majority of the mothers delivered by CS in this study could be due to the large proportion of severe pre-eclampsia cases and the only definitive treatment for such cases is delivery of the placenta. The poor monitoring practice of magnesium sulphate may contribute for NRFHRP to be the common indication for caesarean section as persistant bradycardia is one of the ADR of magnesium sulphate. [20]
In this study there was one death report (0.5%) but no maternal admissions to ICU. This is low as compared to the result of the study done by Savita et al which reported 8% maternal mortality. [15] Closer to the current study result no maternal death was recorded in the study done by Ugwu et al. [19] Another study in Jimma, Ethiopia reported two (2.5%) maternal deaths among preeclamptic women. [9] A study in India, Hyderabad, showed there were 3 (4%) maternal deaths due to severe pre-eclampsia. [15] A decrease in maternal death in this study could be due to an improvement in early antenatal and post natal care follow up. In addition the introduction of magnesium sulphate as a prophylaxis of seizure in case of severe preeclampsia could have a role in decreasing maternal mortality. [19,21-24]
The most common maternal complication was HELLP syndrome developed in 28 (14%) of the women. HEELP syndrome occurs in 1 of 1000 over all pregnancies but it reaches 4-12% in patients who develop sever preeclampsia. [25] A study in Jimma reported that HELLP syndrome was one of the most severe forms of the disorder affecting 8.9% of the mothers. [9] A study in Bangkok showed one of the common maternal complications was HELLP syndrome occurred in 10.1% of subjects. [26] Study in India showed 2% of the mothers developed HELLP syndrome. [15] A relatively higher HELLP syndrome cases in this study may be due to delays in early detection and timely management of preeclamptic women at health centers as most of the mother were referred from primary health centers where HELLP syndrome may developed but platelet transfusion may be impossible.
In the current study, out of the 200 mothers 82 (41%) had prolonged hospital stay. A study in Nigeria showed 11.7% of the mother had a prolonged hospital stay. [19] Similar study in Jimma reported 11.2% of the mothers had prolonged hospital stay. [18] A relatively higher number of mothers with prolonged hospital stay in this study could be due to higher rate of complication since all of them were referred patients with large proportion of advanced cases. Therefore, in order to manage such complications additional days of hospitalization would be needed.
Regarding toxicity of magnesium sulphate in this study, it has been found that low urine output was the most commonly reported toxicity (22.5%) followed by DTR (15%). A retrospective study conducted in Nigeria reported that the observed magnesium sulphate toxicities were acute renal and respiratory depression in 9% of patients. [27] Similarly the Magpie Trial indicated intramuscular injection site problems account for 12% of magnesium sulphate received pregnant women. [28] A relatively more drug toxicity recorded in this study could be due to poor monitoring practice for magnesium sulphate. Proper administration of magnesium sulphate is again a problem in many low resources settings like ours where electric infusion pumps are not available for intravenous administration.
The current study showed gestational age at delivery is the most important independent predictor for maternal outcomes like maternal complication. According to a retrospective study in India preterm (< 37 week of gestation) delivery was found to be associated with poor maternal outcome. [29,30]
The study is limited by its retrospective nature and its dependence on patients’ records so that missed information may bias the result of the study. Furthermore this hospital-based approach includes only women attending the hospital; as many women die in rural Ethiopia without visiting a health facility, the result of the study may not represent maternal outcomes of women with preeclampsia in non-hospital settings.
Conclusion
The commonly seen poor treatment outcomes in preclamptic mothers were symptoms of magnesium sulphate toxicity, prolonged hospital stay and development of complications like HELLP syndrome, oligouria and renal failure. Development of Preeclampsia at gestational age of less than 37 weeks significantly increases the risk of developing maternal complication. Mothers with antipartum PE were more likely to have prolonged hospital stay.
Acknowledgements
We would like to thank Addis Ababa University for its financial support in conducting this research. We would also like to extend our gratitude to the staffs who were working in the card room, nursing department and department of Gynecology and Obstetrics of Gandhi Memorial Hospital for providing us the necessary information and their cooperation in the data collection process.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Sibai B, Chames M. Chronic Hypertension in Pregnancy. Glob Libr Women's Med. 2008.
- Carl H, Kara M, Pamela M, Leandro C, Craig A, Peter J. Maternal preeclampsia and neonatal outcomes. J Pregnancy. 2011; 22: 1-7.
- Manju C, Jason W, Andrew S. Management of hypertension and pre-eclampsia in pregnancy. Trends in Urology Gynaecology & Sexual Health. 2007; 22-29.
- Saxena R. 2014. Bedside Obstetrics & Gynecology. 2nd ed. Jaypee Brothers Medical Publishers Private Limited, New Delhi, Page 497.
- Rathore RB, Iqbal A, Khan M. Complications and outcome of patients of pre-eclampsia and eclampsia presenting to medical wards of Mayo Hospital Lahore. ANNALS. 2010; 16:1
- Gaym A, Bailey P, BLuwei P, Admasu K, Gebrehiwot Y. Disease burden due to pre-eclampsia/eclampsia and the Ethiopian health system’s response. Int J Gynecol Obstet. 2011; 115: 112-116.
- Bharti C. Role of 2 gram calcium supplementation in prevention of pre-eclampsia in high risk cases. JEMDS. 2013; l2: 7205-7210.
- Osungbade K, Ige O. Public health perspectives of preeclampsia in developing countries: implication for health system strengthening. J Pregnancy 2011; 48: 10-95.
- Zenebe W, Hailemariam S, Mirkuzie W. Hypertensive disorders of pregnancy in jimma university specialized hospital. Ethiop J Health Sci. 2011; 21: 147-154.
- Abdella A. Maternal mortality trend in Ethiopia. Ethiop J Health Dev. 2010; 24: 115-122.
- Garomssa HD, Dwivedi A. Maternal mortality in Ambo Hospital: a five year retrospective review. Ethiopian J Reprod Health. 2008; 2: 2-13.
- Misganaw A, Zufan L. Eclampsia a five years retrospective review of two hundred sixteen cases managed in two teaching hospitals in Addis Ababa. Ethiop. Med. J. 2006; 44: 27-31.
- Shabnam S, Najma B, Shehla C, Ambreen G. Outcome of pregnancy in women with severe pre-eclampsia. MC. 2012; 19: 41-45
- Preeclampsia: A decade of perspective, building a global call to action. Preeclampsia Foundation, Melbourne, Florida, Nov 2010.
- Savita R, Deepika P, Anshu S, Smiti N. Maternal and perinatal outcome in sever preeclampsia and eclampsia. South Asian Federation of Obstetrics and Gynaecology. 2009; 1: 25-28.
- Maternal mortality in 2005: Estimates developed by WHO, UNICEF, UNIFPA and the World Bank, Geneva, World Health Organization, 2007.
- Sultana A, Aparna J. Risk factors for pre-eclampsia and its perinatal outcome. Ann Biol Res. 2013; 4: 1-5
- Kassie GM, Negussie D, Ahmed JH. Maternal outcomes of magnesium sulphate and diazepam use in women with severe pre-eclampsia and eclampsia in Ethiopia. Pharm Pract. 2014; 12: 400.
- Ugwu EO, Okonkwo CD, Nwankw TO. Maternal and perinatal outcome of severe pre-eclampsia in Enugu, Nigeria after introduction of Magnesium sulphate. Niger J Clin Pract. 2011; 14: 418-421
- Duffy CR, Odibo AO, Roehl KA, Macones GA, Cahill AG. Effect of magnesium sulfate on fetal heart rate patterns in the second stage of labor. Obstet Gynecol. 2012; 119: 1129-1136.
- Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al. Do women with preeclampsia and their babies, benefit from magnesium sulphate? The Magpie trial: a randomised and placebo-controlled trial. Lancet 2002; 359: 1877-1890.
- Duley L, Gulmezoglu AM, Henderson-Smart DJ. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia (Cochrane Review). Oxford: The WHO Reproductive Health Library CD-ROM No. 10; 2007.
- Duley L, Gulmezoglu AM, Henderson-Smart DJ, Chou D. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2010; 11: CD000025.
- Muganyizi P, Shagdara M. Predictors of extra care among magnesium sulphate treated eclamptic patients at Muhimbili National Hospital, Tanzania. BMC Pregnancy Childbirth. 2011; 11: 41.
- Gupta T, Gupta N, Jain J, Gupta S, Bhatia P, Bagla J. Maternal and perinatal outcome in patients with severe preeclampsia/eclampsia with and without help syndrome. Journal of Universal College of Medical Sciences. 2013; 1: 7-12
- Sujittra J, Somchai T. Perinatal Outcomes in Severe Preeclamptic Women between 24-33+6 Weeks’ Gestation. J Med Assoc Thai. 2008; 91: 25-30
- Khan I. Magnesium sulfate versus diazepam infusion in eclampsia, Annals of KEMU. 2009; 15: 149-151.
- Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, et al. Magpie Trial Collaboration Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo controlled trial. Lancet. 2002; 359: 1877-1890.
- Swamy MK, Patil K, Nageshu S. Maternal and perinatal outcome during expectant management of severe pre-eclampsia between 24 and 34 weeks of gestation. J Obstet Gynaecol India. 2012; 62: 413-418
- Sibai BM. Preeclampsia as a cause of preterm and late preterm (near-term) births. Semin Perinatol. 2006; 30: 16-19.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.