Maturogenesis and Osseous Healing of a Necrotic Immature Premolar using Revascularization Procedure - A Case Report and Review of Literature
Citation: Mustafa MME. Maturogenesis and Osseous Healing of a Necrotic Immature Premolar using Revascularization Procedure- A Case Report and Review of Literature. Ann Med Health Sci Res. 2018;8:39-44
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Immature permanent teeth with pulpal necrosis present a clinical challenge to endodontists. Since debridement of pulp canal space is difficult, there is an increased possibility of root perforation and cervical root fracture, besides the presence of an open immature root apex jeopardize the apical seal of a root canal treatment resulting in subsequent failure. Regenerative endodontic Procedures provide an unconventional approach which relies on the principle of tissue engineering. The treatment outcomes of revascularization of necrotic immature permanent teeth have been shown to promote tooth maturogenesis and bone healing. This report presents a case of revascularization of a necrotic left mandibular premolar with apical periodontitis and interseptal bone defects using minimal canal instrumentation and calcium hydroxide paste as a root canal disinfectant. At a following visit, blood clot was evoked in the canal by irritating periapical tissues and the canal properly sealed with mineral trioxide aggregate, glass ionomer cement and composite resin. The case was followed for thirty-eight-month and deemed to be clinically normal with a positive response to cold test (Endo-frost, Roeko, UK). Radiographic evaluation showed root maturogenesis and complete osseous healing which was evident in the apical and interseptal bones.
Keywords
Apexification; Immature permanent tooth; Necrosis; Pulp revascularization
Introduction
Immature permanent teeth with pulpal necrosis present a clinical challenge to endodontists, with the facts that debridement of pulp canal space is not guaranteed, there is an increased possibility of root perforation and cervical root fracture due to thin root dentine and the presence of an open immature root apex jeopardize the apical seal of a root canal treatment resulting in subsequent failure. Regenerative endodontic Procedures provide an unconventional approach which relies on the principle of tissue engineering. [1-3]
Conventionally, necrotic immature permanent teeth were treated with traditional calcium hydroxide apexification techniques or more recently MTA was used to treat immature teeth with pulp necrosis in a single visit setting. [4]
However, apexification with calcium hydroxide has several drawbacks, including unpredictability of treatment time, several recall visits are needed to place and replace calcium hydroxide to avoid possible weakening of the root structure and subsequent root fracture, also root dentin does not increase in thickness and remain stunted. [3,5-7]
A new treatment modality of revascularization of immature necrotic permanent teeth was introduced in the past several years. The concept of revascularization was first established by Ostby [8] in 1961, and in 1966, Rule and Winter [9] reported root development and apical barrier formation in cases of pulpal necrosis in children.
Successful Revascularization of an immature permanent tooth with increased root length and root dentin width have been reported after appropriate canal disinfection and the presence of a scaffold (blood clot) in the canal space for both human and in animals. [10]
Revascularization procedures in general require the use of an intracanal disinfectant which is regarded as a major prerequisite for success. [2,3,5,11,12]
The triple antibiotic paste (TAP) consisted primarily of a mixture of ciprofoxacilin, metronidazole and minocycline which has been reported to be effective in bacterial elimination and canal disinfection. [13]
Calcium hydroxide has been extensively used as an intracanal medicament in mature and immature permanent teeth owing to its known antibacterial effects. Its increased PH impedes bacterial proliferation and it has also been reported to decrease the likelihood of discoloration following revascularization procedures. On the other hand, high PH of Calcium hydroxide can prevent vital tissue growth in the root canal space and the difficulty of its complete washout might lead to diminished space required for tissue regeneration. Moreover, Calcium hydroxide can induce a hard tissue response instead of pulp-like structures. [14,15]
The treatment outcomes of revascularization have been shown to result in increased thickening of the canal walls by deposition of hard tissue and/or encourage continued root development in immature permanent teeth with necrotic pulp tissue and/or apical periodontitis/abscess. [6]
This case report presents a thirty-eight-month follow-up of a necrotic immature mandibular premolar with apical periodontitis treated with revascularization procedures using calcium hydroxide with iodoform paste (Mitapex) as a root canal disinfection dressing material. The tooth showed continued root development, apical closure and osseous healing.
Case Report
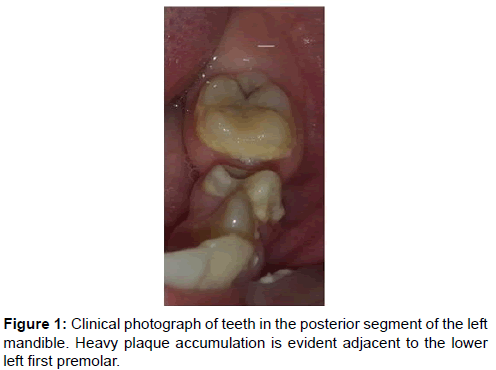
A 10-year-old Saudi female presented to King Khalid University, College of Dentistry, outpatient clinics, for evaluation of her mandibular left first premolar. The medical history was of no relevance. There was history of pain on biting, whilst her mother was anxious about some swelling of the gingiva adjacent to the offended tooth. Intraoral examination revealed deep occlusal caries with heavy plaque accumulation on the lower left quadrant indicating it as a non-chewing side [Figure 1]. Sensibility testing of the mandibular left first premolar was not responsive to both cold and electric pulp sensibility testing as compared to the remaining teeth in the lower left arch which showed a positive response. Periodontal examination revealed normal periodontal health around the offended tooth with no probing depths greater than 3 mm. The tooth revealed grade I mobility and the crown showed a deep carious lesion.
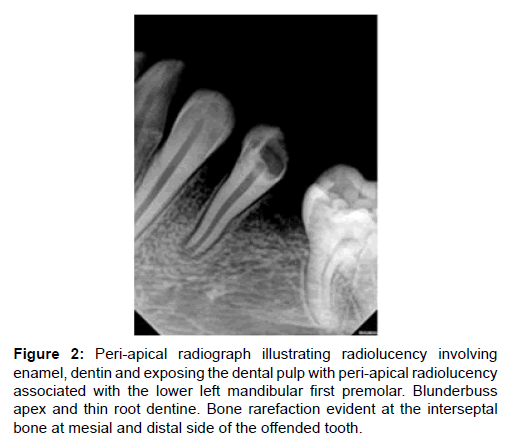
Radiographically, the mandibular left first premolar had; radiolucency involving enamel, dentin and exposing the dental pulp, an increased periodontal ligament space and apparent periapical radiolucency. The apex was Blunderbuss and dentinal wall were thin at the apical third of the root. Bone rarefaction was obvioust at the interseptal bone both mesial and distal sides of the offended tooth. Agenesis of the left second mandibular premolar was also evident [Figure 2].
Figure 2: Peri-apical radiograph illustrating radiolucency involving enamel, dentin and exposing the dental pulp with peri-apical radiolucency associated with the lower left mandibular first premolar. Blunderbuss apex and thin root dentine. Bone rarefaction evident at the interseptal bone at mesial and distal side of the offended tooth.
On the basis of the clinical and radiographic examination, the tooth was diagnosed as being necrotic with acute apical periodontitis which was a result of untreated dental caries and consequent pulpal involvement. Regenerative endodontic procedure was planned considering the age of the child, immaturity of the root apex, the thin root dentin, apical radiolucency and the rarefied interseptal bone. The primary goal was to promote matureogenesis of the root and healing of the periradicular and interseptal lesion.
Detailed information regarding the benefits, hazards, possible side effects and other possible treatment alternatives were offered for the child’s legal guardian and a written informed consent was obtained.
Local anaesthesia using 2% lidocaine with vasoconstrictor was administered and rubber dam isolation achieved.
Access cavity was prepared; a wide single canal was detected. Working length was estimated with a periapical radiograph taken with a size 15 K-file (Sybron Endo, Orange, CA, USA) inserted inside the canal.
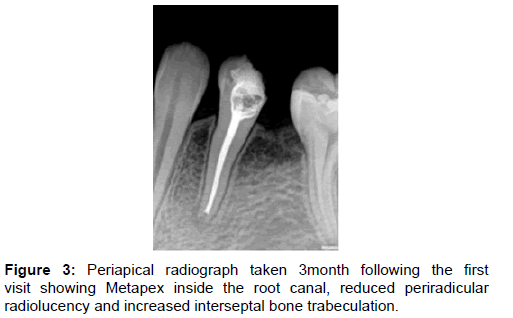
The canal was minimally instrumented and copiously irrigated with 20ml of 1.5% sodium hypochlorite followed by 17% EDTA. This was followed by dryness of the canal using paper points then calcium hydroxide with iodoform paste (Metapex) was used as dressing and tooth temporary restored with Glass Ionomer Cement Fuji IX (GC, IL, USA). Next recall visit was scheduled three weeks from the first appointment. However, patient failed to attend her appointment and came after 3 months instead. Patient reported no symptoms following the first appointment and pain disappeared completely. Therefore, the second visit was initiated; a periapical radiograph was taken and showed Metapex was in place with good apical and coronal adaptation [Figure 3].
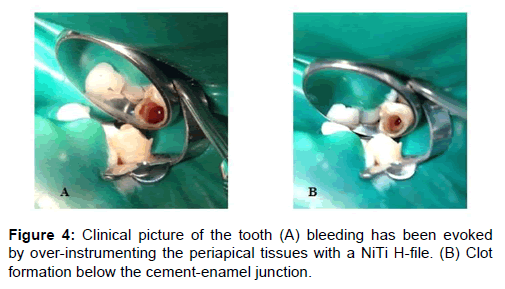
A 3% mepivacaine without a vasoconstrictor was used in order to facilitate intracanal bleeding. Under rubber dam isolation, bleeding was evoked by over-instrumenting the canals beyond the apical foramen to allow the influx of blood containing mesenchymal stem cells from periapical tissues to the root canal space using a NiTi H-file (Dentsply Tulsa Dental, TN, USA). Then blood clot formation was initiated by applying a damped cotton pellet to canal orifice for 15 minutes to produce a natural scaffold for the regenerative procedure [Figures 4A and 4B].
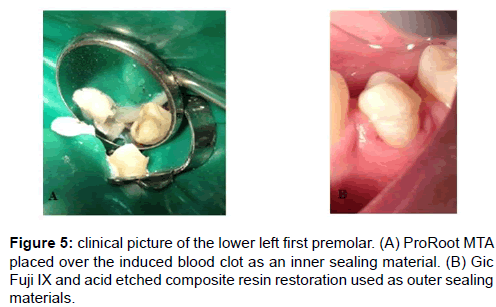
Access cavity was then sealed with an inner layer of 2 mm of ProRoot white MTA (Dentsply Tulsa Dental, TN, USA) using an amalgam carrier (CF-II® Hu-Friedy, USA) and a Buchannan Plugger (Sybron Endo, Orange, CA, USA) and an outer layer composed of GIC Fuji IX and an acid etched composite resin restoration [Figures 5A and 5B].
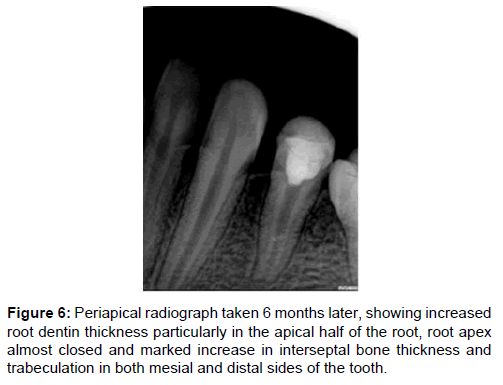
Patient was recalled six months later and reported no clinical symptoms, the tooth was functioning efficiently and periapical radiograph showed increased root dentin thickness particularly in the apical half of the root, root apex almost closed and marked increase in interseptal bone thickness and trabiculation in both mesial and distal sides [Figure 6].
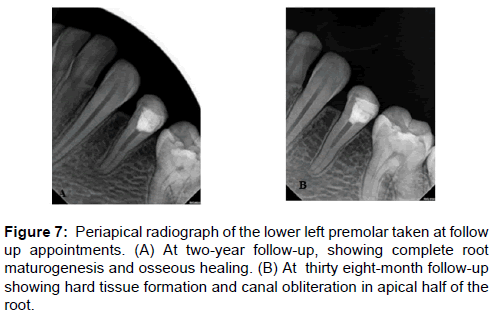
The tooth was clinically and radiographically followed up for thirty-eight-month. Patient was recalled at year two and three for clinical and radiographic evaluation. The tooth was clinically normal and a positive response was found when cold test was used (Endo-frost, Roeko, UK). Radiographic evaluation showed root maturogenesis and osseous healing; increased width of root dentine which was particularly evident at the apical half, slight lengthening of the root, apex was completely closed and radiopaque tissues were noticeable in the root canal space. Complete osseous healing was evident in the apical and interseptal bones [Figures 7A and 7B].
Conclusion
In conclusion, the authors consider revascularization procedures as an appropriate treatment for necrotic immature permanent teeth with apical periodontitis and/or associated bone defects, which not only result in tooth maturogenesis, but can also promote bony healing. However, case reports on endodontic regeneration have used varying treatment protocols and further clinical trials are required to assess the overall outcomes of the procedures.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Foundation A. Endodontics Colleagues for Excellence in Regenerative Endodontics, M. Cover artwork: Rusty Jones, Inc, Editor. 2013, American Association of Endodontists.
- Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: Case report and review of the literature. Pediatr Dent. 2007;29:47-50.
- Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: New treatment protocol? J Endod. 2004;30:196-200.
- Rafter M. Apexification: A review. Dent Traumatol. 2005;21:1-8.
- Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17:185-187.
- Chen MH, Chen KL, Chen CA, Tayebaty F, Rosenberg PA, Lin LM. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. International endodontic journal. 2012;45:294-305.
- Shabahang S, Torabinejad M, Boyne PP. A comparative study of root-end induction using osteogenic protein-1, calcium hydroxide, and mineral trioxide aggregate in dogs. J Endod. 1999;25:1-5.
- Ostby BN. The role of the blood clot in endodontic therapy: An experimental histologic study. Acta Odontol Scand. 1961;19:324-353.
- Rule DC, Winter G. Root growth and apical repair subsequent to pulpal necrosis in children. Br Dent J. 1966;120:586-90.
- Rui YD, Shun-pan G, Cheung J. Pulp revascularization of immature teeth with apical periodontitis, aclinical study. J Endod. 2009;35:745-749.
- Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: A case series. J Endod. 2008;34:876-887.
- Reynolds K, Johnson JD, Cohenca N. Pulp revascularization of necrotic bilateral bicuspids using a modified novel technique to eliminate potential coronal discolouration: A case report. Int Endod J. 2009;42:84-92.
- Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, et al. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. International Endodontic Journal. 1996;29:125-130.
- Gordon T, Ranly D, Boyan B. The effects of calcium hydroxide on bovine pulp tissue: Variations in pH and calcium concentration. J Endod. 1985;11:156-160.
- Schroder U, Granath L. Early reaction of intact human teeth to calcium hydroxide following experimental pulpotomy and its significance to the development of hard tissue barrier. Odontology. 1971;22:379-395.
- Hargreaves KM, Diogenes A, Teixeira FB. Treatment options: Biological basis of regenerative endodontic procedures. Pediatr Dent. 2013;35:129-140.
- Das S, Das A, Murphy R. Experimental apexigenesis in baboons. Endod Dent Traumatol, 1997;13:31-35.
- Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis: A clinical study. Journal of Endodontics. 2009;35:745-749.
- Petrino JA, Boda KK, Shambarger S, Bowles WR, McClanahan SB. Challenges in regenerative endodontics: a case series. Journal of endodontics. 2010;36:536-541.
- Chueh LH, Huang GT. Immature teeth with periradicular periodontitis or abscess undergoing apexogenesis:a paradigm shift. J Endod, 2006;32:1205-1213.
- Cotti E, Mereu M, Lusso D. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: Report of a case. J Endod. 2008;34:611-616.
- Lovelace EA. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod. 2011;37:133-138.
- Tittle K. Apical closure induction using bone growth factors and mineral trioxide aggregate. J Endod. 1996;22:198.
- Torabinejad M, Parirokh M. Mineral trioxide aggregate: A comprehensive literature review--part II:leakage and biocompatibility investigations. J Endod. 2010;36:190-202.
- Wang X, Thibodeau B, Trope M, Lin LM, Huang GT. Histologic characterization of regenerated tissues in canal space after the revitalization/revascularization procedure of immature dog teeth with apical periodontitis. Journal of Endodontics. 2010;36:56-63.
- Yamauchi N, Yamauchi S, Nagaoka H, Duggan D, Zhong S, Lee SM, et al. Tissue engineering strategies for immature teeth with apical periodontitis. Journal of endodontics. 2011;37:390-397.
- Huang GT, Sonoyama W, Liu Y, Liu H, Wang S, Shi S. The hidden treasure in apical papilla: the potential role in pulp/dentin regeneration and bioroot engineering. Journal of Endodontics. 2008;34:645-651.
- Heithersay G. Stimulation of root formation in incompletely developed pulpless teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1970;29:620-630.
- Lin L, Shovlin F, Skribner J, Langeland K. Pulp biopsies from the teeth associated with periapical radiolucency. Journal of Endodontics. 1984;10:436-448.
- Ritter AL, Ritter AV, Murrah V, Sigurdsson A, Trope M. Pulp revascularization of replanted immature dog teeth after treatment with minocycline and doxycycline assessed by laser Doppler flowmetry, radiography, and histology. Dental Traumatology. 2004;20:75-84.
- Shah N, Logani A, Bhaskar U, Aggarwal V. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: A pilot clinical study. Journal of endodontics. 2008;34:919-925.
- Thomson A, Kahler B. Regenerative endodontics--biologically-based treatment for immature permanent teeth: A case report and review of the literature. Aust Dent J. 2010;55:446-452.
- Huang GT. A paradigm shift in endodontic management of immature teeth: Conservation of stem cells for regeneration. J Dent. 2008;36:379-386.
- Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134-137.
- Law AS. Considerations for regeneration procedures. Pediatr Dent. 2013;35:141-152.
- Kahler B, Mistry S, Moule A, Ringsmuth AK, Case P, Thomson A, et al. Revascularization outcomes: a prospective analysis of 16 consecutive cases. Journal of endodontics. 2014;40:333-338.
- Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. Journal of Endodontics. 2009;35:1343-1349.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.