Multiple Sclerosis in a Nigerian Alcoholic Male: A Case Report from Enugu, South East Nigeria
- *Corresponding Author:
- Dr. Ikenna O Onwuekwe
Neurology Unit, Department of Medicine, University of Nigeria Teaching Hospital, P.M.B. 01129 Enugu, Nigeria.
E-mail: ikenna.onwuekwe@unn.edu.ng, onwuekweio@yahoo.com
Date of Received :7/10/2010
Date of Accepted :12/11/2010
Available Online :12/12/2010
Abstract
Background: Multiple sclerosis is a rare neurological disorder in black Africans. In Nigeria it had been difficult to confirm suspected cases due to the paucity of diagnostic facilities. The availability of magnetic resonance imaging has enabled an increased confidence in making the diagnosis.
Method: This is a case report of a 40- year old Nigerian farmer of the Igbo ethnic group living in a rural community in Enugu who presented with clinical features suggestive of multiple sclerosis. Though the patient had a significant history of alcohol consumption, he had clinical and magnetic resonance imaging features diagnostic of multiple sclerosis.
Results: A 40-year old male farmer presented to the Neurology Clinic of the University of Nigeria Teaching Hospital Enugu in January 2010 with a 10-year history of recurrent episodes of weakness of the legs. Each episode was sudden, affected either limb alternately, was associated with paraesthesiae and would resolve spontaneously after a few days or weeks without any intervention. Over the years he became unable to walk. The sphincters and vision were unaffected. A week prior to presentation he developed tremors of the hands with disorientation. The patient exhibited confabulation and had flaccid quadriparesis with glove and stocking sensory loss. Spinal fluid protein was raised and there were classic periventricular and intracerebral white matter hyper-intensities on magnetic resonance imaging.
Conclusion: This report of a case of multiple sclerosis suggests a need for clinicians in Africa to increase their index of suspicion in probable clinical scenario especially where magnetic resonance imaging exists.
Keywords
Multiple sclerosis, male, South- East Nigeria.
Introduction
Multiple sclerosis is a chronic demyelinating disease with protean manifestations that is believed to be uncommon in tropical countries including Nigeria. The non-availability of magnetic resonance imaging (MRI) in many Nigerian health institutions has made definitive diagnosis of suspected cases more difficult.
A case of multiple sclerosis diagnosed in a Nigerian male alcoholic is hereby presented. The clinical diagnosis was greatly aided by the availability of facilities for MRI in Enugu, South East Nigeria.
Case Summary
B.E is a 40- year old subsistent farmer living all his life in Eha-Alumona, a rural community in Enugu state. He presented to the Neurology Clinic on the 2nd of February 2010 with complaints of recurrent difficulty with walking of 10 years duration as well as fever and tremors of the limbs of one week duration.
His problems started about 10 years ago when he developed weakness in the left lower limb, which worsened progressively over days. He was able to walk though with support. There was associated paraesthesiae in the limb. There was no history of trauma, cough, or contact with a person with chronic cough, and no band like sensation. These symptoms resolved spontaneously after a few weeks. He remained stable until about a year later when he experienced a recurrence of weakness in the same limb and now involvement of the right upper limb with poor hand grip associated with paraesthesiae too. Again, the weakness lasted a few weeks and resolved.
This pattern of episodic weakness, at varying intervals, was to continue for the next 10 years involving the right upper limb and the left lower limb which would resolve without treatment.
About 6 weeks prior to presentation, there was recurrence of progressive weakness in the limbs earlier affected, with the right lower limb additionally involved for the first time. There was associated paraesthesiae, which involved the feet and hands. The weakness was now so profound that the patient was no longer able to ambulate. There was no sphincteric involvement, blurring of vision, double vision, eye pain, vertigo, neck pain, swallowing or speech difficulty. For these new problems he resorted to taking herbal concoctions without relief.
A week prior to presentation he developed high grade fever without chills and rigor.
There were no significant associated symptoms and he had to be admitted in a hospital for about 5 days before being referred to this centre. It was during this period that he noticed coarse tremors of his limbs associated with confusion and irrational speech.
He had taken alcohol in excess for more than 10years with a preference for local gin and spirits as well as beer. Often drunk, he had felt a need to cut down his alcohol intake. The tremor and confusion commenced after patient did not have access to alcohol during the period of his hospitalization.
There was no history of passage of dark tarry stools, altered sleep pattern, easy bruising, leg swelling, or abdominal swelling. Patient had gradually lost weight since the onset of symptoms and he was actually referred because of excessive coarse tremors of the body.
His past medical history and family history were unremarkable except as mentioned above. He had been married to one wife for six years but had no children yet. He also smoked about 8-10 cigarettes/day (10 pack year). He had worked as a peasant farmer for over 10yrs ago and was forced to stop due to the difficulty in walking. His relatives take care of the monetary needs of his family.
Physical examination revealed an emaciated and unkempt middle-aged man, conscious but confused, mildly pale, with coarse tremors of the hands and feet. He was febrile (T= 39.4oC), not jaundiced, acyanotic and had no peripheral lymphadenopathy, digital clubbing or leg oedema. There was no gynaecomastia.
He was confabulating. There was no meningeal irritation and no obvious cranial nerve deficit. He had flaccid mild quadriparesis with proximal muscles more affected than distal muscles. There was global hypo-reflexia and the plantar responses were flexor. There was sensory loss in a glove and stocking distribution (up to the elbows in the upper limbs and above the knees in the lower limbs). He had a high stepping gait. Cerebellar functions appeared intact
The abdomen had female pattern of hair distribution but no superficial distended veins were observed. There was non- tender hepatomegaly of 15cm span in the midclavicular line with a smooth surface. There was no splenomegaly or ascites.
He had a pulse rate of 84/min, normal volume and regular without arterial wall thickening. The blood pressure was 100/70mmHg supine. The rest of the cardiovascular examination system was normal. Save for the finding of hair loss on the legs with shiny atrophic skin, the rest of the systemic examination was normal.
He was admitted into the medical ward and managed as case of alcoholism with complications of Wernicke‟s encephalopathy, peripheral neuropathy and alcoholic liver disease. A possibility of multiple sclerosis was considered as well. Investigations were requested for including brain MRI, lumbar puncture for CSF studies, blood gamma glutamyl transferase assay, serum proteins, liver function test, abdominal ultrasound, retroviral screening, serum electrolytes, blood urea and creatinine, lipid profile, urine analysis and culture, complete haemogram including ESR. Some of his drug regimen included tablets of thiamine hydrochloride 50 milligram three times a day, chlordiazepoxide 10 milligram three times a day, intravenous ceftriaxone 1gram 12- hourly, tablets. Vitamin E 1000IU once day, tablets. Vitamin C 400 milligram three times a day. Necessary dietary modifications were made and physical therapy commenced.
Over the next few days the tremors subsided and the sensorium normalised. By the second week on admission, he had regained full power in the upper limbs and could walk with his legs. Patient was counselled on the need to stop taking alcohol and was discharged in February 2010 to be followed up in the out-patient clinic but has yet to attend since then.
Results of Investigations
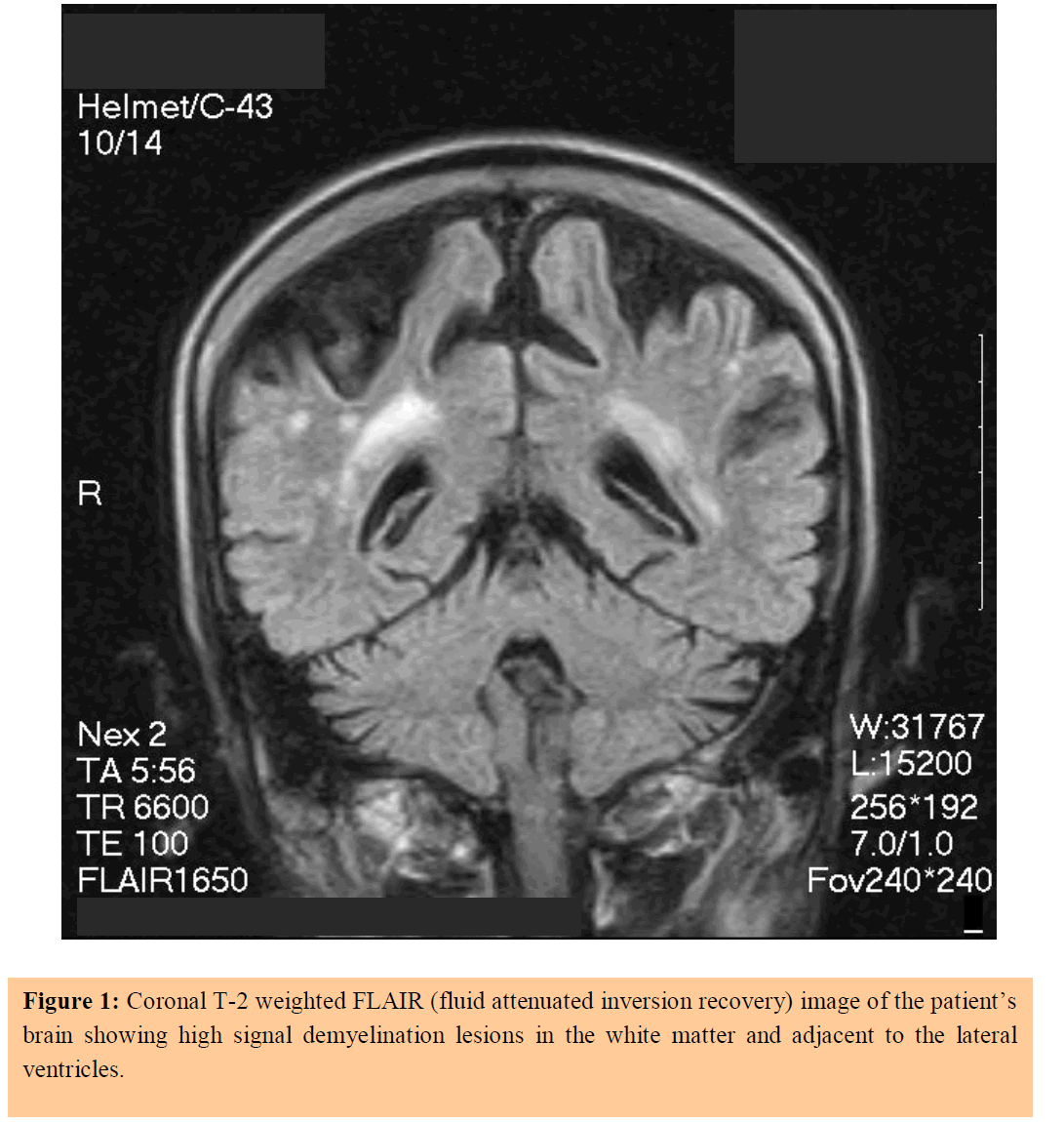
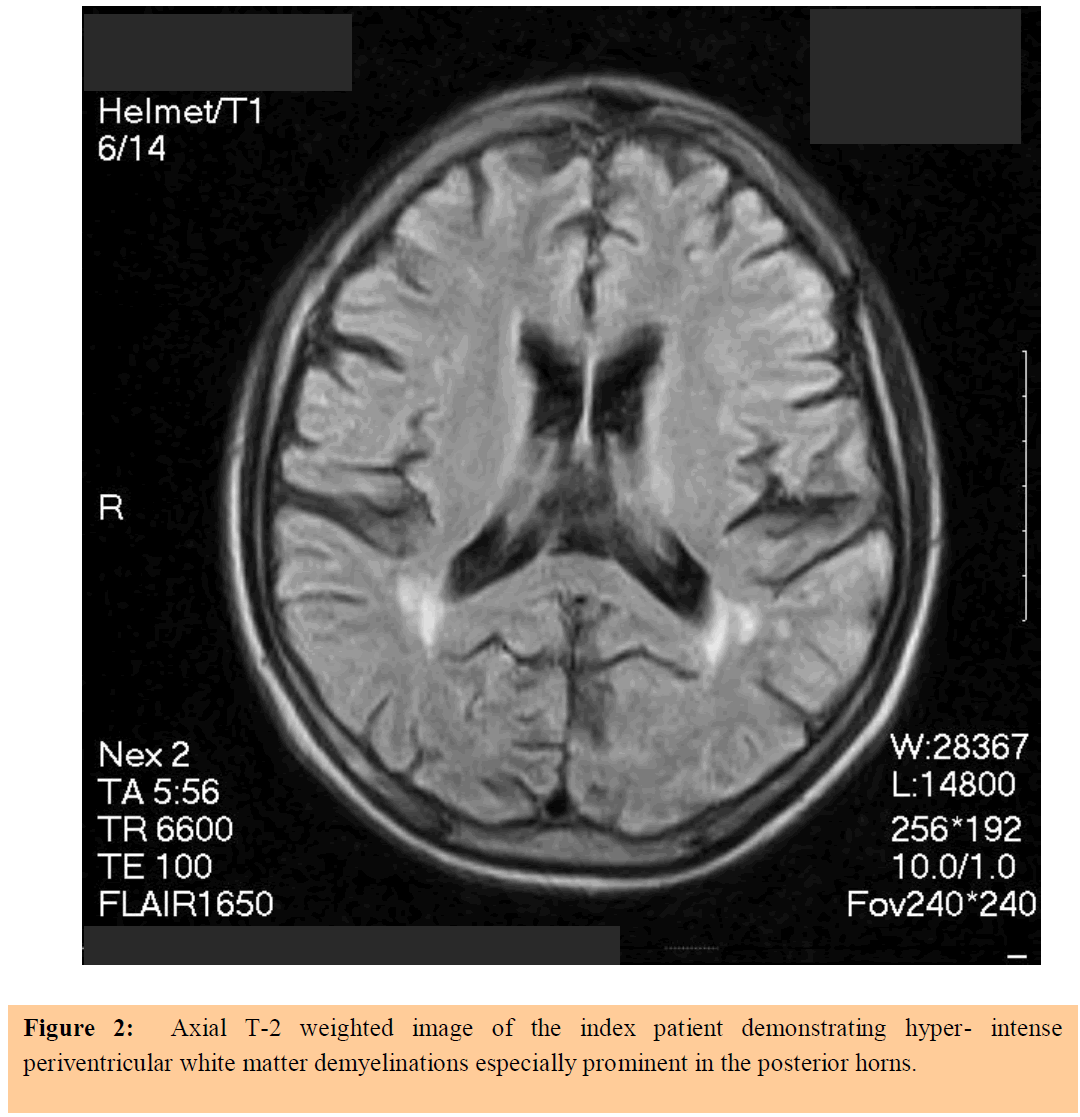
1. Brain MRI: Multiple small rounded plaques in both hemisphere with periventricular distribution and involving the corpus callosum that have slightly high signal intensity in T2 but marked high signal intensity in FLAIR. These are consistent with multiple sclerosis (see figures 1 and 2).
2. Serum protein: Total protein 68g/dl, albumin 29g/dl, globulin 39g/dl.
3. Haemogram: Mild anaemia with haemoglobin of 8.4g/dl, normal white cell count of 7.9x109/L (N59%, L41%), normal platelet count of 153x109/L, elevated ESR of 44mm/1st hr, abnormal peripheral blood film showing hypochromasia (++) and target cells (+).
4. Serum chemistry: Normal results.
5. Lipid profile: Normal results.
6. Urine culture yielded growth of klebsiella spp. >105 with sensitivity to ceftriaxone.
7. Liver function test: Normal results excepting elevated alanine transaminase of 34IU/L.
8. Abdominal ultrasound: Enlarged liver of 16.5cm span with irregular margins and coarse echotexture. It harbors no nodules or lesions within. The portal vessels are within normal dimensions. Normal kidneys and spleen. No ascites. Features suggest early cirrhotic changes.
9. HIV screening was not reactive
10. Cerebrospinal fluid protein was increased with normal cell count.
Discussion
Multiple sclerosis is also known by the term disseminated sclerosis because the clinical features of this demyelinating disease which affects the central nervous system (and spares the peripheral nervous system) are typically disseminated in time and space.[1] The condition is more prevalent in Caucasians than in blacks.
The rarity of multiple sclerosis in blacks especially Africans is well documented. However blacks who live in those countries with very high incidence tend to have the disease more than those resident in Africa suggesting an environmental role in the aetiology.[1] This environmental contribution is also apparent with the increased incidence of MS noted in countries with higher latitudes and colder climates, regardless of ethnicity.[2] A viral infection has been implicated in some cases though the evidence remains tenuous. [2]
Much of the diagnosis of multiple sclerosis is made based on the typical clinical features which commonly have a relapse-remission pattern. Though most sufferers describe episodes of spontaneous remissions, there tends to be a degree of residual neurological deficit with each attack which culminates in a chronic debilitating state with fixed neurological deficits, progressive disability and eventual death.
Though there are several criteria for the diagnosis of multiple sclerosis which suggest three levels of diagnosis; possible, probable and definitive, it must be remembered that these do not replace sound clinical judgment.[1] Numerous electrophysiological tests may assist in some cases; magnetic resonance imaging (MRI) has become extremely helpful in confirming a diagnosis. Examination of the cerebrospinal fluid in MS usually shows an increase in protein, lymphocytosis and the presence of oligoclonal bands (the latter in 90% of cases).
The index patient presented with neurological features that emanated at various times and in various regions of the body over a 10 year period culminating in quadriparesis. Though there was no visual or sphincter association which may have been expected, the absence of these is insufficient to invalidate the diagnosis. The finding of elevated CSF protein was further evidence for MS (it was not possible to check for oligoclonal bands at this centre) and whatever doubts there could have been was eliminated by the classic radiologic features evident on the patient‟s brain MRI results (see figures 1 and 2). It must be emphasised that diagnostic criteria cannot replace sound clinical judgement.[1]
There has been no published report of a case of multiple sclerosis in South East Nigeria with such clinical and radiologic correlations. This patient represents the first case. His heavy and chronic alcohol consumption with toxic effects on the peripheral nerves and liver probably accounts for features not in keeping with MS such as the glove and stocking sensory loss / high steppage gait and hepatomegaly respectively. Hepatomegaly could be the result of fatty liver or early cirrhosis as suggested by the ultrasound.
In South South Nigeria though, a case of MS in a 41- year old University lecturer with the locked-insyndrome had been reported.[3] Unfortunately the patient did not have the benefit of either a CSF examination or brain MRI test. Some of the close differentials of multiple sclerosis are described in table 1.[4] It can be readily appreciated that none of these can account for the index patient‟s clinical and radiologic features.
Multiple sclerosis is a rare demyelinating disease in black Africans. This case report of a Nigerian male with clinical and radiological features consistent with a diagnosis of multiple sclerosis suggests the need for increased awareness as well as a high index of suspicion among clinicians practicing in Africa. The availability of magnetic resonance imaging services will further augment diagnosis in certain cases.
References
- Hauser SL and Goodkin DE. Multiple sclerosis and other demyelinating diseases. In: Fauci AS, Braunwald E, Isselbacher KJ, Wilson JD et al. (Eds). Harrison‟s Principles of Internal Medicine. 14th ed. New York: McGraw-Hill; 1998; 2409 -2419.
- Victor M and Ropper AH. Multiple sclerosis and allied demyelinating disease. Adams and Victor‟s Principles of Neurology. 7th ed. New York: McGraw Hill; 2001; 954 -982.
- Imananagha KKE and Asindi AA. Locked in Syndrome in a Nigerian male with Multiple Sclerosis. A case report and literature review. The Pan African Medical Journal. 2008; 1:4.
- Rolak LA and Fleming JO. The differential diagnosis of multiple sclerosis. The Neurologist 2007; 13: 57–72.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.