Myomectomy for Retained Placenta Due to Incarcerated Fibroid Mass
- *Corresponding Author:
- Dr. Mbamara SU
P.O. Box 354, Amaraku, Imo State, Nigeria.
E-mail: Kensunny30@yahoo.co.uk
Abstract
Retained placenta is one of the most common complications of preterm delivery and/or mid‑trimester miscarriage. It is an important cause of increased maternal morbidity and sometimes mortality especially in developing countries. It is associated with several complications that could be tasking to the facility and of great challenge to the obstetrician. Here we present a very rare event in obstetrics which is retained placenta due to incarcerated, posteriorly‑sited fibroid that was successfully managed with myomectomy.
Keywords
Fibroid, Myomectomy, Placenta, Retained
Introduction
Retained placenta is a significant cause of maternal morbidity and mortality throughout the developing world with a case mortality rate of nearly 10% in rural areas. [1,2] It is associated with complications which may have immediate and remote effects on the woman’s reproductive life. Fibroid mass as a cause of retained placenta is extremely rare but a worrisome and life threatening complication. We present a patient who had mid-trimester miscarriage, complicated by retained placenta due to incarcerated uterine fibroid masses and had myomectomy.
Case Report
A 29-year-old Para 0+2 Nigerian woman was admitted through the gynaecology emergency room with pre-viable rupture of membrane of 15 min duration at 19 weeks of gestation and multiple uterine fibroids. There was no uterine contraction or bleeding per vaginam.
She booked for prenatal care in Abuja Clinics Limited on the May 6, 2013 at a gestational age of 13 weeks. Her date of last menstrual period (LMP) was February 15, 2013 and her expected date of delivery (EDD) was November 22, 2013. She had no complaint at booking. She suffered from severe malaria prior to booking which was treated with tablet chloroquine elsewhere by a pharmacist. The only significant finding at booking was the symphysio-fundal height which was greater than the estimated gestational age. At booking her symphysiofundal height was 30 weeks which was greater than expected at 13 weeks of gestation.
She had a spontaneous miscarriage in the year 2012 at 8 weeks gestation. There was nothing significant in her past medical and surgical history. Her blood group was A Rhesus D positive and her haemoglobin genotype was AA. Haematocrit was 27.8%, (Haemoglobin level – 9.3 mg/dl). She received iron and folic acid supplementation, intermittent preventive treatment against malaria and a dose of tetanus toxoid injection.
At the emergency room she was anxious-looking, her pulse rate was 90 beats/min and her blood pressure was 150/90 mmHg. Speculum examination revealed a pool of fluid in the vagina although the cervix was visualized. The posterior fornix was filled with nodular masses. Urgent ultrasound scan done revealed anteverted, bulky and gravid uterus which harboured a single, viable intra-uterine fetus in atransverse lie. Fetal cardiac activity was observed with no evidence of fetal movement throughout the scan duration. Multiple well circumscribed mixed echogenic masses were seen co-existing with the gestation. The largest mass measured 13.2 cm × 10.8 cm and it covered the whole lower segment of the uterus thereby impairing the visualization of the cervix. Other nodules which measured 7.2 cm × 6.9 cm located at the antero-fundal aspect of the uterus and 4.2 cm × 3.3 cm (located within the mid anterior myometrium were noted. The placenta was anterior and not low lying with grade 0 maturation. Liquor volume was markedly reduced. Both adnexae were normal. There was no fluid seen in the pouch of Douglas. The estimated GA was 18 weeks 3 days while the EDD was 09/11/2014 ± 2 weeks. An impression of single viable intra-uterine fetus at 18 weeks + 3 days GA with severe oligohydramnios was made. Her packed cell volume was 22% and urinalysis was normal.
The couple was counselled extensively on the problems, management options, prognosis and possible complications by the Obstetrician, Paediatrician and Medical Counsellor. They opted for conservative management. She was commenced on antibiotics-erythromycin, and metronidazole. About 16 h later the couple gave consent for the termination of the pregnancy. Uterine contractions were stimulated using intravaginal 400 mcg of misoprostol tablets. Few hours later she expelled the fetus but the placenta was retained. Syntocinon infusion was set up. After continuous cord traction failed an attempt was made to remove the retained placenta in the theatre under general anaesthesia but this failed too because the cervix could not be visualized.
Ultrasound and Doppler ultrasound showed a completely separated placenta that was retained intrauterine and the uterine cervix was still not visualized. The couple and their relatives were counselled extensively and repeatedly on the need to do a myomectomy to enable the obstruction to be relieved and the placenta delivered. The placenta remained intra-uterine for over 12 h before they gave their consent for myomectomy. Four units of blood were grouped and cross-matched. A unit was transfused pre-operatively and another one intra-operatively.
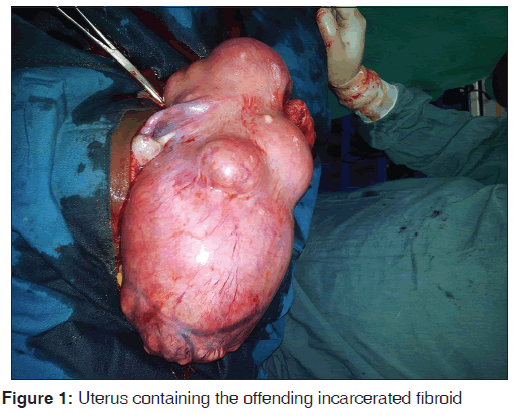
Intra-operative findings were 15 number, variously sized, nodular fibroids masses intramural and subserosal in location with a total weight of 2.5 kg. The biggest fibroid which measured 15 cm × 20 cm × 15 cm and weighed 1.5 kg was located posteriorly and it filled the pouch of Douglas [Figure 1]. Some of the fibroid masses had undergone red degeneration. The placenta fell into the vagina with the enucleation of the posterior fibroid. The weight of the placenta was 0.25 kg. The endometrium was not breached. The fallopian tubes and ovaries were normal. Foley’s catheter was used to reduce blood loss during the surgery. The estimated blood loss was 500 ml. Postoperative management included intravenous fluids, blood transfusion, antibiotics and analgesics. She was discharged on the fifth postoperative day to continue further management as an out-patient. She had made three further clinic visits with no complaints. She recovered completely with no complications and her menstrual periods returned 6 weeks postoperation and had remained normal. She did give her consent for this case to be published.
Discussion
Retained placenta is one of the common clinical problems encountered in obstetric practice the world over. It is a significant cause of maternal morbidity and mortality throughout the developing world with a case mortality rate of nearly 10% in rural areas. [1-3] Varied incidence(s) of retained placenta has been documented. [1,2] Depending on the population studied and the definition used, it is estimated that between 0.01 and 6.3% of all vaginal deliveries are complicated by retained placenta. [1-3] There is no local guideline or worldwide consensus on the length of time after which the diagnosis of retained placenta should be made or intervention initiated. The World Health Organization (WHO) recommends a waiting time of 60 min. [4] In this case presented, the diagnosis of retained placenta was made 1 h after the foetus was expelled and manual extraction under general anaesthesia was attempted after administration of continuous parenteral syntocinon for another hour. Although retained placenta has been noted to be commoner in developed nations but it is associated with higher morbidity and mortality in developing nations. [1,2] This is because access to appropriate, well-equipped medical facilities and evenly distributed skilled manpower allowing for timely and proper surgical management/intervention is either lacking or inadequate in the less developed countries.
The three basic pathophysiologic types of retained placenta are placenta adherence, morbidly adherent placenta and trapped placenta. In placenta adherence there is mild adherence of the placenta to the uterus but this is easily separated manually in contrast to morbidly adherent placenta in which there is invasion of the uterine myometrium by the placental tissue. In trapped placenta, the placenta is completely separated from uterus but the placenta fails to be extracted due to mechanical obstruction. The common causes of trapped placenta are partial closure of the cervix and/or contracted lower uterine segment. Trapped placenta in a septate uterus has also been reported. [5,6] In this case however, the placenta was entrapped by incarcerated uterine fibroid masses [Figure 1] which is actually a very rare phenomenon.
Uterine leiomyoma (fibroids) is a common benign uterine tumour affecting women of reproductive age. It is noted in about 4–5% of pregnancies and is usually asymptomatic. It is about six times (6×) more common in Blacks than Caucasians. There are lots of controversies surrounding the effect of fibroid on pregnancy and also the effect of pregnancy on fibroid. Uterine fibroids are usually asymptomatic both in pregnant and nonpregnant women. In pregnancy it may present with symptoms of complications. These complications include but not limited to anaemia in pregnancy due to menorrhagia before the onset of pregnancy, symphysio-fundal height being greater than estimated gestational age, abdominal pain as a result of necro-biosis (red degenerationor torsion of pedunculated fibroid mass, abnormal lie/presentation. In the third stage labour and in peurperium, it has been associated with both primary and secondary postpartum haemorrhage (PPH).
Retained placenta has been documented to be commoner in women with fibroids. [7] Other independent risk factors for retained placenta include history of previous retained placenta, preterm delivery and previous miscarriage. [8] Intravenous oxytocin administered during or after delivery has not been shown to increase the incidence of PPH as a result of retained placenta and or length of third stage of labour. [9]
The diagnosis of fibroids was made before the onset of her first pregnancy and she suffered some of the aforementioned complications. The fear of surgery itself and the possible effects of surgery on her reproductive function made her to decline myomectomy which was offered to her initially before the onset of the index pregnancy. The fear of surgery among African women has been corroborated in other reports. [10] The mainstay of the diagnosis of fibroids and retained placenta is ultrasound scan. Ultrasound scan is reliable, readily available, cheap and easy to interpret. Doppler ultrasound scan helps is to confirm the flow of blood to the placenta and document if the placenta is fully detached. Other modalities of diagnosis include computerized tomography scan, and magnetic resonance imaging.
It is our belief that the fibroids could be responsible for the mid-trimester pregnancy losses and also the cause of the retained placenta. The fibroid which was incarcerated in the pouch of Douglas pushed the cervix to the anterior pubic rami thereby preventing it from being accessed from the vagina. This made the extraction of the placenta impossible and made the attempted removal under anesthesia to fail. The fact that the placenta fell off on its own on the enucleation of the huge incarcerated posterior fibroid confirms the fact that it was responsible for the placenta retention.
Complications of retained placenta are PPH, puerperal sepsis/ infection uterine sub-involution, increased need for blood transfusion and complications arising from its management like urological injuries and fistula formation. Other possible complications/morbidities include infertility; amenorrhoea and hysterectomy. However none of these complications was noted in our patient. She received blood transfusion as a result of her low preoperative anaemic state.
The optimal management of retained placenta should involve early recognition of the women at risk, accurate preoperative diagnosis of retained placenta and its possible cause(s), detailed couple counselling and meticulous planning of intervention by a skilled and experienced obstetrician. Management is commonly by manual removal of placenta under general anaesthesia. Expectant management as an option has been described in the literature. [11] A large randomized controlled trial suggested that expectant management is not inferior to intra-umblical injection of saline solution with or without oxytocin for the management of retained placenta. [12]
Other management options include the use of misoprostol, glyceryl trinitrate, hysterotomy and hysterectomy. [1] Nitroglycerine has been described for the management of partial closure of the cervix or contracted lower uterine segment preventing placenta delivery. It is usually administered to relax the uterus and facilitate placental delivery. [12,13] Another option of management of persistent retained placenta not responding to conventional treatment is conservative management with methotrexate. [14]
None of these usual methods of treatment was helpful in the management of this patient. Continuous cord traction was not successful and manual removal under general anaesthesia was not feasible since the cervix was not accessible per vaginam. It was stretched and flushed to the anterior pelvic bones. Medical management was not applicable to her since the pathophysiology of the entrapped placenta is different.
She had myomectomy instead because the placenta was mechanically obstructed by the incarcerated fibroid mass. The placenta fell into the vagina by itself on the enuculeation of the offending fibroid mass confirming the fact that the placenta had completely separated previously but was held back by mechanical obstruction by the fibroid. The endometrial cavity was left intact to limit further complications and help preserve her fertility.
Myomectomy as a treatment for retained placenta is a very rare phenomenon as we did not find any other reported case in our literature search. It should be considered only after the less invasive methods have failed because of the risk of significant blood loss and even hysterectomy.
In conclusion, it is pertinent to note that uterine fibroid in pregnancy could be a rare cause of retained placenta hence the need for increased awareness. The diagnosis requires a very high index of suspicion and management requires great skill/dexterity because of the complications associated with performing myomectomy on a pregnant uterus.
References
- Weeks AD. The retained placenta. Best Pract Res Clin Obstet Gynaecol 2008;22:1103-17.
- Weeks AD. The retained placenta. Afr Health Sci 2001;1:36-41.
- Cheung WM, Hawkes A, Ibish S, Weeks AD. The retained placenta: Historical and geographical rate variations. J Obstet Gynaecol 2011;31:37-42.
- World Health Organization. Pregnancy, Childbirth, Postpartum and Newborn Care. A Guide for Essential Practice. 2nd ed. Geneva, Switzerland: WHO; 2006.
- Soltani H, Hutchon DR, Poulose TA. Timing of prophylactic uterotonics for the third stage of labour after vaginal birth. Cochrane Database Syst Rev 2010;8; Art no: CD006173.
- Endler M, Grünewald C, Saltvedt S. Epidemiology of retained placenta: Oxytocin as an independent risk factor. Obstet Gynecol 2012;119:801-9.
- Lee D, Johnson J. Hysterotomy for retained placenta in a septate uterus: A case report. Case Rep Obstet Gynecol 2012;2012:594140.
- Deckers EA, Stamm CA, Naake VL, Dunn TS, McFee JG. Hysterotomy for retained placenta in a term angular pregnancy. A case report. J Reprod Med 2000;45:153-5.
- Lee HJ, Norwitz ER, Shaw J. Contemporary management of fibroids in pregnancy. Rev Obstet Gynecol 2010; 3:20-7.
- Sunday-Adeoye I, Kalu CA. Pregnant Nigerian women’s view of cesarean section. Niger J Clin Pract 2011;14:276-9.
- Harvie RM. Retained Placenta; Expectant Treatment Successful. Can Med Assoc J 1924;14:65.
- Carroli G, Belizan JM, Grant A, Gonzalez L, Campodonico L, Bergel E. Intra-umbilical vein injection and retained placenta: Evidence from a collaborative large randomised controlled trial. Grupo Argentino de Estudio de Placenta Retenida. Br J Obstet Gynaecol 1998;105:179-85.
- Chedraui PA, Insuasti DF. Intravenous nitroglycerin in the management of retained placenta. Gynecol Obstet Invest 2003;56:61-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.