Perceived Indications, Safety and Efficacy of Perinatal Use of Traditional and Spiritual Remedies among Mothers of Under-Five Children in Kano, North-Western Nigeria
2 Department of Obstetrics and Gynaecology, Aminu Kano Teaching Hospital, Kano State, Nigeria, Email: idris_usman@buk.edu.ng
3 College of Health Sciences, Kaduna State, Nigeria, Email: ramla_mk@yahoo.com
4 Department of Applied Sciences, Kaduna Polytechnic, Kaduna State, Nigeria, Email: idris_usman@buk.edu.ng
Citation: Lawan UM, Takai IU, Abdullahi HM, Kamal RM, Umar H. Perceived Indications, Safety and Efficacy of Perinatal Use of Traditional and Spiritual Remedies among Mothers of Under-Five Children in Kano, North-Western Nigeria. Ann Med Health Sci Res. 2017; 7:10-15.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Herbal and spiritual remedies are increasingly being used in the management of perinatal conditions. Objectives: To determine the pattern of use of herbal and spiritual remedies during perinatal period, and the perceived indications, efficacy and safety of these remedies among mothers of under-five children in Kano. Subjects and Methods: A descriptive crosssectional design was used to study a random sample of 189 mothers. Data were analyzed using IBM SPSS statistics 22. The chi-square test and Fisher’s exact test were used for univariate analysis. Result: The means of respondents’ age and their number of children were 33.3 ± 9.2 years and 4.7 ± 2.6 respectively. Three-quarters of the mothers (76.2%) used herbal and/or spiritual remedies within the perinatal period, mostly orally (97.9%); 63.2% used them in combination with orthodox medicines. The main indications were maintaining good health during pregnancy (39.6%); easy labour and safe delivery (39.6%); and treatment of common ailments (28.5%). Majority believed that herbal (66.1%) and spiritual (70.9%) remedies are very effective on pregnancy related problems; 57.1% and 78.8% believed that herbal and spiritual remedies are very effective on problems of labour and pueperium respectively. Most believed that spiritual remedies are safe during pregnancy (94.2%) and in labour and pueperium (97.9%); and herbs are safe during labour and pueperium (91.0%). Conclusion: Health authorities in Nigeria should institutionalize structures for censoring, training, regulation of TM practice and safety of remedies used.
Keywords
Indications, Safety, Perinatal use, Traditional remedies, Northwestern Nigeria
Introduction
The use of herbal and spiritual medicines for prevention and treatment of diseases and ill health including disorders of pregnancy and childbirth is as old as the history of mankind. Herbs and herbal materials are naturally occurring plants with medicinal or preventive properties.[1] In the traditional African societies herbs are used in their raw or cooked forms without subjecting them to laboratory investigations for safety and efficacy, and are thus able to cause side effects and interactions. [1] Spiritual healing on the other hand is overcoming spiritual root causes of problems through faith-based actions or use of sacred as opposed to material things.[2] Both herbal and spiritual medicines are integral parts of traditional medicines.[3]
The use of herbal medicine (HM) is on the increase in many developing and industrialized countries.[4,5] It is known that between 65% and 80% of the world’s population use herbal medicines as their primary form of health care.[6,7] Among women in Africa, herbal and spiritual remedies are increasingly being used in the management of perinatal conditions especially in the rural communities due to easy access and low cost of therapy. [8,9] Pregnant women patronize herbal remedies for treatment of nausea and vomiting, low back pain, to support or terminate pregnancy, for anesthesia and also to prepare for labour or other unrelated health issues such as colds and respiratory illnesses, skin problems or to achieve good psychological health.[2,3,10,11] Herbal remedies are also used to protect the fetus from evil invitro and to have a healthy child.[12,13]
The perinatal period has been defined as “the period between 22 completed weeks of gestation and seven completed days after birth”.[14] It is the period of highest risk in the life time of a woman that if not properly managed may lead to the death of the fetus, mother or both. Despite the wide use of traditional medicines, standard guidelines on its use or evaluation of its efficacy or safety is still lacking especially in sub Saharan Africa where national policies and regulations on traditional medicines products, practices and practitioners are difficult to implement.[3,7,15] In the local Hausa communities of northern Nigeria most herbal medicines are considered polyvalent and their dosages are open. Through the lens of the health belief model developed by Hochbaum et al.[16] this study determined the pattern of perinatal use of herbal and spiritual remedies, and the perceived indications, efficacy and safety of these remedies among mothers of under-five children in Kano, northwestern Nigeria. Findings from this study will be useful to policy makers in understanding and packaging appropriate strategies and interventions to address the challenge. It will also add to empirical literature and provide baseline for further research. According to Jans and Becker, the model suggests that people’s beliefs about health problems, perceived benefits of action and barriers to action, and self-efficacy explain engagement (or lack of engagement) in health-promoting behavior.[17]
Materials and Methods
Settings
The study was conducted in Ungogo Local Government Area (LGA), one of the eight (8) metropolitan LGAs of the state. Ungogo settles 369,657 of the 9,383,682 projected population of Kano state according to the 2006 population census.[18] It has a lot of traditional settlements and a number of renown traditional healers that attract patronage from within and outside of Kano state.
Study design, subjects and sample size
We used a descriptive cross sectional design to study a random sample of 189 mothers of under five children that were resident in Ungogo LGA. Mothers of children more than five years of age and those resident outside Ungogo were excluded from the study. The sample size was determined using the Fisher’s formula for estimating minimum sample size for descriptive studies;[19] and the prevalence of herbal medicine use (84.7%) obtained from a similar study in Enugu, Nigeria.[20]
Sampling
A multistage sampling technique was used to select the participants. At first stage, Ungogo LGA was purposively selected from the 44 LGAs of Kano State because of its multiple traditional settlements and preponderance of renown traditional healers within its locality. At the second stage, one of the 11 wards of Ungogo LGA was randomly selected by drawing lot and the settlements therein were listed. This resulted in the selection of Rimin Gata ward. At the third stage, 50% of the listed settlements in Rimingata ward were radomly selected by simple balloting, and all the houses in the selected settlements were numbered giving a total of 2462 houses. Finally, the houses were selected by systematic sampling using a sampling interval of 13 obtained by dividing the number of houses (2462) by the required sample (189). From each selected house, an eligible mother was identified and administered the tool after obtaining her informed consent. The direction of movement for selecting the houses was determined by spinning a bottle and the house number that corresponded with a random number chosen between one and thirteen was used to identify the first house to be selected. Subsequent houses were identified by adding the sampling interval to the preceding household’s serial number. Where there were more than one eligible respondent in a house, one was selected using a simple random sampling by one time ballot. This was continued until the desired sample size was attained.
Instrument and method of data collection
A pre-tested interviewer administered semi-structured questionnaire with mostly closed ended questions was used for data collection. It was adapted and modified from the questionnaire used in a previous study on the prevalence and patterns of prenatal use of traditional medicine among women at selected Harare clinics.[21] The questionnaire consisted of (32) items subdivided into four sub-sections. The first subsection enquired about the respondent’s socio-demographic characteristics. The second section elicited the use of herbal and spiritual remedies among the mothers during the perinatal period. The third section sought about the mothers’ perceptions about indications for using the remedies and the fourth section sought about perceived efficacy and safety of using the remedies during perinatal period. The questionnaires were administered by four trained female interviewers after obtaining informed consent from the mothers.
Permission and ethical clearance for the study were sought and obtained from the health department of Ungogo LGA and ethical committee of Aminu Kano Teaching Hospital respectively. Data was collected in January/February 2015.
Data analysis
Data were analyzed using IBM SPSS statistics 22. Absolute numbers and simple percentages were used to summarize categorical variables whereas quantitative variables were summarized using means and standard deviation. The chi-square test and Fisher’s exact probability test were used for bivariate analysis involving categorical variables. A p-value <0.05 was considered statistically significant.
Results
Socio-demographic characteristics of the respondents
The respondents’ ages ranged from 17 to 49 years with a mean and standard deviation of 33.3 ± 9.2 years. Majority of the respondents were married (84.1%), Hausa/Fulani (95.2%), Muslims (98.9%), and had 5 to 12 children (49.7%). The mean number of the respondents’ children was 4.7 ± 2.6. Almost half of the respondents (43.4%) had Qur’anic education only while 47.6% had a form of formal education. More than half of respondents (58.2%) were traders, while 28.0% were unemployed [Table 1].
| Characteristic | Frequency (n=189) | Percentage (%) |
|---|---|---|
| Age group (Years) | ||
| 15-19 | 6 | 3.2 |
| 20-24 | 33 | 17.5 |
| 25-29 | 26 | 13.8 |
| 30-34 | 33 | 17.5 |
| 35-39 | 26 | 13.8 |
| 40-44 | 28 | 14.8 |
| 45-49 | 37 | 19.6 |
| No. children of Respondents | ||
| 1-4 | 95 | 50.3 |
| 5-12 | 94 | 49.7 |
| Marital status | ||
| Married | 159 | 84.1 |
| Widowed | 19 | 10.1 |
| Divorced | 11 | 5.8 |
| Religion | ||
| Islam | 187 | 98.9 |
| Christianity | 2 | 1.1 |
| Ethnicity | ||
| Hausa | 146 | 77.2 |
| Fulani | 34 | 18.0 |
| Yoruba | 3 | 1.6 |
| Others | 6 | 3.2 |
| Educational status | ||
| No education | 17 | 9.0 |
| Qur’anic only† | 82 | 43.4 |
| Primary | 38 | 20.1 |
| Secondary | 42 | 22.2 |
| Post-secondary | 10 | 5.3 |
| Occupations | ||
| Civil service | 8 | 4.2 |
| Trading | 110 | 58.2 |
| Artisanship | 18 | 9.5 |
| Unemployed | 53 | 28.0 |
*Other ethnic groups include Nupe and Kanuri; †Qur'anic education only refers to subjects that do not have any other form of education
Table 1: Socio-demographic characteristics of the respondents
Perinatal use of herbal and spiritual remedies
About three-quarters of the mothers, 144 (76.2%) used herbal and/or spiritual remedies at a stage or throughout their last perinatal period and beyond (pregnancy, childbirth and up to 6 weeks after delivery). About two-thirds of these mothers (63.2%) used the remedies in combination with orthodox medicines. Less than half 77 (40.7%) received advice on using the remedies: 51 (27.0%) by parents or close relatives; 23 (12.2%) from spouses; 2(1.1%) from friends/close associates and one (0.5%) from an Islamic scholar.
Majority of the 144 mothers that used herbal and spiritual remedies did so in different permutations and combinations as shown in Table 2. The remedies were commonly administered via the oral route (97.9%), and more than one-fifth used the remedies in the third trimester only (21.5%), but 27.1% and 23.6% used them throughout pregnancy and labour; and from pregnancy, through labour to postpartum period respectively as shown in Table 2. This study observed that perinatal use of herbal and spiritual remedies was significantly associated with the mother’s ethnicity (Fisher’s p=0.0007). Mothers from the Hausa/ Fulani ethnic groups were more likely to have used herbal or traditional remedies during the perinatal period [O.R(95% C.I)=13.08 (2.61; 65.55)] [Table 3].
| Frequency (n=144) | Percentage (%) | |
|---|---|---|
| Type of remedy used | ||
| *Holy water/washings of the sacred writing | 111 | 77.1 |
| *Incantations/prayers | 96 | 66.7 |
| *Unprocessed herbs | 97 | 67.4 |
| Packaged herbal product | 23 | 16.0 |
| Route administered | ||
| *Oral | 141 | 97.9 |
| *Topical | 42 | 29.2 |
| Intravaginal | 4 | 2.8 |
| Period of use | ||
| First trimester only | 4 | 2.8 |
| Second trimester only | 5 | 3.5 |
| Third trimester only | 31 | 21.5 |
| Labour only | 11 | 7.6 |
| Pueperium only | 3 | 2.1 |
| Throughout pregnancy | 17 | 11.8 |
| Pregnancy and labour | 39 | 27.1 |
| Pregnancy labour and pueperium | 34 | 23.6 |
*Multiple responses
Table 2: Perinatal use of herbal and spiritual remedies
| Perinatal use of Herbal and/ or Spiritual remedies | |||||
|---|---|---|---|---|---|
| Characteristics | Used (n=144) Freq (%) | Did not use (n=45) Freq (%) | Total (N=189) | Statistic (p-value) |
OR (95% C.I) |
| Age (Years) | |||||
| 15-34 | 76 (52.8) | 22 (48.9) | 98 | χ2=0.21 | - |
| 35-49 | 68 (47.2) | 23 (51.1) | 91 | (< 0.01) | |
| Ethnicity | |||||
| Hausa/Fulani | 142 (98.6) | 38 (84.4) | 180 | Fisher’s | 13.08 |
| Others | 2 (1.4) | 7 (15.6) | 9 | (< 0.001)* | (2.61; 65.55) |
| Marital status | |||||
| Currently married | 125 (86.8) | 34 (75.6) | 159 | χ2=3.25 | |
| Currently not married | 19 (13.2) | 11 (24.4) | 30 | (< 0.01) | |
| No. of respondents’ children | |||||
| 1-4 | 71 (49.3) | 24 (53.3) | 95 | χ2=0.22 | |
| 5-12 | 73 (50.7) | 21 (46.7) | 94 | (< 0.01) | |
| Educational status | |||||
| At least secondary | 38 (26.4) | 14 (31.1) | 52 | χ2=0.38 | |
| No secondary | 106 (73.6) | 31 (68.9) | 137 | (< 0.01) | |
| Employment status | |||||
| Unemployment | 37 (25.7) | 16 (35.6) | 53 | χ2=1.65 | |
| Gainfully employed | 107 (74.3) | 29 (64.4) | 136 | (< 0.01) | |
*Statistically significant
Table 3: Factors associated with the mothers’ perinatal use of herbal and spiritual remedies
Indications for use of herbal and/or spiritual remedies during perinatal period
More than one-third of the 144 mothers that used the remedies (39.6%) had multiple indications for doing so. Common indications highlighted were maintaining good health during pregnancy (39.6%), easy labour and safe delivery (39.6%) and treatment of common ailments like fever, diarrhoea, hypertension and high blood sugar (28.5%) as shown in Table 4.
| Indication | Frequency (n=144) | Percentage (%) |
|---|---|---|
| *Good health during pregnancy | 57 | 39.6 |
| Treatment of morning sickness | 9 | 6.3 |
| *Treatment of common ailments | 41 | 28.5 |
| Fetal wellbeing | 6 | 4.2 |
| *Easy labour/safe delivery | 57 | 39.6 |
| †Others | 13 | 9.0 |
†Others include treatment for abnormal placental position, protection against evil spirits, adequate flow of breast milk, support involution of uterus and strengthen perineal muscles; *Multiple responses
Table 4: Perceived indications of using herbal and/or spiritual remedies during perinatal period
Perceptions of the mothers about the efficacy of herbal and spiritual remedies during perinatal period
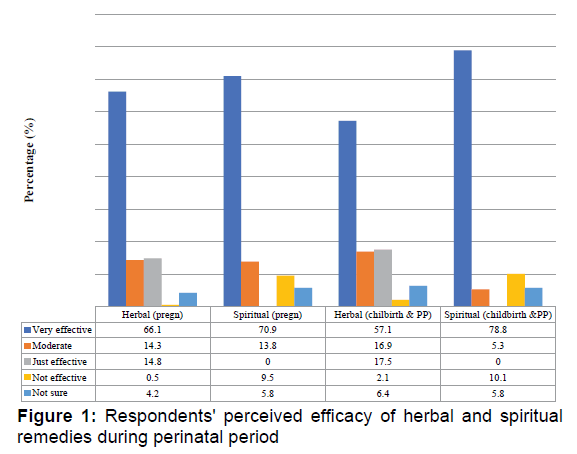
Majority of the mothers (66.1%) believed that herbal remedies are very effective in managing or preventing health conditions associated with pregnancy, and only one mother (0.5%) was skeptical about the use of herbal remedies these conditions. In the same vein, majority of the mothers (70.9%) reported that spiritual remedies are very effective in managing/preventing problems associated with pregnancy. However, up to 18 mothers (9.5%) reported that spiritual remedies are not effective in managing health conditions associated with pregnancy [Figure 1].
More than half of the mothers (57.1%) believe that herbal remedies are very effective in managing labour and health problems occurring during pueperium, but 12 (6.4%) and 4 (2.1%) were not sure about the effects, and that it was not effective respectively. On the other hand, most of the mothers interviewed believed that spiritual remedies are very effective (78.8%) in managing childbirth and post-partum conditions of mothers, but 19 (10.1%) felt that spiritual remedies are not effective while 11 (5.8%) were not sure of the effectiveness of the remedy as depicted in Figure 1.
Mothers’ perceptions about the safety of herbal and spiritual remedies during the perinatal period
Most of the 189 mothers (94.2%) believed that spiritual remedies are absolutely safe during pregnancy. On the other hand, 15.3% were not sure about the safety of herbal remedies in pregnancy because they associated it with miscarriages, low birth weight babies, liver disease, and fetal disease. Similarly, 97.9% of the mothers believed also that spiritual remedies are completely safe during labour and the immediate postpartum period. Furthermore, 91.0% of the mothers also opined that the use of herbal medications is safe during labour and pueperium. However, the remaining 9.0% that considered herbal remedies unsafe associated them with severe abdominal pain, prolonged labour, stillbirth, post-partum haemorrhage and maternal death.
Discussion
The observed level of use of herbal and/or spiritual remedies during pregnancy, labour and/or pueperium in this study is comparable with the global observed range of utilization of traditional medicines (TM),[4-7] but higher than those of local studies from other parts of Nigeria[8,21-23] and from Egypt.[24] The higher prevalence recorded may not be unrelated to the fact that TM has remained popular in northern Nigeria because of its relatively easy access both physically and financially; deeply rooted cultural and traditional beliefs in the region as well as observed successes associated with use of TM in the area.[8,9] Furthermore, policies and statutory laws regulating TM practice in Nigeria, like in many other developing countries are weak and poor, and by implication allow unrestricted access to unhealthy medications even within situations when drug prescriptions by qualified physicians are administered with caution.[3,7,15]
This study also observed that about two-thirds of the mothers combined traditional remedies with orthodox medicines during the perinatal period, and faith-based remedies like prayer healing or use of washings from the holy scriptures, and herbs were most commonly used to complement orthodox medicines. This corroborates the findings that many traditional healing methods
such as religious and spiritual healing are often used alongside more modern scientific medicine among Hausa villages and cities of northern Nigeria.[25] Religion has always enjoyed high favour within most African communities including Nigeria especially in the northern parts where advancement in medical practice, health awareness and utilization of health services are slow.[25,26]
Findings from this study revealed that mothers from the Hausa/ Fulani ethnic groups were much more likely to have used TM during the perinatal period. This is not surprising considering the fact that the Hausa/ Fulani are the predominant ethnic groups in the study area. Interestingly, the age of the mothers, their marital status, number of children, educational or employment status were not statistically associated with the mothers’ use of these remedies during the perinatal period, which did not support previous reports in the empirical literature.[7-10]
The indications for using herbal and spiritual remedies during pregnancy, labour or puerperal period reported by mothers in this study are consistent with those in the literature.[2,3,8,10-13] In contrast to Western Ethiopian study,[8] we found that the use of TM in our study area span throughout pregnancy, labour and puerperium. This could be very harmful, as it may increase the risk of pregnancy complications.[1] Our study found that 63.2% of the mothers used TM in combination with orthodox medicines, most used it via the oral route, and this may cause serious drug interactions and side effects in both mother and the unborn child.[1] The fact that up to 9% of our respondents considered TM unsafe in the perinatal period and another 15.3% were not even sure of its safety calls for renewed and concerted efforts in our society to counsel mothers on the perinatal use of TM during health talk in our antenatal clinics and more especially in the community where up to 40.7% of the respondents received advice on the use of TM. This may probably be achieved through jingles, advocacy visits and in the long run improving the socio-economic status of average Nigerian.
Most of our respondents believed that TM use is very effective in addressing their perinatal health problems. This is in keeping with a recent finding from Bulgaria,[27] where 94% of the respondents believed that herbs were beneficial to their health, but our report is higher than the 13.6%, 22.4% and 64.6% reported efficacy of herbal medicines from Western Ethiopia, western Nigeria, and Egypt respectively.[8,23,24]
Conclusion
The result of this study confirmed wide use of TM in the perinatal period. In view of the findings of the study therefore, there is need to investigate the safety concerns of these TM. Health authorities in Nigeria should as a matter of urgency institutionalize requisite structures for censoring, training and regulation of TM practitioners and their practice. The efficacy and safety of remedies used especially during the perinatal period should be established. Health authorities should also work closely with health care providers to intensify health awareness campaigns in the clinics, communities and through electronic and print media on dangers associated with irrational use of drugs especially for women in the perinatal period.
Limitations
The study was conducted among mothers of under five children and is thus subject to recall bias. The findings may not be generalizable to all settings as the study was undertaken on a small sample from only one out of 44 LGAs in Kano.
REFERENCES
- Tabatabaee M. Use of herbal medicine among pregnant women referring to Valiasr hospital in Kazeroon, Fars, South of Iran. J Med Plants. 2011;10.
- Holst L, Wright D, Nordeng H, Haavik S. Use of herbal preparations during pregnancy: Focus group discussion among expectant mothers attending a hospital antenatal clinic in Norwich, UK. Complement Ther Clin Pract. 2009;15:225-229.
- Olowokere AE, Olajide O. Women’s perception of safety and utilization of herbal remedies during pregnancy in a local government area in Nigeria. Clin Nursing Studies. 2013; 1:9-22.
- Spiritual Science Research Foundation. Principles of spiritual healing. Available from: http://www.spiritualresearchfoundation.org/spiritualresearch/spiritualscience/spiritualhealing?gclid=CjwKEAjwnKCrBRCm1YuPrtWW0QMSJAC-5UYkupp8gCkxojju_DeJcrEZOefU47ynyxHaPT1goBSs0BoC9Zjw_wcB
- Ernst E. Herbal medicines put into context. Brit Med J. 2003;327:881-882.
- Eisenberg D, Davis R. Trends in alternative medicine use in United States. J Am Med Ass. 1998;280:1569-1575.
- World Health Organization. WHO Traditional Medicine Strategy 2002-2005 Geneva 2002. Available from: http://www.wpro.who.int/health_technology/book_who_traditional_medicine_strategy_2002_2005.pdf.
- Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte hospital western Ethiopia. Jundishapur J Nat Pharm Prod. 2014; 9:e17368. Available from: http://jjnpp.com/?page=article&article_id=17368.
- Reyes-Ortiz CA, Rodriguez M, Markides KS. The role of spirituality healing with perceptions of the medical encounter among Latinos. Soc Gen Intern Med. 2009;24:542-547.
- Veale DJ, Furman KI, Oliver DW. South African traditional herbal medicines used during pregnancy and childbirth. J Ethnopharmacol. 1992;36:185-260.
- Tiran D. The use of herbs by pregnant and childbearing women: A risk benefit assessment. Complement Ther Nurs Midwifery. 2003;9:176-181.
- Kooi RV, Theobald S. Traditional medicine in late pregnancy and labour: Perceptions of Kgaba remedies amongst the Tswana in South Africa. Afr J Tradit Complement Altern Med. 2006;3:11-22.
- Varga CA, Veale JH. Isihlambezo: utilization patterns and potential health effects of pregnancy related traditional herbal medicine. Social Sci Med. 1997;44:911-924.
- Guyen RH, Wilcox AJ. Terms in reproductive and perinatal epidemiology. J Epidemiol Community Health. 2005;59:1019-1021.
- Adisa R, Fakeye TO. Assessment of knowledge of community pharmacists regarding common phytopharmaceuticals sold in southwestern Nigeria. Trop J Pharm Res. 2006;5:619-625.
- University of Twente. Health belief Model. Available from: http://www.utwente.nl/cw/theorieenoverzicht/Theory%20Clusters/Health%20Communication/Health_Belief_Model/
- Janz NK, Becker MH. The health belief model: A decade later. Available from: http://deepblue.lib.umich.edu/bitstream/handle/2027.42/66877/10.1177_109019818401100101.pdf?sequence=2&isAllowed=y
- National bureau of statistics (2006) Population census figures by states and LGAs. Available from: http://www.nigerianstat.gov.ng
- Lwanga SK, Lemeshow S. Sample size determination in health studies, a practical manual. Publication of World Health Organization. 1991;1-3.
- Onyiapat JE, Okoronkwo IL, Ogbonnaya NP. Complementary and Alternative Medicine use among adults in Enugu, Nigeria. BMC Complementary and Alternative Medicine. 2011; 11:19.
- Mureyi DD, Monera TG, Maponga CC. Prevalence and pattern of use of prenatal of traditional medicine among women at selected Harare clinics: A case-control study. BMC Complement Altern Med. 2012; 12:164.
- Opaneye AA. Traditional medicine in Nigeria and modern obstetric practice: need for cooperation. Cent Afr J Med. 1998; 44:258-261.
- Titilayo OF, Rasaq A, Ismail EM. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009; 9:53.
- Yasser IO, Nadia FF, Mohammed I, Abdul-Aziz I. Use of herbal medicines among pregnant women attending family health centers in Alexandria. Middle East Fert Soc J. 2014;19:42-50.
- Eucharia EN, Kabat HF. Nigerian’s use of native and western medicine for the same illness". Public Health Reports. 1984;99:93-98.
- Ismail M. Islamic medicine and its influence on traditional Hausa practitioners in northern Nigeria. USA: University of Wisconsin-Madison. 1981; 251.
- Asya PD, Vanya PK, Zheni DN, Teodora VK, Pavlina KJ. A study on current status of herbal utilization in Bulgaria: Part 1-Application of herbal medicines. Acad J. 2015;10:168-176.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.