Physiological Reactivity to Stress: Stratifying the Risk for the Development of Pathological Gambling
2 Deaprtment of Neuroapto Clinical and Applied Neuroscience, University of Cyprus, Nicosia, Republic of Cyprus
3 Health Services and Social Policy Research Center, Research Institution, Nicosia, Republic of Cyprus
4 Department of Monitoring, Cyprus National Addictions Authority & Gambling Harm Minimization Research Unit, Republic of Cyprus
Received: 21-Jun-2024, Manuscript No. amhsr-24-139569; Editor assigned: 24-Jun-2024, Pre QC No. amhsr-24-139569 (PQ); Reviewed: 08-Jul-2024 QC No. amhsr-24-139569; Revised: 15-Jul-2024, Manuscript No. amhsr-24-139569 (R); Published: 22-Jul-2024
Citation: Spyros C. Champi. Physiological Reactivity to Stress: Stratifying the Risk for the Development of Pathological Gambling. Ann Med Health Sci Res. 2024; S2: 930-934
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Individuals reactivity to stress is an important factor in the progression to Problem Gambling (PG). Stress responses are under tonic inhibitory control via Prefrontal Cortex (PFC) areas. Attenuation of PFC activity, via the Basolateral Amygdala (BLA), leads to disinhibition of the Central Nucleus of the Amygdala (CeA) that activates stress responses also associated with impaired decision-making and excessive risk-taking. Vagally mediated Heart Rate Variability (VmHRV) can assimilate the abovementioned mechanism which leads to excessive, suboptimal risk-taking, and thus, elevated risk for PG. With the aforementioned in mind, the present pilot study examined whether Vagally mediated Heart Rate Variability (VmHRV) can stratify the risk for the development of Problem Gambling (PG). One hundred and ninety individuals from professional populations at high risk for acute and/or chronic stress were recruited through online advertising. Eligible individuals completed the Problem Gambling Severity Index before proceeding with Electrocardiograph (ECG) and Heart Rate Variability (HRV) measures. Results indicated that VmHRV differed significantly across low risk (M=3.4, SE=0.05), moderate risk (M=3.27, SE=0.08) and problem gambling (M=3.17, SE=0.05), (F (2, 62)=8.2, p=0.001). These differences were unaffected after controlling for age, gender, and ethnicity. The findings of this study indicate that reactivity to stress, as measured via VmHRV, can differentiate individuals with distinct risk for PG. The findings of this study are likely to hold practical implications for public health initiatives relevant to problem gambling for professionals who are subjected to ongoing stress.
Keywords
Problem gambling; Problem gambling severity index; Heart rate variability; Stress; Public health
Introduction
Stress has long been implicated in the development of problematic gambling behavior [1]. For example, individuals’ reactivity to stress is seen as an important factor for the progression from social, low-risk to problematic/pathological gambling [2]. Stress responses are regulated by the Central Autonomic Network (CAN), a system of interrelated brain structures [3]. Within the CAN, the Central Nucleus of the Amygdala (CeA) is very important in the initiation of both the immediate, transient, and delayed, prolonged, stress responses.
The reciprocal interconnection between CAN’s neural structures allows the Prefrontal Cortex (PFC) to inhibit the amygdala, and thus, the individual to respond to stress in an effective manner. More specifically, the sympathetic output of the CAN is under tonic inhibitory control via prefrontal cortical areas, including the medial Prefrontal Cortex (mPFC) and the Orbitofrontal Cortex (OFC), that inhibit the amygdala via networks of gabaminergic neurons [4,5]. Attenuation of PFC activity, via the Basolateral Amygdala (BLA) leads to disinhibition of the CeA that can directly stimulate the hypothalamus and Rostral Ventrolateral Medulla (RVLM) which in turn activate relevant stress responses [6,7].
Given the association between stress and problematic gambling, it is no surprising that relevant research showed that the CeA and BLA are associated with impaired decision-making, including suboptimal risk-taking behavior as this is relevant to pathological gambling [8-11]. The deficient evaluation of risk that is evident in problem gambling is associated with volumetric decreases in the medial OFC, a structure involved in tonic inhibitory control of the amygdala [12]. Besides that, the functional connection between the PFC and the amygdala is important in the modulation of impulsive behavior which constitutes an important component of at-risk and problem gambling [13-15].
PFC’s control of the sympathetic output of the CAN points out its role in the modulation of the cardiac output. For example, research utilizing functional Magnetic Resonance Imaging (fMRI) to localize the central network for induced cardiovagal activity indicated a positive correlation between the dorsolateral PFC and VmHRV [16]. Similarly, fMRI paradigms examining the interaction between the brain and the heart in a resting state condition highlighted ventromedial PFC’s role in the generation of efferent vagal activity [17,18]. In addition, the pharmacological modulation (deactivation) of the activity of the PFC via intracarotid administration of sodium amobarbital resulted in the elevation of the HR and the concomitant decrease of the VmHRV [19].
As such, the neural substrates of Vagally mediated Heart Rate Variability (VmHRV) indicate that it is able to assimilate such an interfacing mechanism [20]. Indeed, relevant systematic reviews pointed out that higher VmHRV is associated with better decision-making performance under risk and uncertainty while at the same time pertinent research indicated that individuals with Internet gaming disorder have lower VmHRV compared to healthy controls [21,22]. Within this context, VmHRV integrates individuals’ reactivity capturing a prominent biological mechanism through which stress impacts risk evaluation and impulsive behavior. In essence, decreases in VmHRV signify the deactivation of the PFC, and thus, the disinhibition of CeA’s sympathetic input which leads to deficient risk evaluation and impulse control, and thus, elevated risk for problematic gambling.
The present pilot study examined whether VmHRV can stratify the risk for the development of problematic gambling. A first step toward that direction is the differentiation of individuals participating in casino games according to VmHRV. Within this context, the present pilot study expected that there would be significant differences between low-risk gambling, moderate- risk gambling, and problem gambling categories as classified by the Canadian Problem Gambling Index (CPGI).
Participants
One hundred-ninety individuals were recruited from professional populations at high risk for the development of acute and/or chronic stress deregulation in the UK via local online advertising [23,24]. Given the focus of the specific study on risk progression, one hundred twenty-five Individuals in the non-gambling and non-problem gambling categories were excluded from further analyses leaving sixty-five individuals (Mage=36.54, SD=5.43 years). Individuals suffering from metabolic disease, including diabetes, renal, cardiovascular or neuropsychiatric disease were excluded. Individuals suffering from temporal lobe epilepsy were also excluded from the present study. Moreover, individuals using medications altering their cardio-respiratory activity were not eligible to participate in the particular study [25,26]. Furthermore, individuals who were regularly involved in athletic and/or endurance sports were excluded given the evidence suggesting that cardiac vagal tone is affected by regular exercise [27].
Materials and Methods
Procedures and measures
Eligible individuals were requested to complete the Problem Gambling Severity Index (PGSI) of the Canadian Problem Gambling Index (CPGI), a public health screening instrument for problematic gambling before proceeding with ECG and HRV measures. The PGSI section of the CPGI was used to define cases in the current pilot study. Contrary to the majority of the screening tools currently in use, the PGSI was designed specifically for use with a general population rather than in a clinical context and encompasses harms associated with problem gambling [28]. Such screening is in line with contemporary research that approaches problem/pathological gambling as a public health concern recognizing the harms it places on the individual, communities and society [29-32].
The accuracy of screening tools, like the CPGI, is measured via sensitivity and specificity analyses [33]. Sensitivity refers to the proportion of individuals that display a condition, like PG, who are correctly identified as such by the screening tool (i.e., true positive). Specificity is relevant to the proportion of individuals that do not display a condition, like PG, who are correctly identified as such (i.e., true negative). The CPGI showed good sensitivity (83%) and excellent specificity (100%) as compared to DSM-IV classification criteria indicating high accuracy [34,35]. In addition, the CPGI showed good internal consistency (0.84), test-retest reliability (0.78) and criterion-related validity (concurrent validity 0.83) [36,37].
Screening classified participants into 5 categories including non-gambling, non-problem gambling, low-risk gambling, moderate-risk gambling, and problem gambling. Individuals in the non-gambling and non-problem gambling categories were excluded from further analyses. The remaining participants were required to abstain from caffeine, tobacco, and alcohol, for 2 hrs before ECG & HRV measurement sessions. Subsequent 5-minute resting supine position ECG and HRV measurements were obtained in the morning (between 08:00 and 11:00) in a temperature-controlled room (21°C-24°C). The sampling rate was set at 500 Hz with a digital electrocardiograph (BIOPAC MP160 System with ECG100C), consistent with international standards for ECG and HRV analysis [38]. ECG electrode placement followed an Einthoven’s triangle configuration. ECG data were analysed and RRi series were extracted using the AcqKnowledge software (version 4). Artifact detection followed previously established procedures [39]. RRi series were automatically pre-processed to remove ectopic beats and artifacts, and linear interpolation was used to replace any removed beats. HRV was measured as the Root Mean Square of Successive Differences (RMSSD) in the Inter Beat Intervals (IBIs). This time-domain measure is correlated with measures reflecting high frequency components of the respiratory range [38]. It therefore indicates parasympathetic influences to the heart and thus is considered as an indicator of VmHRV.
Ethics
The study was approved by the local ethics board and was undertaken in accordance with the Principles of Human Rights, as adopted by the World Medical Association at the 18th WMA General Assembly, Helsinki, Finland, June 1964 and subsequently amended at the 64th WMA General Assembly, Fortaleza, Brazil, October 2013. All participants gave their written informed consent to participate in the study after complete explanation of the procedures. Enrolled subjects did not receive any form of payment.
Results and Discussion
General sample characteristics
The mean age of the total sample was 36.54 years, 30.77% were women. Of these participants, 23.08% were Hispanic, 21.4% were Black/African American, 20% were Asians, and 20% were white. The majority of these individuals were single (24.62%), had either an undergraduate (30.77) or a postgraduate university degree (30.77%), and were currently employed (55.38%). Table 1 shows the general characteristics of the sample. Relevant analyses using Kruskal-Wallis H showed that there were no significant differences among the 3 groups in all demographic variables (Table 1).
| Variables | Total (N=65) | Low risk gambling (N=26) | Moderate risk gambling (N=21) | Problem gambling (N=18) | P Value |
|---|---|---|---|---|---|
| Age | 36.54 (5.43) | 35.1 (4.9) | 37.62 (5.46) | 37.4 (5.93) | 0.2 |
| Women (%) | 20 (30.77) | 9 (34.62) | 6 (28.57) | 5 (27.77) | 0.86 |
| Ethnicity | 0.6 | ||||
| Asian | 13 (20) | 5 (19.23) | 5 (23.81) | 3 (16.67) | |
| White | 13 (20) | 7 (26.92) | 2 (9.52) | 4 (22.22) | |
| Black/African | 14 (21.54) | 6 (23.08) | 4 (19.05) | 4 (22.22) | |
| American Hispanic/Latino | 15 (23.08) | 6 (23.08) | 6 (28.57) | 3 (16.67) | |
| Other/missing | 10 (15.38) | 2 (7.69) | 4 (19.05) | 4 (22.22) | |
| Education (%) | 0.83 | ||||
| High school | 13 (20) | 5 (19.23) | 6 (28.57) | 2 (11.11) | |
| College/technical school | 12 (18.46) | 5 (19.23) | 2 (9.53) | 5 (27.78) | |
| University (Undergrads) | 20 (30.77) | 6 (23.08) | 7 (33.33) | 7 (38.89) | |
| University (Postgrads) | 20 (30.77) | 10 (38.46) | 6 (28.57) | 4 (22.22) | |
| Employment status (%) | 0.46 | ||||
| Employed | 36 (55.38) | 13 (50) | 14 (66.67) | 9 (50) | |
| Unemployed | 20 (30.77) | 9 (34.62) | 5 (23.81) | 6 (33.33) | |
| Other/missing | 9 (13.85) | 4 (15.38) | 2 (9.52) | 3 (16.67) | |
| Marital status (%) | 0.22 | ||||
| Single | 16 (24.62) | 6 (23.08) | 8 (38.1) | 2 (11.11) | |
| Married/Living with partner | 13 (20) | 5 (19.23) | 5 (23.81) | 3 (16.67) | |
| Divorced | 14 (21.54) | 7 (26.93) | 2 (9.51) | 5 (27.78) | |
| Widowed | 13 (20) | 4 (15.38) | 3 (14.29) | 6 (33.33) | |
| Other/missing | 9 (13.84) | 4 (15.38) | 3 (14.29) | 2 (11.11) |
VmHRV
Participants’ scores were trimmed to three standard deviations of their mean. A set of Kolmogorov–Smirnov tests indicated that the natural logarithmic transformation of RMSSD did not deviate significantly from normality across the 3 classification categories, low risk (D=0.127, p=0.11), moderate risk, (D=0.156, p=0.18), and problem gambling (D=0.123, p=0.65).
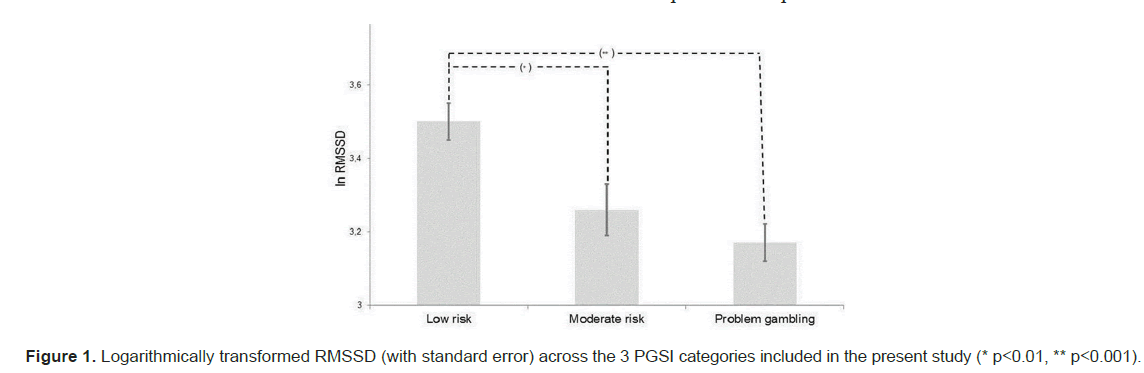
VmHRV, as indexed via RMSSD, differed significantly across low risk, moderate risk and problem gambling (F (2,62)=8.2, p=0.001). More specifically, relevant post-hoc analyses controlling for alpha inflation via Bonferroni correction (α=0.017) showed that participant with low risk for the development of problem gambling had significantly higher RMSSD compared to participants classified as having moderate risk (t (34.89)=2.56, p=0.008) or exhibiting problem gambling (t (42) = 4.51, p<0.001). Figure 1 displays all relevant post-hoc comparisons.
The present study controlled for the effects of age, gender, and ethnicity given that these variables have a consistent association with problem gambling [40,41]. The above mentioned differences in VmHRV between low risk, moderate risk, and problem gambling were unaffected after controlling for the effects of relevant covariates (F (2,59) =7.50, p<0.01). Post hoc tests showed there was a significant difference between low and moderate risk (p=0.02) and low risk and problem gambling (p=0.001). Estimated marginal means showed that individuals classified in the problem gambling category had lower VmHRV (M=3.17, SE=0.07) compared to moderate (M=3.27, SE=0.06) and low risk (M=3.5, SE=0.05) respectively.
Practical applications
The findings of the present study are likely to hold practical implications for public health protection and promotion initiatives relevant to problem gambling for professionals who are subject to ongoing stress. Such applications are likely to make use of recent technological advancements that enhanced the capacity of commercially available portable and wearable devices to record and monitor HRV [42,43]. For example, HRV data recorded by smart watches can be used to calculate and monitor VmHRV indices, and therefore utilised to further screening for problem gambling. Subsequently, this function can be employed to monitor gamblers current risk for problem gambling. Interfacing application can deliver continuous data monitoring from wearable devices into the smartphone of the gambler in a format that is simple to understand. Such information will allow gambles to evaluate their current risk for gambling in a manner that is considered problematic.
Limitations and future research
The cross-sectional nature of the particular study means that future research should examine the field utilization of VmHRV indices for the prospective stratification of the risk for problem gambling. Evidence arising from such longitudinal research can strengthen the findings of the present study and therefore support their use by stakeholders, policy makers and decision makers in developing public health protection and promotion applications to address problem gambling and associated harms. In addition, given the reliance of the present study on professional populations at high risk for the development of acute and/or chronic stress deregulation, future research should seek to replicate the present findings in a more diverse sample from the general population. The relatively small sample of the present research meant that we were unable to examine individual differences in terms of cognitive, perceptual aspects of stress [44]. Future research should, however, seek to replicate the present findings among larger, more diverse samples that would allow the examination of such individual differences.
Conclusion
The present pilot study aimed to examine differences in time domain indices of VmHRV between individuals classified as having low risk, moderate risk and problem gambling. Preliminary results indicated that there are significant differences in VmHRV between the 3 risk categories for problem gambling. These remained significant after controlling for relevant covariates including age, gender, and ethnicity. Estimated marginal means showed that individuals classified as belonging to the problem gambling category had lower VmHRV (M=3.17, SE=0.07) compared to individuals classified in the moderate (M=3.27, SE=0.06) and low risk (M=3.5, SE=0.05) categories respectively.
The findings of this study suggest that stress deregulation (i.e. deactivation of the PFC, and thus, the disinhibition of CeA’s sympathetic input) as measured via VmHRV can differentiate between individuals with distinct risk for problem gambling.
References
- Coman GJ, Burrows GD, Evans BJ. Stress and anxiety as factors in the onset of problem gambling: Implications for treatment. Stress Med. 1997; 13(4):235-244.
- Buchanan TW, McMullin SD, Baxley C, Weinstock J. Stress and gambling. Curr Opin Behav Sci. 2020; 31:8-12.
- Benarroch EE. The central autonomic network: Functional organization, dysfunction, and perspective. Mayo Clin Proc. 1993; 68(10):988-100. Elsevier.
- Gianaros PJ, Wager TD. Brain-body pathways linking psychological stress and physical health. Curr Dir Psychol Sci. 2015; 24(4):313-321.
- Shekhar A, Sajdyk TJ, Gehlert DR, Rainnie DG. The amygdala, panic disorder, and cardiovascular responses. Ann N Y Acad Sci. 2003; 985(1):308-325.
- Dilgen J, Tejeda HA, O'Donnell P. Amygdala inputs drive feedforward inhibition in the medial prefrontal cortex. J Neurophysiol. 2013; 110(1):221-229.
- Park AT, Leonard JA, Saxler PK, Cyr AB, Gabrieli JD, et al. Amygdala-medial prefrontal cortex connectivity relates to stress and mental health in early childhood. Soc Cogn Affect Neurosci. 2018; 13(4):430-439.
- Passecker J, Mikus N, Malagon-Vina H, Anner P, Dimidschstein J, et al. Activity of prefrontal neurons predict future choices during gambling. Neuron. 2019; 101(1):152-164.
- Tremblay M, Adams WK, Winstanley CA. Kindling of the basolateral or central nucleus of the amygdala increases suboptimal choice in a rat gambling task and increases motor impulsivity in risk-preferring animals. Behav Brain Res. 2021; 398: 112941.
- Van Holstein M, MacLeod PE, Floresco SB. Basolateral amygdala-nucleus accumbens circuitry regulates optimal cue-guided risk/reward decision making. Prog Neuropsychopharmacol Biol Psychiatry. 2020; 98:109830.
- Winstanley CA, Theobald DE, Cardinal RN, Robbins TW. Contrasting roles of basolateral amygdala and orbitofrontal cortex in impulsive choice. J Neurosci. 2004; 24(20):4718-4722.
- Freinhofer D, Schwartenbeck P, Thon N, Eigenberger T, Aichhorn W, et al. Deficient decision making in pathological gamblers correlates with gray matter volume in medial orbitofrontal cortex. Front Psychiatry. 2020; 11:109.
- Varkevisser T, Gladwin TE, Heesink L, van Honk J, Geuze E. Resting-state functional connectivity in combat veterans suffering from impulsive aggression. Soc Cogn Affect Neurosci. 2017; 12(12):1881-1889.
- Ioannidis K, Hook R, Wickham K, Grant JE, Chamberlain SR. Impulsivity in gambling disorder and problem gambling: Ameta analysis. Neuropsychopharmacology. 2019; 44(8):13541361.
- Paliwal S, Petzschner FH, Schmitz AK, Tittgemeyer M, Stephan KE. A model-based analysis of impulsivity using a slot-machine gambling paradigm. Front Hum Neurosci. 2014; 8:428.
- Napadow V, Dhond R, Conti G, Makris N, Brown EN, et al. Brain correlates of autonomic modulation: Combining heart rate variability with fMRI. Neuroimage. 2008; 42(1):169-177.
- Duggento A, Bianciardi M, Passamonti L, Wald LL, Guerrisi M, et al. Globally conditioned Granger causality in brain–brain and brain–heart interactions: A combined heart rate variability/ultra-high-field (7 T) functional magnetic resonance imaging study. Philos Trans A Math Phys Eng Sci. 2016; 374(2067):20150185.
- Ziegler G, Dahnke R, Yeragani VK, Bär KJ. The relation of ventromedial prefrontal cortex activity and heart rate fluctuations at rest. Eur J Neurosci. 2009; 30(11):2205-10.
- Ahern GL, Sollers JJ, Lane RD, Labiner DM, Herring AM, et al. Heart rate and heart rate variability changes in the intracarotid sodium amobarbital test. Epilepsia. 2001; 42(7):912-921.
- Champi SC. Vagally mediated heart rate variability: A risk factor for hypertension. NeuroRegulation. 2021; 8(3):173.
- Forte G, Morelli M, Grässler B, Casagrande M. Decision making and heart rate variability: A systematic review. Applied Cognitive Psychology. 2022; 36(1):100-110.
- Park SM, Lee JY, Choi AR, Kim BM, Chung SJ, et al. Maladaptive neurovisceral interactions in patients with Internet gaming disorder: A study of heart rate variability and functional neural connectivity using the graph theory approach. Addict Biol. 2020; 25(4):e12805.
- Stress and anxiety as factors in the onset of problem gambling: Implications for treatment
- Torpey, E. Adrenaline jobs: High-intensity careers : Career Outlook: U.S. Bureau of Labor Statistics. 2016.
- Quintana DS, Alvares GA, Heathers JA. Guidelines for Reporting Articles on Psychiatry and Heart rate variability (GRAPH): Recommendations to advance research communication. Transl Psychiatry. 2016; 6(5):e803.
- Quintana DS, Heathers JA. Considerations in the assessment of heart rate variability in biobehavioral research. Front Psychol. 2014; 5:805.
- Nakamura Y, Yamamoto Y, Muraoka I. Autonomic control of heart rate during physical exercise and fractal dimension of heart rate variability. J Appl Physiol. 1993; 74(2):875-881.
- Holtgraves T. Evaluating the problem gambling severity index. J Gambl Stud. 2009; 25:105-120.
- Abbott MW. The changing epidemiology of gambling disorder and gambling-related harm: Public health implications. Public health. 2020; 184:41-45.
- Browne M, Langham E, Rawat V, Geer N, Li E, et al. Assessing gambling-related harm in Victoria: A public health perspective. Victorian Responsible Gambling Foundation.2016; 188.
- John B, Holloway K, Davies N, May T, Buhociu M, et al. Gambling harm as a global public health concern: A mixed method investigation of trends in Wales. Front Public Health. 2020; 8:320.
- Wardle H, Reith G, Langham E, Rogers RD. Gambling and public health: We need policy action to prevent harm. BMJ. 2019; 365.
- Swift A, Heale R, Twycross A. What are sensitivity and specificity? Evid Based Nurs. 2020; 23(1):2-4.
- Currie SR, Hodgins DC, Casey DM. Validity of the problem gambling severity index interpretive categories. J Gambl Stud. 2013; 29: 311-327.
- Ferris JA, Wynne HJ. The Canadian problem gambling index. Ottawa, ON: Canadian Centre on substance abuse; 2001.
- Dellis A, Sharp C, Hofmeyr A, Schwardmann PM, Spurrett D, et al. Criterion-related and construct validity of the problem gambling severity index in a sample of South African gamblers. S Afr J Psychol. 2014; 44(2):243-257.
- Gorenko JA, Konnert CA, O’Neill TA, Hodgins DC. Psychometric properties of the problem gambling severity index among older adults. Int J Gambl Stud. 2022; 22(1):142-160.
- Electrophysiology TF. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation. 1996; 93(5):1043-1065.
- Goedhart AD, Van Der Sluis S, Houtveen JH, Willemsen G, De Geus EJ. Comparison of time and frequency domain measures of RSA in ambulatory recordings. Psychophysiology. 2007; 44(2):203-215.
- Håkansson A, Mårdhed E, Zaar M. Who seeks treatment when medicine opens the door to pathological gambling patients-psychiatric comorbidity and heavy predominance of online gambling. Front Psychiatry. 2017; 8: 255.
- Starcevic V, Khazaal Y. Relationships between behavioural addictions and psychiatric disorders: What is known and what is yet to be learned? Front Psychiatry. 2017; 8:53.
- Dalmeida KM, Masala GL. HRV features as viable physiological markers for stress detection using wearable devices. Sensors. 2021; 21(8):2873.
- Dobbs WC, Fedewa MV, MacDonald HV, Holmes CJ, Cicone ZS, et al. The accuracy of acquiring heart rate variability from portable devices: A systematic review and meta-analysis. Sports Med. 2019; 49:417-435.
- Koolhaas JM, Bartolomucci A, Buwalda B, de Boer SF, Flügge G, et al. Stress revisited: A critical evaluation of the stress concept. Neurosci Biobehav Rev. 2011; 35(5):1291-1301.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.