Postpartum Resumption of Sexual Activity, Sexual Morbidity and Use of Modern Contraceptives Among Nigerian Women in Jos
- *Corresponding Author:
- Dr. A. S. Anzaku
Department of Obstetrics and Gynecology, Bingham University Teaching Hospital, PMB 2238, Jos, Plateau State, Nigeria.
E-mail: steveanzaku@gmail.com
Abstract
Background: Postpartum sexual abstinence until when the child is weaned from breast milk is deeply rooted in most cultures in Nigeria. Aim: The study aimed at describing the current sexual practices of postpartum women, sexual morbidity, contraceptive prevalence and predictive factors for early postpartum sexual intercourse and associated sexual problems in our setting. Subjects and Methods: This cross‑sectional study was conducted among consecutive 340 women at a child welfare clinic 14 weeks after childbirth. Questionnaires were administered between January 2012 and June 2012 to ascertain their socio‑demographic and obstetric features, sexual activity, time to coital resumption, reasons for resumption and non‑resumption of intercourse, sexual problems encountered and contraceptive usage. Statistical analysis was performed using the SPSS version 16 for windows (SPSS Inc., Chicago, IL, USA). Results: Sexual intercourse was resumed by 67.6% (230/340) of women with a mean time to resuming intercourse of 8.2 (2.9) weeks postpartum and a median time of 8.0 weeks. About 3.5% (8/230) did so within the puerperium. Sexual intercourse was initiated mainly (77.4% [178/230]) by their husbands and only 19.1% (44/230) of them were using modern contraceptives. About 62.6% (144/230) of women experienced sexual morbidities including vaginal dryness/insufficient lubrication, dyspareunia and vaginal discharge. Socio‑demographic and obstetric features, menstrual and breastfeeding status were not predictive of early resumption of coitus. Vaginal delivery (OR: 3.6, 95% CI: 1.3‑10.0, P = 0.01,) and previous episiotomy (OR: 2.4, 95% CI: 2.0‑6.1, P = 0.04,) were predictive of sexual morbidity. Conclusion: Women in our setting resume sexual intercourse early after childbirth without the use of contraception and often with associated sexual morbidity. Emphasis on sexual and contraceptive education during the immediate postpartum period is therefore imperative.
Keywords
Contraception, Jos, Postpartum, Resumption, Sexual intercourse, Sexual morbidity
Introduction
The delivery of a child brings about a variety of changes to the mother’s health and wellbeing including fatigue, depression and changes in sexual function.[1-3] There are inconsistent reports concerning women’s sexuality after delivery. However, most studies report that interest in sexual activity often decrease throughout pregnancy, but eventually return to normal postpartum with average resumption of intercourse, ranged between 5 weeks and 8 weeks after childbirth.[4,5] Abstinence from sexual intercourse after childbirth until the child is fully weaned from breastfeeding is a deeply rooted practice in cultures of different communities.[6,7] Men were generally married to several wives in the past and a woman after childbirth was obliged to stay away from the husband with the aim of offering her the opportunity to breastfeed for as long as 2-3 years without intercourse to prevent pregnancy. Recent reports however, suggest that most women resumed sexual intercourse within 3-6 months of delivery,[8,9] which is a shift from the taboo against sexual intercourse after birth. The introduction of modern contraceptive methods and monogamous marital settings has probably led to changes in the socio-cultural practice of the people.
Women often experience sexual problems on resumption of sexual intercourse after childbirth, yet they are usually not reported and no medical interventions are sought.[9-11] These could reflect a lack of communication between women and their care givers with regard to postpartum sexuality. These sexual problems include superficial and deep dyspareunia, vaginal dryness/insufficient lubrication, vaginal tightness, looseness and discharge, loss of sexual desire and bleeding or irritation after sexual intercourse.[5,11,12] This silent affliction as postpartum sexual morbidity could be detrimental to women’s quality-of-life, negatively affecting their social, psychological, physical and emotional well-being.[13]
Commencement of sexual intercourse postpartum may also herald a greater risk of unintended pregnancies. Some women may be fecund few weeks after delivery especially those that are not breastfeeding. So, a sexually active woman after delivery not using an effective contraceptive method increases her vulnerability to pregnancy in the month before her first menstruation. Unintended pregnancy could lead to worrisome emotional and psychological disturbances for the woman and or the family as a whole. Pregnancy related health services are likely to expose women to various types of reproductive information and services including the practice of modern contraception. Reports suggest that prenatal care has a strong influence on subsequent use of modern contraceptive methods.[14] Despite the provision of information about contraceptive methods during antenatal and postnatal cares, most women resume sexual intercourse within 6 months postpartum without the use of a modern contraceptive method in many countries.[15,16]
Postpartum sexual health and sexual problems, which are common had received little attention from researchers and are often not discussed by clinicians during the prenatal and postpartum care, but the focus is mainly on postpartum contraception even though such discussion should be part of complete obstetric care.[10,11]
It is in view of these that this study was designed to establish the current sexual practices among our postpartum women, time taken to resume sexual activity, prevalence and pattern of sexual problems, prevalence of modern contraceptive usage as well as predictive factors for early resumption of sexual intercourse after childbirth and sexual morbidity among sexually active postpartum women attending a child welfare (immunization) clinic in Jos.
Subjects and Methods
This was a cross-sectional study among 340 consecutive women who brought their babies for the third dose of pentavalent vaccine 14 weeks postpartum at the child welfare clinic of Bingham University Teaching Hospital, Jos, from January 2012 to June 2012. This clinic is highly subsidized and attends to babies delivered by women from different hospitals and clinics in Jos. Eligible women were consecutively recruited for the study after obtaining verbal consent. The women were given questionnaires to fill and those that were not literate were interviewed by the nurses to extract the required information. The study was approved by the Human Research and Ethics Committee of the Hospital.
Data was sought on socio-demographic features, the last obstetric history, breastfeeding status and onset of menstruation after the delivery. The women were also asked whether they had resumed vaginal intercourse and if so, when after delivery and whether a modern contraceptive method was being used. Reason (s) for commencement of sexual intercourse, morbidity/problem(s) encountered and health seeking behavior was also recorded. A woman is said to have a sexual morbidity in this study if she reported one or more sexual problems on resumption of sexual activity after the last delivery. Women who had not resumed sexual intercourse were asked to state the main reason (s). Questions to ascertain reasons for resumption and non-resumption of sexual intercourse among the women were multiple choices. The response options for resumption of sexual intercourse included husband’s request, initiation by self, cultural demand, and feeling it was convenience to commence intercourse. Those of sexual problems were vaginal bleeding, vaginal discharge, vaginal dryness/insufficient lubrication, vaginal looseness, vaginal tightness, vaginal irritation after intercourse, painful penetration, pain during sexual intercourse, loss of sexual desire, lack of sexual satisfaction, tiredness and bruises/tear while that of non-resumption of coitus included unavailability of the husband, believe it was not yet time to commence coitus, feeling unwell, to avoid pregnancy, not interested and advice by a health worker.
Descriptive statistics were performed and relationship between sexual intercourse and other variables as well as pre-disposing factors to sexual problems were assessed by Chi-square tests for categorical variables and t-test (continuous variables) using SPSS version 16 for windows (SPSS Inc., Chicago, IL, USA). Variables with P < 0.05 on bivariate analysis were subjected to a multivariate logistic regression model to identify independent factors predictive of sexual problems among women that were sexually active after the last child birth.
Results
The response rate for the questionnaires was 96.6% (340/352) while 3.4% (12/352) declined to participate in this study. The non-response by some of the women was probably because they were shy to talk about sex and cultural taboo about public disclosure of sexual issues in some ethnic groups may also be responsible. However, among the women that participated in this study, their ages ranged from 18 years to 42 years, with a mean of 29.5 (4.7) years. They were of 49 different ethnic groups spread across Nigeria comprising mainly of Igbos (39.4% [134/340]), 8.8% (30/340) were Yoruba and 6.5% (22/340) were Beroms. About 45.3% (154/340) of them were engaged in business (traders), 23.5% (80/340) were civil servants and 13.5% (46/340) were housewives. Most of the women (92.3% [314/340]) had secondary or tertiary level of education. Table 1 shows the socio-demographic features of the women.
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age group (years) | ||
| ≤25 | 64 | 18.8 |
| 26-30 | 156 | 45.9 |
| 31-35 | 82 | 24.1 |
| ≥36 | 38 | 11.2 |
| Total | 340 | 100.0 |
| Educational status | ||
| Primary | 26 | 7.7 |
| Secondary | 116 | 34.1 |
| Tertiary | 198 | 58.2 |
| Total | 340 | 100.0 |
| Ethnic groups | ||
| Igbo | 134 | 39.4 |
| Yoruba | 30 | 8.8 |
| Berom | 22 | 6.5 |
| *Others | 154 | 45.3 |
| Total | 340 | 100.0 |
| Religion | ||
| Christianity | 334 | 98.2 |
| Islam | 6 | 1.8 |
| Total | 340 | 100.0 |
| Occupation | ||
| Business | 154 | 45.3 |
| Civil servant | 80 | 23.5 |
| Students | 58 | 17.1 |
| House wife | 46 | 13.5 |
| Missionaries | 2 | 0.6 |
| Total | 340 | 100.0 |
*Other ethnic groups-consist of 46 different ethnic groups in Nigeria including Irigwe, Mwaghvul, Ngas, Jarawa, Anaguta, Urhobo, Igala, Idoma, Mupun, Eggon, Tarok, Ozalla, Ibibio, Esan and Kwale (delta)
Table 1: Socio-demographic features of the women
About 67.6% (230/340) were of parity 1-2, with a mean of 2.2 (1.4). Majority of women (97.6% [332/340]) were breastfeeding exclusively or supplementing with bottle feeding. One hundred and two of the women (30%) had resumed menstruation after delivery with a mean time of 7.9 (3.7) weeks and a range of 4-13 weeks. Majority of the respondents (80.6% [274/340]) delivered vaginally, 19.7% (54/274) of them had an episiotomy while 29.9% (82/274) had vaginal laceration. Most of the episiotomies and vaginal lacerations (77.9% [106/136]) healed well while the rest developed complications, which included infection, chronic pain and scar formation. Table 2 shows the obstetric and reproductive features of the women.
| Characteristics | Frequency | Percentage |
|---|---|---|
| Parity | ||
| 1 | 138 | 40.6 |
| 2 | 92 | 27.1 |
| 3 | 46 | 13.5 |
| 4 | 40 | 11.8 |
| ≥5 | 24 | 7.0 |
| Total | 340 | 100.0 |
| Mode of delivery | ||
| Vaginal | 274 | 80.6 |
| Cesarean section | 66 | 19.4 |
| Total | 340 | 100.0 |
| Genital injury during the last delivery | ||
| Nil | 138 | 50.4 |
| Episiotomy | 54 | 19.7 |
| Vaginal laceration | 82 | 29.9 |
| Total | 274 | 100.0 |
| Outcomes of genital injury | ||
| Healed well | 106 | 78.0 |
| Chronic pain | 14 | 10.3 |
| Infected | 12 | 8.8 |
| Scar formation | 4 | 2.9 |
| Total | 136 | 100.0 |
| Postpartum menstruation (weeks) | ||
| ≤5 | 40 | 39.2 |
| 6-10 | 32 | 31.4 |
| 11-13 | 30 | 29.4 |
| Total | 102 | 100.0 |
Table 2: Obstetric and reproductive features of the respondents
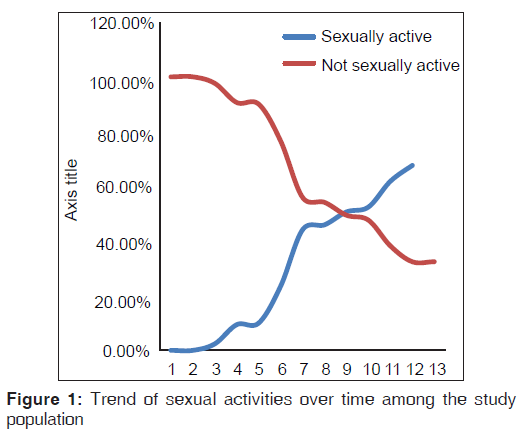
About two-thirds (67.6% [230/340]) of the women had resumed sexual intercourse with a median time to resumption of coitus after delivery of 8.0 weeks and a mean of 8.2 (2.9) weeks. Eight (3.5%) of them commenced sexual intercourse within the puerperium. The earliest time to commencement of coitus was 3 weeks while the latest time was at 13 weeks postpartum. Figure 1 depicts the trend of sexual activities over time among the study population. About 77.4% (178/230) of the women resumed sexual intercourse because of their husband’s request for sex while 14.8% (34/230) felt it was convenience to resume sex. Other reasons given for commencement of sexual intercourse include advice by health workers (10 [4.3%]), initiation by self (6 [2.6%]) and cultural demand (2 [0.9%]). Among the women that had resumed sexual intercourse, only 19.1% (44/230) of them were using modern methods of contraception. The contraceptive methods they were using included male condoms (31.8% [14/44]), intra-uterine contraceptive device (31.8% [14/44]), long acting injectable contraceptives (27.3% [12/44]) and sub-dermal implants (9.1% [4/44]).
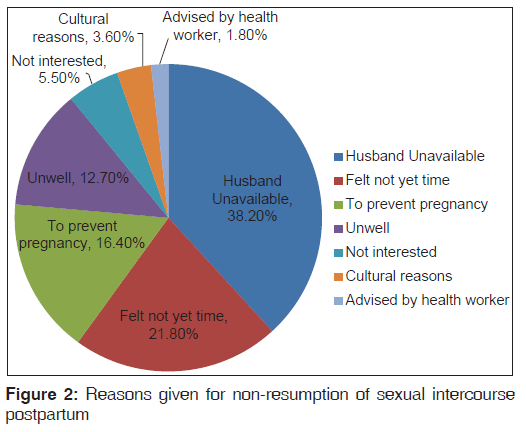
Furthermore, among the sexually active women, 62.6% (144/230) experienced at least a sexual morbidity/problem at the commencement of sexual intercourse, but only 22.2% (32/144) of them were still having the problem(s) at the time of enrolment into the study. Most of the problems abated spontaneously within 2.3 (2.1) weeks of resumption of coitus. Only 5.6% (8/144) of women with sexual problem(s) sought medical advice or intervention. Table 3 shows the types of sexual problems among the women. About one-third (32.4% [110/340]) of the women were yet to commence sexual intercourse 14 weeks after delivery. Forty two (38.2%) of the sexually inactive women had not resumed sexual intercourse because their husbands had been away from home after the childbirth. The reasons given for not resuming sexual intercourse after delivery are shown in Figure 2.
| Sexual problems | Frequency | Percentage |
|---|---|---|
| Vaginal dryness/insufficient lubrication | 28 | 16.7 |
| Deep dyspareunia | 25 | 14.9 |
| Vagina tightness | 22 | 13.1 |
| Superficial dyspareunia | 21 | 12.5 |
| Loss of sexual desire | 20 | 11.9 |
| Vaginal looseness | 14 | 8.3 |
| Abnormal vaginal discharge | 12 | 7.1 |
| Vaginal bleeding | 8 | 4.8 |
| Tiredness | 8 | 4.8 |
| ‡Others | 10 | 5.9 |
| Total | 168 | 100.0 |
‡Others include lack of sexual satisfaction, bruises/tear of external genitalia and vaginal irritation after coitus, *Out of the 144 women with sexual problems, some had multiple morbidities giving a total frequency of 168
Table 3: Sexual problems experienced among women
Maternal age (P = 0.41), educational status (P = 0.99), religion (P = 0.22), parity (P = 0.32), mode of delivery (P = 0.18), history of genital injury (P = 0.95), breastfeeding status (P = 0.08), and onset of menstruation (P = 0.86) were not significantly associated with the likelihood of early commencement of sexual intercourse among the women on univariate analysis. However, multivariate regression analysis identified two factors significantly associated with a higher likelihood of experiencing sexual morbidity among the women. Women that had a vaginal delivery were 3.6 times more likely to experience sexual problem(s) on commencement of coitus postpartum compared with those that delivered by caesarean section (OR: 3.6, 95% CI: 1.3-10.0, P = 0.01,). Furthermore, those that had an episiotomy or vaginal laceration were more likely to develop sexual problem(s) on resumption of sexual intercourse postpartum than those that has no genital tract injury (OR: 2.4, 95% CI: 2.0-6.1, P = 0.04,). Being a housewife positively influenced the likelihood of using a contraceptive method among the women that were sexually active after the last childbirth (OR: 1.3, 95% CI: 1.2-1.4, P = 0.04,). However, onset of menstruation (P = 0.11), breastfeeding (P = 0.81), and educational status (P = 0.15) were not associated with the likelihood of using a contraceptive method among the women.
Discussion
This study showed that 67.6% of the women had resumed sexual intercourse with a mean time of 8.2 (2.9) weeks. This reported rate could have been higher as over one-third (38.2%) of those that were not sexually active postpartum was as a result of unavailability of their husbands at home after the childbirth. However, the rate is comparable with 65% and 66.4% reported from Sagamu, Nigeria and Kampala, Uganda respectively.[8,17] It is higher than reports of 23.8% and 47% from Ghana and Germany,[15,18] but lower than 89% and 90% rates from the UK and USA respectively.[3,11,19] The mean time to resumption of coitus postpartum agrees with 7.87 (4.9) and 7.06 weeks reported from Turkey and Uganda.[12,17]
These differences in rates of resumption of postpartum sexual intercourse may be attributable to diverse cultural and religious practices and sexual attitudes of women in different parts of the world. Moreover, there were differences in postpartum periods where other studies were carried out (4-6 months) compared with this study, which was conducted at about 3 months after childbirth. The relatively high rate of early resumption of postpartum sexual intercourse in our study relative to the traditional practices suggests declining postpartum sexual abstinence after childbirth, which had been deeply rooted in our environment and cultures.[6,20,21] This may not be unconnected to the fact that there are changing cultural and sexual practices as a result of influence of Christianity, which forbids polygamy.
Over 98% of the women were from Christian setting, suggesting that they may be the only wife of their respective husbands. Hence, most men are now marrying one wife unlike in the past, which made it possible for a woman to abstain from sex until the child is weaned from breast milk while the man is having a sexual relationship with other wives. Nevertheless, the fact that the child welfare clinic is a paid clinic suggest that the socio-economic status of the women was mainly middle class and above. Hence, the reported time taken for resumption of postpartum sexual activity may not be generalized to the practice among women of low socio-economic status in our environment.
Women also cited different reasons why they resumed sexual intercourse early in the postpartum period. Most of them (77.4%) reported that request for sex by their husbands was the main reason for commencement of postpartum sexual activity. This was also noted as the commonest reason in other African settings in Uganda and Cote d’Ivoire.[17,22] About 14.8% of the women initiated sexual activity by themselves, which is in contrast to the traditional practice of postpartum sexual abstinence by couples until the child is fully weaned from breast milk.[6,7,23] This may be attributable to the fact that women may desire sex and want to feel close to their partners or may fear that their partners would seek sexual activity elsewhere if they delay sexual relations for too long.[22] Also, loss of sexual desire accounted for only 11.9% of sexual problems among women and so some couples may enjoy intercourse because it is pleasurable and increases their connection to their spouse especially with the challenges of caring for a newborn.
More worrisome is the low contraceptive prevalence (19.1%) among women who were sexually active including those that have commenced menstruation, even though postpartum women have the risk of getting pregnant even before the onset of menstruation. This low contraceptive rate among postpartum women was also noted in Lusaka, Zambia.[24] Onset of menstruation is thought to positively influence the commencement of contraception,[17] but this is in contrast to the finding in this study even though 30% of them had commenced menstruation. Women that are full time housewives are more likely to use a contraceptive method among women in this study. Education and literacy level usually predict contraceptive knowledge but predictor of poor usage.[25] This is also noted in this study as educational status is associated with poor contraceptive usage among the women. Hence, there is the need to re-emphasize in our health facilities the importance of postpartum contraceptive counseling as it has been found to positively influence the use of contraception after delivery among women.[25] Furthermore, this underscores the need to involve the men in sexuality education and involvement in contraceptive decision making and usage with the aim of preventing severe consequences of unplanned and unwanted pregnancies.
About 32.4% of the women were not sexually active after the last childbirth. The non-responders who were probably shy to talk about sex and bound by cultural taboo are the ones that are likely to delay the onset of intercourse in the postpartum period. Hence, this reported rate of postpartum abstinence could have been higher if they participated in the study. The major reason offered by women who were not sexually active was non-availability of their partners at home since the childbirth (38.2%). This is comparable to the finding in Uganda,[17] but in contrast to that in Ontario, Canada,[26] where decline in sexual desire was the main reason for non-resumption of coitus postpartum. This may be related to the fact that men in our environment have greater influence in control and initiation of sexual activity compared to advanced countries where women have better control of their sexuality because of knowledge about their sexual and reproductive rights and possibly better economic status. Other reasons given for non-resumption of coitus postpartum are similar to findings elsewhere.[17,26]
Sexual problems appear to be common on initiation of postpartum sexual intercourse, but few women discuss these with their health providers.[2,9,10] This was noted in this study as about two-third of the women experienced sexual morbidity, but only 5.6% of them sought medical advice or intervention. This may be because many of these symptoms were mild, transient as well as reporting sexual problems is often stigmatized and many women may not feel these are medical issues. This high sexual morbidity rate is higher than figures reported from Uganda (22.2%) and Gambia (27%),[17,27] but lower that 83% reported from Britain in the first 3 months postpartum,[28] though disorders related to sexual desire, arousal and orgasm were included in the study from Britain. Sexual issues are believed to be private and people tend to keep it to themselves and often postpartum sexuality is not routinely discussed with women during antenatal and postnatal care.[10,11] The reported sexual problems including vaginal dryness/insufficient lubrication, dyspareunia, abnormal vaginal discharge and bleeding reported in this study were also noted by other researchers;[1,12,17,21] though, most of the problems were transient with only 22.2% of the women still having the sexual morbidities.
Maternal age, parity, educational status, religion, mode of delivery, history of genital injury, breastfeeding status and onset of menstruation were not significantly associated with early resumption of postpartum sexual activity (P > 0.05). This is in contrast to the findings from other studies,[4,15,26] where mode of delivery, breastfeeding status and onset of menstruation positively influenced postpartum coital activity. This suggests that early commencement of sexual intercourse is common to all women in our setting irrespective of different socio-demographics and obstetric characteristics probably as a result of the influence of modern way of life and demand for sex by their husbands, which might have been promoted by the monogamous setting of the families.
However, women who had a vaginal delivery with or without episiotomy were more likely to experience sexual problems on resumption of coitus postpartum. This finding agrees with reports from other studies,[5,18,29] but in contrast to reports elsewhere.[30] Women may therefore benefit from open discussion about postpartum sexuality and problems so as to positively influence their health seeking behavior.
In conclusion, most women in this study resume sexual intercourse early after childbirth mostly as a result of initiation by their husbands and without the use of contraception. They often experience sexual morbidity, especially among those who had a vaginal delivery (with or without episiotomy) with poor health seeking behavior. Discussion with couples about postpartum sexuality and contraception should be part of routine antenatal and immediate postpartum care in order to prevent unplanned pregnancies and improve their health seeking behavior.
Strengths and limitations of the study
The strengths of this study are the prospective documentation of women sexuality early in the postpartum period thereby eliminating recall bias, and the reasons given for the resumption and non-resumption of sexual intercourse may help clinicians to discuss postpartum sexuality routinely in the context of postnatal care. However, cultural stigma associated with admitting desire for sex, especially in a period in which it is considered a taboo may affects the reasons given for resumption of intercourse as well as admission by women of resumption of postpartum sexual intercourse. The study was conducted in a single child welfare clinic and so may not be the true representative picture in the general population. Furthermore, the non-significant factors found may be owing to the small number of Muslims in the study and the sample size.
Acknowledgments
I acknowledge with thanks Mrs. Olasumbor Ojegbile and Mrs. Dinatu Bako for their assistance in data collection and women who participated in this study for sharing the stories of their private lives.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Thompson JF, Roberts CL, Currie M, Ellwood DA. Prevalence and persistence of health problems after childbirth: Associations with parity and method of birth. Birth 2002;29:83-94.
- Lamont J. Female sexual health consensus clinical guidelines. J Obstet Gynaecol Can 2012;34:769-75.
- Handa VL. Sexual function and childbirth. Semin Perinatol 2006;30:253-6.
- Byrd JE, Hyde JS, DeLamater JD, Plant EA. Sexuality during pregnancy and the year postpartum. J Fam Pract 1998;47:305-8.
- Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: A retrospective cohort study of primiparous women. Am J Obstet Gynecol 2001;184:881-8.
- Grudzinskas JG, Atkinson L. Sexual function during the puerperium. Arch Sex Behav 1984;13:85-91.
- Dada OA, Akesode FA, Olanrewaju DM, Olowu OA, Sule-Odu O, Fakoya TA, et al. Infant feeding and lactational amenorrhea in Sagamu, Nigeria. Afr J Reprod Health 2002;6:39-50.
- Sule-Odu AO, Fakoya TA, Oluwole FA, Ogundahunsi OA, Olowu AO, Olanrewaju DM, et al. Postpartum sexual abstinence and breastfeeding pattern in Sagamu, Nigeria. Afr J Reprod Health 2008;12:96-100.
- Abdool Z, Thakar R, Sultan AH. Postpartum female sexual function. Eur J Obstet Gynecol Reprod Biol 2009;145:133-7.
- Leeman LM, Rogers RG. Sex after childbirth: Postpartum sexual function. Obstet Gynecol 2012;119:647-55.
- Barrett G, Pendry E, Peacock J, Victor C, Thakar R, Manyonda I. Women’s sexual health after childbirth. BJOG 2000;107:186-95.
- Acele EÖ, Karaçam Z. Sexual problems in women during the first postpartum year and related conditions. J Clin Nurs 2012;21:929-37.
- Hipp LE, Kane Low L, van Anders SM. Exploring women's postpartum sexuality: Social, psychological, relational, and birth-related contextual factors. J Sex Med 2012;9:2330-41.
- Zerai A, Tsui AO. The relationship between prenatal care and subsequent modern contraceptive use in Bolivia, Egypt and Thailand. Afr J Reprod Health 2001;5:68-82.
- Borda MR, Winfrey W, McKaig C. Return to sexual activity and modern family planning use in the extended postpartum period: An analysis of findings from seventeen countries. Afr J Reprod Health 2010;14:72-9.
- Nyengidiki KT, Eyindah CE. Contraceptive prevalence amongst women attending infant welfare clinic at the university of port harcourt teaching hospital. Port Harcourt Med J 2008;3:42-8.
- Odar E, Wandabwa J, Kiondo P. Sexual practices of women within six months of childbirth in Mulago hospital, Uganda. Afr Health Sci 2003;3:117-23.
- Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G, Dudenhausen JW. Rate of dyspareunia after delivery in primiparae according to mode of delivery. Eur J Obstet Gynecol Reprod Biol 2006;124:42-6.
- Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, et al. Sexual function 6 months after first delivery. Obstet Gynecol 2008;111:1040-4.
- Isenalumhe AE, Oviawe O. The changing pattern of post-partum sexual abstinence in a Nigerian rural community. Soc Sci Med 1986;23:683-6.
- Adinma JI. Sexual activity during and after pregnancy. Adv Contracept 1996;12:769-75.
- Desgrées-du-Loû A, Brou H. Resumption of sexual relations following childbirth: Norms, practices and reproductive health issues in Abidjan, Côte d'Ivoire. Reprod Health Matters 2005;13:155-63.
- Udry JR, Deang L. Determinants of coitus after childbirth. J Biosoc Sci 1993;25:117-25.
- Susu B, Ransjö-Arvidson AB, Chintu K, Sundström K, Christensson K. Family planning practices before and after childbirth in Lusaka, Zambia. East Afr Med J 1996;73:708-13.
- Newmann SJ, Goldberg AB, Aviles R, Molina de Perez O, Foster-Rosales AF. Predictors of contraception knowledge and use among postpartum adolescents in El Salvador. Am J Obstet Gynecol 2005;192:1391-4.
- Rowland M, Foxcroft L, Hopman WM, Patel R. Breastfeeding and sexuality immediately post partum. Can Fam Physician 2005;51:1366-7.
- Walraven G, Scherf C, West B, Ekpo G, Paine K, Coleman R, et al. The burden of reproductive-organ disease in rural women in The Gambia, West Africa. Lancet 2001;357:1161-7.
- Barrett G, Pendry E, Peacock J, Victor CR. Sexual function after childbirth: Women’s experiences, persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol 1998;105:242-4.
- Ejegård H, Ryding EL, Sjogren B. Sexuality after delivery with episiotomy: A long-term follow-up. Gynecol Obstet Invest 2008;66:1-7.
- Klein MC, Kaczorowski J, Firoz T, Hubinette M, Jorgensen S, Gauthier R. A comparison of urinary and sexual outcomes in women experiencing vaginal and Caesarean births. J Obstet Gynaecol Can 2005;27:332-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.