Predicting Cesarean Delivery in Nulliparous Women: The Role of Maternal Anthropometric Traits and Fetal Birth Weight
2 Department of Obstetrics and Gynaecology, Lagos State University Teaching Hospital, Lagos, Nigeria, Email: ayokunleolumodeji@yahoo.com
3 Department of Obstetrics and Gynaecology, College of Medicine, Afe-Babalola University, Ekiti State, Nigeria
Received: 05-Oct-2023, Manuscript No. amhsr-23-106735; Editor assigned: 09-Oct-2023, Pre QC No. amhsr-23-106735 (PQ); Reviewed: 23-Oct-2023 QC No. amhsr-23-106735; Revised: 30-Oct-2023, Manuscript No. amhsr-23-106735 (R); Published: 06-Nov-2023
Citation: Olumodeji AM. Predicting Cesarean Delivery in Nulliparous Women: The Role of Maternal Anthropometric Traits and Fetal Birth Weight. Ann Med Health Sci Res. 2023;13: 831-837
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The rate of caesarean section has increased rapidly in many parts of the world, and now it is one of the most commonly performed operations.
Aim: The study aimed to evaluate the role of maternal and fetal anthropometric parameters as possible predictors for cesarean delivery in nulliparous women.
Method: This was a comparative cross-sectional study, over a 9-month period, at the Federal Teaching Hospital Ido-Ekiti and Ekiti State University Teaching Hospital Ado-Ekiti, in which 700 nulliparous women in labour with cephalic presenting, singleton fetus at term were recruited and their mode of delivery noted. Study participants had their weight, body mass index, height, mid-upper arm circumference and new-born birth weight determined. These anthropometric parameters in women who achieved vaginal delivery were compared in women who had dystocia-indicated caesarean delivery. Women who had assisted vaginal delivery and emergency caesarean section due to a non-dystocia indication were excluded. The data obtained were analyzed using independent t-test, fisher’s exact test, chi-square and binary logistic regression at significance level of p<0.05 and 95% confidence interval.
Results: Three hundred and forty-six nulliparous women who had spontaneous vaginal delivery were compared with 354 nulliparous women who had caesarean delivery. The mean ages of those who had caesarean section and vaginal deliveries were 28.32 ± 83.86 years and 27.62 ± 4.04 years respectively. Predictors of caesarean section were height ≤ 150 cm (OR=10.831, P=0.001), maternal weight in 1st trimester ≥ 90 kg (OR=13.157, P=0.001), obesity (OR=56.617, P=0.001) (MUAC) >24 cm (OR=0.866, P=0.010) and birth-weight >3500 g (OR=0.108, P=0.001). There was no association between caesarean delivery rate and maternal age, gestational age at presentation, maternal weight at term, maternal weight gain and baby’s gender.
Conclusion: Obesity, short-stature and maternal weight of >90 kg in the first trimester in nulliparous pregnant women are factors associated with increased risk of caesarean delivery.
Keywords
Nulliparous; Caesarean delivery; Maternal anthropometry
Introduction
Caesarean section when genuinely indicated can prevent poor obstetric outcomes and be live-saving for both mother and fetus [1]. The rate of caesarean section continue to rise progressively with a wide variability among different countries and regions [2]. However, there is a growing concern for unnecessary caesarean sections. Unnecessary caesarean sections can increase the risk of maternal morbidity and neonatal death [1]. Approximately one in three pregnancies is delivered by caesarean, accounting for more than 1 million surgeries each year in United states [3,4]. In Nigeria, the rate of caesarean section varies from one centre to the other with 35.5% in Osogbo, 27.6% (Enugu), 20.3% (Birnin- Kebbi), 18.3%(Ilorin), 15.8%(Jos), 11.4% (Zaria) and 40.1% in Lasuth, Lagos having been reported [5-7]. These increases are due to a sharp rise in primary caesarean delivery rates [8]. Previous research has indicated that caesarean delivery compared with vaginal birth is associated with increased maternal and neonatal morbidity and mortality [9]. In order to reduce caesarean delivery in nulliparous women, it is important to screen nulliparous women for cephalopelvic disproportion, one of the leading indications for caesarean section among nulliparous women worldwide. Thus, this study was conducted to investigate the maternal anthropometric measurements and foetal birth weight associated with caesarean delivery in nulliparous women.
Materials and Methods
This was a comparative cross-sectional study that assessed the association of maternal anthropometric characteristics and fetal birth weight with caesarean delivery in nulliparous women with singleton fetus in cephalic presentation. This study was carried out for 9 months in the Departments of Obstetric and Gynaecology of the Federal Teaching Hospital Ido-Ekiti and Ekiti State University Teaching Hospital Ado-Ekiti. The study population consisted of nulliparous pregnant women who presented for delivery at the labour ward in the study locations and satisfy the inclusion criteria. The inclusion criteria for this study were nulliparous pregnant women, at term (37-42 weeks), singleton fetus in longitudinal lie and cephalic presentation, presenting in labour, and who had registered for antenatal care with their weight in the first trimester measured and documented. Excluded from this study were patients with medical complications such as essential hypertension, renal disorders, pre-eclampsia, eclampsia and cardiovascular disorder, patients with preterm delivery, patients with fetal malpresentation, patients with recent injuries, surgeries, malignancies and other inflammatory diseases or conditions, patients with multiple pregnancies and women who had caesarean section for nondystocia indication like fetal distress.
A structured proforma was used to obtain relevant data from each patient. The proforma contained a brief history regarding parity, socioeconomic condition, maternal age, occupation, education and antenatal care utilization. The variables included anthropometric measurements (Maternal height, weight, BMI, Mid-Upper Arm Circumference (MUAC), maternal weight gain and foetal birth weight). Maternal weight (kg) and height (m) were measure, expressed as body mass index (BMI-weight (kg)/height2 (m2). Maternal weight was measured by a standard scale to the nearest 100 grams. Maternal height was measured with a standard scale to the nearest millimeter and the maternal mid-arm circumference was measured by an inelastic tape to the nearest millimeter. Babies’ weight was measured by a standard scale to the nearest 10 grams and gestational age was calculated from the last menstrual period in completed weeks of gestation. Data was analyzed using statistical program for social sciences (SPSS)version 20(SPSS Inc., Chicago, Illinois, USA). P values were calculated using chi-square test, student t-test and Fisher’s exact test (where applicable). The p values were evaluated for statistical significance. A significant value was put at p<0.05.
Results
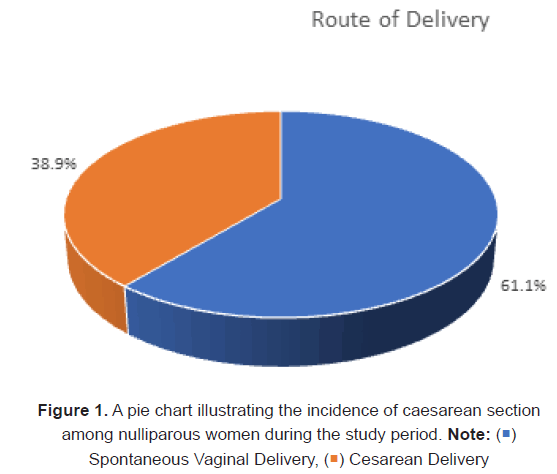
A total of 910 nulliparous pregnant women had deliveries in both centres during the period of study, out of which 700 consenting women who fulfilled inclusion the criteria were recruited into the study. Of the study participants, 346 had vaginal deliveries and the other 354 had emergency caesarean delivery. The Caesarean Section (CS) rate in nulliparous women during the study period was 38.9%. About 48.6% of the subjects were aged between 25 to 29 years. The mean ages of those who had caesarean section and vaginal deliveries were 28.32 ± 3.86 years and 27.62 ± 4.04 years respectively. There was a statistically significant difference between the mean age of the two groups (P=0.020) (Table 1). Most of the nulliparous pregnant women in both caesarean and vaginal delivery groups had some form of education, most had tertiary level of education (80.3% vs 67%). The level of education was statistically different between the two groups (P<0.001). Other characteristics of the study group are as depicted in Table 1.
| Spontaneous Vertex Delivery (%) (n=346) | Caesarean Delivery (%) (n=354) | Test of Significance | p-Value | |
|---|---|---|---|---|
| Age | ||||
| ≤ 19 years | 12 (3.5) | 17 (4.8) | ||
| 20–24 years | 57 (16.5) | 31 (8.8) | 10.871χ | 0.027 |
| 25–29 years | 155 (44.8) | 172 (48.6) | ||
| 30–34 years | 113 (32.7) | 128 (36.2) | ||
| ≥ 35 years | 9 (2.6) | 6 (1.7) | ||
| Mean ± SD | 27.62 ± 9.04 | 28.32 ± 3.86 | -2.327† | 0.02 |
| Marital Status | ||||
| Single | 28 (8.1) | 31 (8.8) | 0.100χ | 0.787 |
| Married | 318 (91.9) | 323 (91.2) | ||
| Occupation | ||||
| Unemployed | 59 (17.1) | 43 (12.1) | ||
| Artisan | 31 (9.0) | 20 (5.6) | ||
| Civil servant | 145 (41.9) | 191 (54.0) | 11.782χ | 0.091 |
| Trading | 79 (22.8) | 69 (19.5) | ||
| Student | 32 (9.2) | 31 (8.8) | ||
| Religion | ||||
| Christianity | 316 (91.3) | 335 (94.6) | 2.933χ | 0.103 |
| Islam | 30 (8.7) | 19 (5.4) | ||
| Tribe | ||||
| Yoruba | 324 (93.6) | 341 (96.3) | ||
| Igbo | 16 (4.6) | 13 (3.7) | 5.996χ | 0.07 |
| Hausa | 4 (1.2) | 0 (0.0) | ||
| Others | 2 (0.6) | 0 (0.0) | ||
| Level of education | ||||
| None | 1 (0.3) | 4 (1.1) | ||
| Primary | 16 (4.6) | 14 (4.0) | ||
| Secondary | 97 (28.0) | 52 (14.7) | 24.643χ | <0.001 |
| Teacher training college | 33 (9.5) | 35 (9.9) | ||
| Polytechnic | 101 (29.2) | 104 (29.4) | ||
| University | 98 (28.3) | 145 (41.0) |
Note: †=Independent t-testχ2═ Chi square
Table 1: Sociodemographic characteristics of the study population
The height of the women who had CS ranged from 145 to 171 cm (mean 158 ± 7 cm) while those who had vaginal deliveries ranged from 150 to 183 cm (mean 163 ± 6 cm). The caesarean section rate was found to be the highest (91.8%) among women who were less than or equal to 150 cm in height and least among those who were greater than 170 cm in height (18.97%). Hence, the height of women was found to be significantly associated with caesarean section (p<0.005) (Table 2).
The weights at 1st trimester of the subjects who had CS ranged from 45 to 128 kg (mean 70.19 ± 13.15 kg) while those that had vaginal deliveries were between 47 to 104 kg (mean 66.17 ± 10.85 kg). The weights at term of those that had CS were found to be in the range of 55 to 130 kg (mean 79.51 ± 12.72 kg) while those who had vaginal deliveries were between 53 to 110 kg (mean 73.09 ± 11.58 kg). The caesarean section rate was the highest (78.6%) among women who weighed 90 kg and above in the 1st trimester, with 21.4% of them having vaginal deliveries and was lowest (34%) amongst those who weighed 50 to 59 kg, with 66% of them having vaginal deliveries. Maternal weight was found to be significantly associated with caesarean section (p<0.001).
The weight gain in pregnancy for those who had CS ranged from 5 to 21 kg (mean 9.31 ± 3.27 kg), while those who had vaginal deliveries were between 4 to 18 kg (mean 6.91 ± 2.36 kg). The caesarean section rate was highest (77.8%) among women who had weight gain of 16 to 20 kg and was lowest amongst those who had weight gain of <6 kg (13.9%). Maternal weight gain was found to be significantly associated with caesarean section (p<0.001) (Table 2).
| Spontaneous Vertex Delivery (%) (n=346) | Caesarean Delivery (%) (n=354) | X2 | p-value | |
|---|---|---|---|---|
| Maternal Height | ||||
| ≤ 1.5 m | 5 (1.4) | 56 (15.8) | ||
| 1.5–1.6 m | 133 (38.4) | 174 (49.2) | 78.787 | <0.001 |
| 1.61–1.70 m | 161 (46.5) | 113 (31.9) | ||
| >1.7 m | 47 (13.6) | 11 (3.1) | ||
| Maternal Weight (1st Trimester) | ||||
| <50 kg | 10 (2.9) | 11 (3.1) | ||
| 50–59 kg | 99 (28.6) | 51 (14.4) | 27.508 | <0.001 |
| 60 –69 kg | 107(30.9) | 126 (35.6) | ||
| 70–79 kg | 90 (26.0) | 105 (29.7) | ||
| 80–89 kg | 34 (9.8) | 39 (11.0) | ||
| ≥ 90kg | 6 (1.7) | 22 (6.2) | ||
| Maternal Weight Gain | ||||
| <6 kg | 99 (28.6) | 16 (4.5) | ||
| 6–10 kg | 220 (63.6) | 275 (77.7) | ||
| 11–15 kg | 19 (5.5) | 32 (9.0) | 89.265‡ | <0.001 |
| 16–20 kg | 8 (2.3) | 28 (7.9) | ||
| >20 kg | 0 (0.0) | 3 (0.8) | ||
| Body Mass Index | ||||
| Normal | 121 (35.0) | 3 (0.8) | ||
| Overweight | 129 (37.3) | 106 (29.9) | 210.639‡ | <0.001 |
| Obese | 96 (27.7) | 245 (69.2) | ||
| Maternal Mid Upper Arm Circumference | ||||
| 20–24 cm | 34 (9.8) | 0 (0.0) | ||
| 25–29 cm | 162 (46.8) | 183 (51.7) | ||
| 30–34 cm | 137 (39.6) | 149 (42.1) | 50.111‡ | <0.001 |
| 35–39 cm | 11 (3.2) | 22 (6.2) | ||
| >39 cm | 2 (0.6) | 0 (0.0) |
Note: ‡=Fisher’s Exact test
Table 2: Anthropometric measurements of the study population
The BMI in pregnancy for those who had CS ranged from 22.90 to 50.15 kg/m2 (mean 31.96 ± 4.47 kg/m2), while that of those who had vaginal deliveries were between 19.8 to 42.74 kg/ m2 (mean 27.55 ± 4.27 kg/m2). The caesarean section rate was highest (71.8%) among women who had BMI of ≥ 30 kg/m2 (obese) and was lowest amongst those who had BMI of 18.5 to 24.9 kg/m2 (normal) (2.4%). Maternal BMI was found to be significantly associated with caesarean section (p<0.001) (Table 2).
The maternal MUAC of those that had CS ranged from 25 to 39 cm (mean 29.72 ± 2.68 cm), while that of those who had vaginal deliveries were between 20-40 cm (mean 28.67 ± 3.2 cm). The caesarean section rate was highest (66.7%) among women who had MUAC of 35-39 cm and was lowest amongst those who had MUAC of 20 to 24 cm (0%). Maternal MUAC was found to be significantly associated with caesarean section (p<0.001) (Figure 1).
The comparison of anthropometric measurements by route of delivery is depicted in the table below. It shows that the maternal height, maternal weight at 1st trimester and term, maternal weight gain, Body Mass Index (BMI) and maternal MUAC were significantly associated with caesarean delivery (Table 3).
| Spontaneous Vertex Delivery (%) (n=346) | Caesarean Delivery (%) (n=354) | T | p-value | |
|---|---|---|---|---|
| Maternal height (m) | 1.63 ± 0.06 | 1.58 ± 0.07 | 10.917 | <0.001 |
| Maternal weight in 1st trimester (kg) | 66.17 ± 10.85 | 70.19 ± 13.15 | -4.405 | <0.001 |
| Maternal weight at term (kg) | 73.09 ± 11.58 | 79.51 ± 12.72 | -6.972 | <0.001 |
| Maternal weight gain (kg) | 6.91± 2.36 | 9.31 ± 3.27 | -11.15 | <0.001 |
| Body mass index (kg/m2) | 27.55 ± 4.27 | 31.96 ± 4.47 | -13.35 | <0.001 |
| Maternal MUAC (cm) | 28.67 ± 3.27 | 29.72 ± 2.68 | -4.636 | 0.002 |
Note: t=student t-test
Table 3: Comparison of anthropometric measurements by route delivery.
Comparison between the neonatal parameters by route of delivery in both groups shows that the fetal birth weight among the subjects who had CS was within the range of 2.70 to 5.70 kg (mean 3.54 ± 0.48 kg) while in those who had vaginal deliveries, it was between 2.3 to 4.20 kg (mean 2.96 ± 0.37 kg). The caesarean section rate was found to be the highest (97.2%) in women with fetal weights of ≥ 4 kg while the least was in the<2.5 kg (0.0%) group. The birth weight of the babies was found to be significantly associated with caesarean section p<0.001 (Table 4).
Among the subjects who had CS, 57.3% of the baby’s gender was male and 42.7% was female. While in those who had vaginal deliveries, 47.1% of the baby’s gender was male and 52.9% was female (Table 4). The male gender of the babies was found to be statistically significantly associated with caesarean section p=0.008. Among the subjects who had CS, the mean Apgar scores of babies at 1 and 5 minutes were 7.53 ± 1.10 and 9.42 ± 0.71 respectively. While in those who had vaginal deliveries, the mean Apgar scores of babies at 1 and 5 minutes were 7.75 ± 0.85 and 9.73 ± 0.53 respectively. The Apgar scores of the babies at 1 and 5 minutes were similar in both groups and were not significantly associated with caesarean section p=0.090 and p=0.070 respectively.
| Spontaneous Vertex Delivery (%) (n=346) | Caesarean Delivery (%) (n=354) | T | p-value | |
|---|---|---|---|---|
| Foetal birth weight | ||||
| <2.5 kg | 4 (1.2) | 0 (0.0) | ||
| 2.5–3.5 kg | 315 (91.0) | 212 (59.9) | 126.202‡ | <0.001 |
| 3.51–3.99 kg | 25 (7.2) | 73 (20.6) | ||
| ≥4.0 kg | 2 (0.6) | 69 (19.5) | ||
| Mean ± SD | 2.96 ± 0.37 | 3.54 ± 0.48 | -18.088 | <0.001 |
| Median (IQR) | 2.9 (0.5) | 3.5 (0.6) | ||
| Baby’s Sex | ||||
| Male | 163 (47.1) | 203 (57.3) | 7.347χ | 0.008 |
| Female | 183 (52.9) | 151 (42.7) | ||
| Mean APGAR scores | ||||
| 1 minute | 7.75 ± 0.85 | 7.53 ± 1.10 | 2.976 | 0.09 |
| Median (IQR) | 8 (1.0) | 8 (1.0) | ||
| 5 minutes | 9.73 ± 0.53 | 9.42 ± 0.71 | 6.57 | 0.07 |
| Median (IQR) | 10 (0.0) | 10 (1.0) |
Note: t=student t-test, χ=chi square test, ‡=Fisher’s Exact test
Table 4: Comparison between the neonatal parameters by route of delivery.
Table 5 shows the binary logistic regression for predictors of caesarean section among the subjects. In logistic regression, the predictors of caesarean section were marital status (single) (OR=3.373, P=0.026), height ≤ 150 cm (OR=10.831, P<0.001), maternal weight in 1st trimester ≥ 90 (OR=13.157,P<0.001), overweight (≥ 25-29.99 kg/m2) (OR=25.419,P<0.001) and obesity(BMI ≥ 30 kg/m2) (OR=56.617, P<0.001).The other predictors of caesarean section were maternal MUAC>24 cm (OR=0.866, P=0.010) and birth weight >3500 g (OR=0.108, P<0.001) .There was no association between caesarean delivery rate and maternal age, gestational age at presentation, maternal weight at term, maternal weight gain and baby’s gender using binary logistic regression.
| Odds Ratio | 95% C.I | p-value | |
|---|---|---|---|
| Age | |||
| 17–25 years | 0.991 | (0.523 – 1.876) | 0.977 |
| 26–35 years | 0.981 | (0.594 – 1.621) | 0.942 |
| >35 years | 1 | ||
| Gestational Age at Presentation | |||
| >40 weeks | 1.085 | (0.671 – 1.755) | 0.738 |
| 37-40 weeks | 1 | ||
| Marital Status | |||
| Single | 3.373 | (1.153 – 9.864) | 0.026 |
| Married | 1 | ||
| Maternal Height | |||
| ≤ 1.5 m | 10.831 | (3.980 – 29.475) | <0.001 |
| >1.5 m | 1 | ||
| Maternal Mid Upper Arm Circumference | |||
| >24 cm | 0.866 | (0.776 – 0.967 | 0.01 |
| ≤ 24 cm | 1 | ||
| Maternal Weight in the First Trimester | |||
| ≥ 90 kg | 13.157 | (3.142-55.097) | < 0.001 |
| < 90 kg | 1 | ||
| Maternal Weight at Term | |||
| ≥ 90 kg | 0.467 | (0.202 – 1.082) | 0.076 |
| <90 kg | 1 | ||
| Maternal Weight Gain | |||
| 1.055 | (0.961 – 1.159) | 0.262 | |
| Body Mass Index | |||
| Obese | 56.617 | (14.746 – 217.388) | < 0.001 |
| Overweight | 25.419 | (6.996 – 92.364) | < 0.001 |
| Normal | 1 | ||
| Foetal Birth Weight | |||
| >3.5 kg | 0.108 | (0.055 – 0.212) | < 0.001 |
| ≤ 3.5 kg | 1 | ||
| Baby’s Sex | |||
| Male | 1.429 | (0.938 – 2.179) | 0.097 |
| Female | 1 | ||
| Constant | 1 |
Table 5: Binary Logistic regression (odds ratio) for predictors of caesarean section among the subjects.
Discussion
The rate of caesarean delivery has rapidly increased in many parts of the world and now it is one of the most commonly performed surgical operations. In order to minimize repeat caesarean section in subsequent pregnancies which could lead to increased maternal and perinatal morbidity, and mortality, it is important to identify nulliparous who are at risks of cephalopelvic disproportion and subsequent caesarean delivery. From the results of this present study, it is clear that there was a high incidence of caesarean delivery, especially among short, obese women and women who had large fetus. The rate of caesarean delivery was found to be 38.9% among nulliparous women. This is higher than the caesarean delivery rate (27.6%) among nulliparous women in Khatoun hospital, Sudan [10]. Previous studies in tertiary hospitals in Nigeria confirmed caesarean delivery rates of 18.3%, 27.6% and 35.5%, which was lower than the caesarean delivery rate (38.9%) found in our study [7,11].
This rate of caesarean delivery (38.9%) is much higher than the recommended rate of 15% by WHO [12]. In comparison with other studies, a high caesarean delivery rate of 40.1% was reported by Akinola et al., and a high rate of 43.2% was reported by Khatoun Hospital in Sudan [13,14]. This high rate of caesarean delivery is probably due to the increased likelihood of cephalo-pelvic disproportion and obstructed labour, in nulliparous pregnant women. Our study population consisted of only nulliparous women.
The socio-demographic characteristics in this study shows that the marital status and occupation of patients are similar in both groups. However, the level of education was found to be significantly associated with caesarean section on basis of univariate analysis only and not by binary logistic regression. Maternal age was not found to be a significant risk factor for caesarean section in this study (OR=0.981, p=0.942). This corroborates with a prior research conducted in LASUTH, Lagos, Nigeria [13]. However, in contrast with other studies, the increase in maternal age is associated with increase in caesarean delivery rates [10,15]. This may be due to the relatively younger age distribution of the patients in this study where most of the patients were aged between 25 to 29 years with only few patients above 35 years compared to other studies.
A surprising finding from this study is that being single was significantly associated with caesarean delivery(OR=3.373, P=0.026). This shows that single women were 3.37 times more likely to deliver by cesarean section. This could be due to the relative younger age of this patients where their pelvis may not be fully developed and therefore may have inadequate pelvis making it difficult for them to have vaginal delivery of relatively heavier newborn.
Although univariate analysis showed that the maternal height ≤ 150 cm, maternal weight at 1st trimester and term, maternal weight gain, increased Body Mass Index (BMI) and maternal MUAC, fetal birth weight and fetal male gender were significantly associated with caesarean delivery but binary logistic regression only showed that height ≤ 150 cm (OR=10.831, P<0.001), maternal weight in 1st trimester ≥ 90 (OR=13.157, P<0.001), overweight(≥ 25-29.99 kg/m2) (OR=25.419, P<0.001), obese (BMI ≥ 30 kg/m2) (OR=56.617, P<0.001) maternal MUAC>24 cm (OR=0.866, P=0.010), and birth weight >3500 g (OR=0.108, P<0.001) were statistically significant predictive factor for caesarean delivery. However, there was no association between cesarean delivery rate and maternal age, gestational age at presentation, maternal weight at term, maternal weight gain and male baby’s gender using binary logistic regression.
Another important analysis revealed that increase in maternal weight (OR=13.15, p=0.01) as well as increase in BMI were associated with increased risk of caesarean section. In line with previous studies, maternal weight was found to be associated with increase in the risk of caesarean delivery. This agrees with previous studies demonstrated by Akinola et al., in Lagos, Nigeria, Alsammani et al., at Khatoun hospital, Sudan and to findings in other studies [10,13,16,17]. This may be because increase in maternal weight and body mass index are associated with increased risk of fetal macrosomia leading to increased risk of cephalopelvic disproportion and need for caesarean delivery and is similar to findings from other studies.
Furthermore, although the univariate analysis showed that maternal weight gain in pregnancy was significantly associated with increased caesarean delivery but binary logistic regression showed no significant association. Contrary to a previous study done by Savitz et al., pre-pregnancy weight and weight gain in pregnancy have been proven to be associated with increased cesarean delivery rate [18]. Previous studies have also demonstrated that there was significant association between pre pregnancy weight, gestational weight gain and increase in BMI during pregnancy as risk factors for caesarean section and found a positive association [19].
The binary logistic regression analysis in this study showed that maternal height is a significant predictive factor for caesarean section (OR=10.831, p<0.001). In addition, results from this study shows that short statured nulliparous women (≤ 150 cm) had 10.8 folds risk of having a caesarean delivery. A short maternal stature is associated with an increased risk of obstructed labour due to cephalopelvic disproportion and most antenatal programmes designate short women as at risk. This is consistent with previously published studies which identified maternal height to be a predictive factor for cesarean section [10,20].
The maternal MUAC was found to be significantly associated with caesarean delivery. This is similar to previous studies which showed that MUAC correlated with increase in caesarean section rate [21,22]. However, this is in contrast to study done at Khatoun hospital in Sudan which showed no relationship between the two [10]. Various studies have shown that MUAC can be used as an indicator of the progress of pregnancy and its outcome. MUAC has also been proven to have excellent correlations with weight and BMI [21].
We found that birth weight >3500 g (which was obtained at delivery) increased the risk of cesarean delivery. This corroborates with a similar study done in Sudan where birth weight of >3750 g increased the risk of caesarean delivery. Increase in birth weight was found to be associated with an increased caesarean section risk in this study. The increase in caesarean section rate was more pronounced at birth weights of 4 kg and above (97.2% to 2.8%) and this is in line with a prior research carried out in Lasuth, Lagos where increase in birth weight of ≥ 4 kg was associated increased caesarean section rate [13]. Prior research have proven fetal macrosomia to be associated with increased risk of cephalopelvic disproportion leading to delivery by caesarean section [13,15].
The diagnosis of actual fetal birth weight is retrospective, and it cannot be used as a predictor for cesarean delivery, moreover, the clinical assessment and ultrasound for estimation of fetal weight have a limited predictive value and can lead to unnecessary obstetrical intervention [23]. In a recently published data, it has been reported that over half (52.4%) of macrosomic babies were diagnosed retrospectively indicating a limited value of clinical and ultrasound examinations for estimation of the fetal weight [24]. For this reason, fetal birth weight as a predictor of cesarean delivery rate cannot be put into practice since there is no an ideal method for optimal prediction of fetal weight estimation antenatally.
In this study, univarate analysis demonstrated that male fetal gender is significantly associated with caesarean section. However, with binary logistic regression, fetal gender is not a predictor of cesarean delivery. This agrees with another study conducted in Sudan which also showed no association between fetal gender and caesarean section [25]. However, Harlow et al., reported that fetal sex significantly influenced the cesarean delivery rate [10]. The mechanism whereby fetal sex affects the cesarean delivery rate remain unclear, some suggest increase production of corticosteroids by fetus which lead to more disposition of adipose tissues in fetal subcutaneous tissues.
The major findings in this study are high caesarean section rate due to CPD among nulliparous pregnant women. The predictors of caesarean section in this study are single marital status, short maternal stature(≤ 150 cm), maternal weight ≥ 90 kg in the 1st trimester, overweight and obesity, increased maternal MUAC and birth weight of >3500 g. Primary health care facilities and maternity homes, can antenatally counsel patients with these above risk factors, to have their labours monitored in facilities where CS can be offered if needed.
Conclusion
In conclusion, our study of nulliparous women undergoing childbirth revealed several significant predictors of caesarean section. Notably, height ≤ 150cm, maternal weight in the 1st trimester ≥ 90kg, obesity, maternal upper arm circumference >24cm, and birth-weight >3500g were all associated with a higher likelihood of caesarean delivery. These findings emphasize the importance of early monitoring and intervention for women with these risk factors to optimize maternal and fetal outcomes. These insights can inform clinical decision-making and patient counseling to reduce the rate of caesarean deliveries among nulliparous women.
Ethical Considerations
Verbal informed consent was obtained from all individual participants involved in the study. Approval for this study was obtained from the ethics and research committee of the Federal Teaching Hospital Ido-Ekiti with protocol number ERC/2015/01/13/01A.
References
- Cavallaro FL, Cresswell JA, Va França G, Victora CG, Jd Barros A, et al. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bulletin of the World Health Organization. 2013;91:914-922D.
[Crossref], [Google Scholar], [PubMed]
- Robson M, Hartigan L, Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best practice&research Clinical obstetrics&gynaecology. 2013;27:297-308.
[Crossref], [Google Scholar], [PubMed]
- Bragg, F, Cromwell DA, Edozien LC, Gurol-Urganci I, Mahmood TA, et al., Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. Bmj;2010:341.
[Crossref], [Google Scholar], [PubMed]
- Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, et al. Cesarean section rates and maternal and neonatal mortality in low‐, medium‐, and high‐income countries: An ecological study. Birth. 2006;33:270-277.
[Crossref], [Google Scholar], [PubMed]
- Adekanle DA, Adeyemi AS, Fasanu AO. Caesarean section at a tertiary institution in Southwestern Nigeria—A 6-year audit. 2013.
[Crossref], [Google Scholar], [PubMed]
- Ugwu EO, Obioha KC, Okezie OA, Ugwu AO. A five-year survey of caesarean delivery at a Nigerian tertiary hospital. Ann Med Health Sci Res. 2011;1:77-83.
[Google Scholar], [PubMed]
- Nwobodo E, Wara H. High Caesarean Section Rate at Federal Medical Centre, Birnin-Kebbi: Real or Apparent? Nigerian Medical Practitioner. 2004;46:39-40.
- Howell EA, Zeitlin J, Hebert P, Balbierz A, Egorova N. Paradoxical trends and racial differences in obstetric quality and neonatal and maternal mortality. Obstet Gynecol. 2013;121:1201-1208.
[Crossref], [Google Scholar], [PubMed]
- Organization WH. WHO statement on caesarean section rates. World Health Organization. 2015.
- Alsammani MA, Rayis DA, Abakur AO, Abdullahi H, Imam AM, et al. Maternal anthropometric characteristics and fetal birth weight as predictors of cesarean delivery in nulliparous women, with singletons pregnancies in cephalic presentation: A cross sectional study. Journal of Advances in Medicine and Medical Research. 2014;4:3022–3030.
[Crossref], [Google Scholar]
- Ijaiya M, Aboyeji P. Caesarean delivery: The trend over a ten-year period at Ilorin, Nigeria. Nigerian Journal of Surgical Research, 2001;3:11-18.
[Crossref], [Google Scholar]
- Organization WH. WHO recommendations: Intrapartum care for a positive childbirth experience. World Health Organization. 2018.
- Akinola OI, Fabamwo AO, Tayo AO, Rabiu KA, Oshodi YA, et al. Caesarean section--an appraisal of some predictive factors in Lagos Nigeria. BMC Pregnancy Childbirth. 2014;14:217.
[Crossref], [Google Scholar], [PubMed]
- Abdel-Rahman ME, Thalib L, Rayis DA. Caesarean section in Sudan: Findings from nationwide household surveys on rates, trends, and geographic and sociodemographic variability. BMC Pregnancy and Childbirth, 2022. 22:716.
[Crossref], [Google Scholar], [PubMed]
- Akindele AA, Okewole I, Omigbodun A. Multi variate analysis of risk factors for caesarean section in the university college hospital ibadan. Nigerian Journal of Clinical Practice. 2003;6:87-91.
- Roman H, Goffinet F, Hulsey TF, Newman R, Robillard PY, et al. Maternal body mass index at delivery and risk of caesarean due to dystocia in low risk pregnancies. Acta Obstet Gynecol Scand. 2008;87:163-70.
[Crossref], [Google Scholar], [PubMed]
- Fyfe EM, Anderson NH, North RA, Chan EHY, Taylor RS, et al. Screening for Pregnancy Endpoints (SCOPE) Consortium. Risk of first-stage and second-stage cesarean delivery by maternal body mass index among nulliparous women in labor at term. Obstet Gynecol. 2011;117:1315-1322.
[Crossref], [Google Scholar], [PubMed]
- Savitz DA, Stein CR, Siega-Riz AM, Herring AH. Gestational weight gain and birth outcome in relation to prepregnancy body mass index and ethnicity. Ann Epidemiol. 2011;21:78-85.
[Crossref], [Google Scholar], [PubMed]
- Klemetti M, Nuutila M, Tikkanen M, Kari MA, Hiilesmaa V, et al. Trends in maternal BMI, glycaemic control and perinatal outcome among type 1 diabetic pregnant women in 1989-2008. Diabetologia. 2012;55:2327-34.
[Crossref], [Google Scholar], [PubMed]
- Sheiner E, Levy A, Katz M, Mazor M. Short stature--an independent risk factor for Cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2005;120:175-8.
[Crossref], [Google Scholar], [PubMed]
- Shaikh F, Zeeshan F, Hakeem R, Basit A, Fawwad A, et al. Maternal dietary intake and anthropometric measurements of newborn at birth. The Open Diabetes Journal, 2009. 7:14-9.
- Kelly A, Kevany J, De Onis M, Shah PM. A WHO Collaborative Study of Maternal Anthropometry and Pregnancy Outcomes. Int J Gynaecol Obstet. 1996;53:219-33.
- Bajracharya J, Shrestha N, Karki C, Accuracy of prediction of birth weight by fetal ultrasound. Kathmandu University Medical Journal, 2012.10:74-76.
[Google Scholar], [PubMed]
- Alsammani MA, Ahmed SR. Fetal and maternal outcomes in pregnancies complicated with fetal macrosomia. North American journal of medical sciences, 2012. 4:283.
[Crossref], [Google Scholar], [PubMed]
- Abrams B, Altman SL, Pickett KE. Pregnancy weight gains: still controversial. The American journal of clinical nutrition, 2000. 71:1233S-1241S.

 )
Spontaneous Vaginal Delivery, (
)
Spontaneous Vaginal Delivery, ( ) Cesarean Delivery
) Cesarean Delivery


 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.