Primary Breast Tuberculosis Presenting as a Lump: A Rare Modern Disease
- *Corresponding Author:
- Dr. Samita Gupta
C/o Dr Kundan Lal Hospital, Ahmedgarh, Distt- Sangrur, Pin code – 148021, Punjab, India.
E-mail: singalsurgery@yahoo.com
Abstract
Breast tuberculosis is an uncommon form of entity especially in the infra‑mammary area. A 25‑ year‑old female, presented with a lump in the breast and infra‑mammary area. She was having off and on fever without any other complaints. There was no positive family history. Primary breast tuberculosis was diagnosed on fine needle aspiration cytology wherein ZN stain for acid fast bacilli was positive. The patient received antitubercular drugs and at 3 month follow up the swelling had resolved and the patient was asymptomatic. Breast tuberculosis is a rare disease with non‑specific clinical, radiological, and histological findings. Misdiagnosis is common as biopsy specimens are pauci‑bacillary and investigations such as microscopy and culture are frequently negative.
Keywords
Abscess, Breast, Extra–pulmonary, Infra-mammary, Lump, Tuberculosis
Introduction
Breast tuberculosis (TB) is classified as either primary or secondary TB. In 1829, Sir Astley Cooper described TB mastitis as “scrofulous swelling” in the bosom of young women.[1] It typically affects young lactating multiparous women and can present either as an abscess or as a painless breast mass. Primary breast TB is a rare form of extra-pulmonary TB. Although over one billion people suffer from TB worldwide, mammary TB is a relatively rare condition.[2] Its prevalence has been estimated to be 0.1% of breast lesions examined histologically.[3] Moreover, the diagnosis is not straightforward because of its similarity to carcinoma and bacterial abscesses. It is rare to see breast tuberculosis in infra-mammary area especially in unmarried female as seen in the presenting case.
Case Report
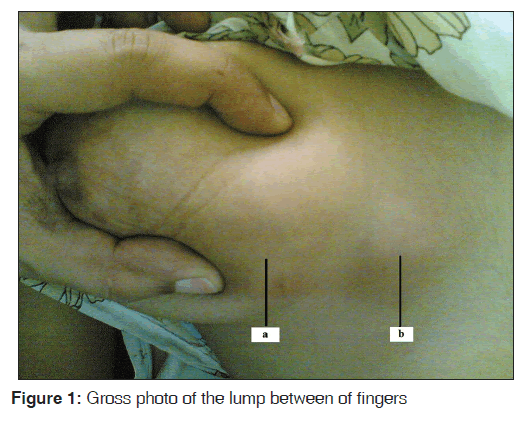
A 25-year-old female presented with a painless lump in her right breast for 1 month duration. She gave history of low grade fever off and on for the last 2 weeks. There were no other complaints like weight loss, loss of appetite, and any cough. She was unmarried and there was no positive family history of breast tuberculosis. On local examination, a non-tender lump of size 3 × 4 cm was felt in lower quadrant of the breast [marked with a line as a - Figure 1]. It was freely mobile and no axillary nodes were present. Another 1 × 1.5 cm swelling was present in infra-mammary area just below and medial to the above mentioned lump [marked by line b; Figure 1]. Her systemic examination was non-contributory.
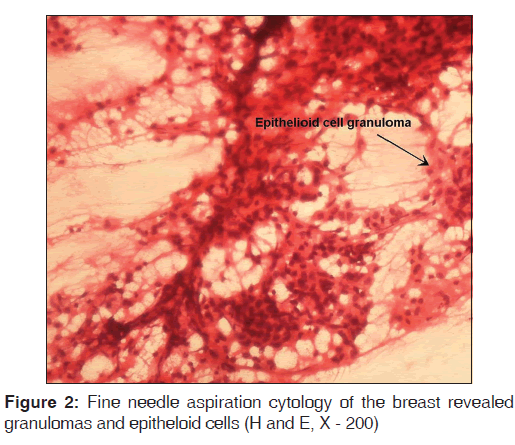
On routine blood investigations, total leucocyte count was 12,000 mm3 and erythrocyte sedimentation rate (ESR) was 60 mm at the end of 1 h, and HIV test was negative. Her fasting blood sugar and blood urea levels were normal. Chest X-ray was normal. Fine needle aspiration cytology (FNAC) of the breast and infra-mammary lump showed granulomas, epitheloid cells, and mixed inflammatory cells [Figure 2]. Background consisted of necrotic material and ZN stain for acid fast bacilli (AFB) was positive in the FNAC of both lumps. Mountex test was not done as on FNAC diagnosis already was made. Final diagnosis made as breast TB.
She was put on a 6-month course of anti-tubercular therapy with a 2 month intensive phase of rifampicin, isoniazid, ethambutol, and pyrazinamide followed by a consolidation phase of rifampicin and isoniazid for another 4 months. The lump size was decreased within 3 weeks of initiation of ATT and at 3 month follow-up the patient remains asymptomatic and both lumps disappeared. She was advised to continue treatment.
Discussion
Breast TB is an uncommon disease, with an incidence of less than 0.1% of all breast lesions in Western countries and 4% of all breast lesions in TB endemic countries.[4] It is uncommon because the mammary gland tissue, like the spleen and skeletal muscle, offers resistance to the survival and multiplication of the tubercle bacillus. Granulomatous mastitis can occur between 0.025% and 3% of all the breast diseases treated surgically.[2] Breast TB may be primary, when no demonstrable tuberculous focus exists elsewhere in the body or secondary to a pre-existing lesion located elsewhere in the body. It can spread by three routes – (a) hematogeneous, (b) lymphatic, (c) direct spread. Breast infection is seen more frequently secondary to a tubercular focus from the lungs, pleura or lymph nodes which may not be detected on radiology or clinically. Tewari and Shukla[4] recently classified mammary TB into three categories (a) nodulocaseous tubercular mastitis, (b) disseminated/confluent tubercular mastitis, and (c) tubercular breast abscess. Our case falls in the last category with primary breast TB because there was no evidence of another focus on physical or radiological examination nor there was prior history of tuberculosis. It is not always possible to detect acid-fast bacilli in histological sections of the breast tissue but these were detectable in the present case on ZN stain.[5]
Breast TB is classified into three types on basis of the clinical, radiological (mammographically) and pathological—a nodular form, a disseminated form, and a sclerosing form.[6,7] The nodular form is the most common and can be mistaken for fibro-adenoma or carcinoma.[4] Lesions due to TB have no specific ultrasonographic findings. They may be heterogeneous, hypoechoic, irregularly bordered mass with internal echoes or thick-walled cystic lesions on ultrasonography. In some cases, there may be fistula formation and thickening of Cooper’s ligaments and subcutaneous tissues.
The most reliable and definitive diagnostic studies include aspirate culture, polymerase chain reaction for mycobacterium, and histological examination of the tissue sample. If in doubt, computed tomography scanning may be useful for the differentiation of primary and secondary lesions by detecting continuity with the thoracic wall or pleura, and associated lesions of the lungs.[8] TB breast abscess can be diagnosed on mammography as a dense sinus tract connecting an ill-defined breast mass with a localized skin thickening but Khanna reported these findings in less number of cases.[2] FNAC from the breast lesion can diagnose breast TB in as many as three quarters of cases when both epitheloid cell granulomas and necrosis are present. However failure to demonstrate necrosis on FNAC does not exclude TB as often a spectrum of histological abnormalities can be found in breast TB specimens.[9] At MR imaging, parenchymal asymmetry with enhancement, microabscesses, and peripherally enhanced masses can be seen.
Treatment of breast TB with standard antituberculosis therapy for 6 months usually results in good clinical response.[10] The regimen consists of a 2 month intensive phase (isoniazid, rifampicin, pyrazinamide, and ethambutol) followed by a 4 month continuation phase (isoniazid and rifampicin). Surgical intervention is reserved for draining cold abscesses or excision of residual lumps. In our case, disease was successfully treated with anti-tubercular therapy.
Conclusion
The significance of breast tuberculosis is due to its rare entity and mistaken identity with breast cancer and pyogenic breast abscess. Caseating epitheloid cell granulomas in the tissue samples are diagnostic of tuberculosis. If there is a high clinical suspicion of TB, then a trial of anti-tubercular therapy with regular clinical assessment is warranted. Extrapulmonary tuberculosis occurring in the breast is extremely rare.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Cooper A. Illustrations of the diseases of breast: Part I. London: Longman, Rees Orme, Brown and Green; 1829. p. 73.
- Singal R, Dalal AK, Dalal U, Attri AK. Primary Tuberculosis of the Breast Presented as Multiple Discharge Sinuses. Indian J Surg 2013;75:66-7.
- BaniHani K, Yaghan R, Matalka I, Mazahreh T. Tuberculous mastitis: A disease not to be forgotten. Int J Tuberc Lung Dis 2005;9:9205.
- Tewari M, Shukla HS. Breast tuberculosis: Diagnosis, clinical features, and management. Indian J Med Res 2005;122:10310.
- Alzaraa A, Dalal N. Coexistence of carcinoma in tuberculosis in one breast. World J Surg Oncol 2008;6:29.
- Baharoon S. Tuberculosis of the breast. Ann Thorac Med 2008;3:1104.
- Gupta R, Singal R, Gupta A, Singal S, Shahi S, Singal R. Primary tubercular abscess of the breast an unusual entity. J Med Life 2012;5:98100.
- Schnarkowski P, Schmidt D, Kessler M, Reiser MF. Tuberculosis of the breast: US, mammographic and CT findings. J Comput Assist Tomogr 1994;18:9701.
- Sriram KB, Moffatt D, Stapledon R. Tuberculosis infection of the breast mistaken for granulomatous mastitis: A case report. Cases J 2008;1:273.
- Morino GF, Rizzardi G, Gobbi F, Baldan M. Breast tuberculosis mimicking other diseases. Tropical Doctor 2007;37:1778.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.