Primary Multidrug-Resistant Tuberculosis of the Breast- A Rare Presentation
2 Department of Pharmacology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, UP-243202, India, Email: drvpgiri@gmail.com
3 Department of Pharmacology, TMMCRC, Moradabad, UP, India
Citation: Vishal Prakash Giri. Primary Multidrug-Resistant Tuberculosis of the Breast- A Rare Presentation. Ann Med Health Sci Res. 2017; 7: 70-72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Tuberculosis of breast is a rare disease usually affecting young women in developing countries. In western countries it occurs most commonly in women of Asian origin. It is usually unilateral. It mimics pyogenic inflammatory disease and carcinoma of the breast. A 18 year old female patient presented with multiple discharging sinuses in left breast and fever for last four months. She had been treated with non-specific antimicrobials by physicians with no response. She neither had previous coexistent evidence of tuberculosis elsewhere in the body nor family history of tuberculosis. Pus was collected from discharging sinuses and subjected to Cartridge Based Nucleic Acid Amplification Test (CBNAAT). It detected Mycobacterium tuberculosis and Rifampicin resistance tuberculosis (RR-TB). Liquid culture and Drug susceptibility testing (LC-DST) confirmed it as a case of multidrug-resistant tuberculosis (MTB isolate Rifampicin and Isoniazid resistant).
Keywords
Breast; Tuberculosis; Multidrug-resistant; Disseminated tubercular mastitis; Confluent tubercular mastitis
Introduction
Mycobacterium tuberculosis (MTB) resistant to Rifampicin and other anti-tuberculosis drugs is a matter of global concern as it challenges the patient survival and public health. 3.9% of new Tuberculosis (TB) cases and 21% of previously treated TB cases worldwide had RR/MDR-TB (Rifampicin resistant/Multi Drug resistant TB). The corresponding figures for India being 2.5% and 16% respectively. [1].
Breast is an uncommon site for Extra- pulmonary tuberculosis (EPTB) with an incidence of less than 0.1% of all breast diseases in the western countries and 3% to 4% in TB endemic countries (India, China and Russia federations). It usually affects young lactating multiparous women. [2].
We present a rare case of breast TB in young, unmarried, nonlactating female due to resistant strains of Mycobacterium tuberculosis.
Case Report
A 18 year-old female reported in Pulmonary Medicine outpatient department of Darbhanga Medical College and Hospital, Bihar with complaints of purulent discharge from multiple sites in the lower part of left breast and fever for the last four months. History revealed that the number of sites of discharge gradually increased from one to five and fever was of low grade, intermittent with evening rise of temperature. The nature of the discharge was spontaneous and intermittent. She had been treated with several non-specific antimicrobials by family physician but there was no relief.
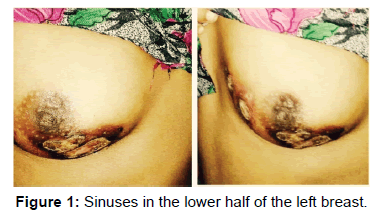
Breast examination revealed five sinuses in the lower half of the left breast [Figure 1]. These sinuses were discharging purulent secretions. The breast skin overlying them was thickened and discoloured. There was no tenderness, lump or nodularity over left breast on palpation. Right breast was normal. Axillary and cervical lymphnodes were not enlarged. Systemic examination revealed no abnormality.
Laboratory investigations viz. complete blood count, liver function tests, renal function tests, thyoid profile, plasma glucose, HIV serology, X-ray chest, CT-scan of chest, Ultrasonography (USG) of abdomen were normal.
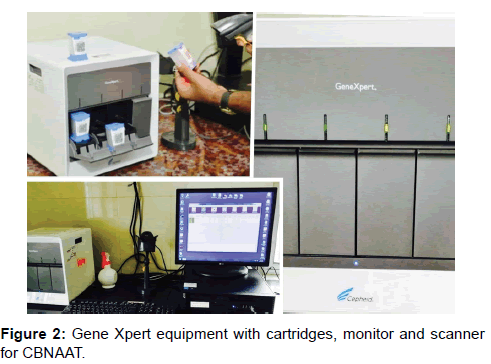
Purulent discharge (Pus) was microscopically examined after Gram’s, fluorescent and PAS staining with normal results. Purulent discharge revealed no microorganism on routine culture. It was also culture negative for fungi. Discharge was then subjected to MTB/RIF assay (CBNAAT) [Figure 2], which detected Mycobacterium tuberculosis and Rifampicin resistance.
Liquid culture and Drug susceptibility testing (LC-DST) of pus specimen by Bactec MGIT 960 system confirmed it as a case of MDR-TB [Figure 3]. The isolate (MTB) was resistant to Rifampicin (R) and Isoniazid (H). It did not show additional resistance to any other anti-TB drug.
Patient has been prescribed Shorter MDR-TB treatment regimen and is taking it for last two months. She is doing reasonably well at present. No adverse drug reaction (ADR) has been reported till date.
Discussion
Primary tuberculosis of breast has been previously reported by some authors from India. [3-9]. In most cases, diagnosis has been made by histopathological examination of the breast tissue. [3-5,7,9]. On the basis of bacteriological diagnosis, there is only one report of primary MDR-TB of the breast. [6].
The present case report of primary tuberculosis of breast is also bacteriologically confirmed and Rifampicin as well as Isoniazid resistant similar to Praveen and Nirat. [6].
Primary breast tuberculosis presented in most of cases either as breast lump [3,4,8]. or breast abscess. [4-7]. Our case report had multiple discharging sinuses.
At present breast tuberculosis is classified as Nodulocaseous tubercular mastitis, Disseminated/Confluent tubercular mastitis and Tubercular abscess. The sclerosing tubercular mastitis, tubercular mastitis obliterans and acute miliary tubercular mastitis varieties are of historical importance only. Breast TB may present as (a) lump in the breast, (b) Lump in the breast with discharging sinus, (c) Multiple sinuses without underlying lump, (d) symptoms of mastalgia and tender nodularity. [9].
Radiographic imaging is not a diagnostic in breast tuberculosis but defining the extent of legion. Histopathological diagnosis of breast tuberculosis is made by demonstration of epithaloid cell granuloma with caseous necrosis in the specimen obtained by Fine Needle Aspiration or Biopsy (core needle or open incision/ excision).
Tools for microbiological confirmation of breast tuberculosis are smear microscopy (Ziehl- Neelsen based microscopy/Light emitting diode based fluorescence microscopy) for acid fast bacilli (AFB), culture for mycobacterium tuberculosis (MTB) on solid media (Lowenstein-Jensen media/Middle brook and Cohn 7H10 media), or automated liquid culture system (Bactec MGIT 960 system/Bac T/Alert 3D system/Versatrek system and by rapid molecular diagnostic tests, Xpert MTB/RIF test (CBNAAT) for MTB specific DNA.
Genotypic drug susceptibility test (DST) can be performed rapidly for Rifampicin resistance (Rif’s resistance) by CBNAAT. Phenotypic DST can be performed in liquid culture system or solid media. The turnaround time for culture DST results by Solid LJ media is around 84 days and by Liquid culture (MGIT) is around 42 days. It takes around 2 hours by CBNAAT.
Mantoux test as well as serum interferon- gamma release assay (IGRA) can determine tuberculosis exposure in such patients. [10].
Conclusion
Differential diagnosis of breast tuberculosis includes idiopathic granulomatous mastitis (predominant neutrophil inflammation and lack of caseation necrosis), actinomycosis (sulphur granules in discharging pus, staining and culture for fungi), sarcoidosis (non-caseating granuloma and normal serum ACE), granulomatous vasculitis (autoantibodies and immunological tests) and foreign body giant cell reaction with fat necrosis.
Shorter MDR-TB treatment regimen consists of Intensive phase (4-6 months duration) comprising of Moxifloxacin- high dose, Kanamycin, Ethionamide, Clofazimine, Pyrazinamide, High dose Isoniazid and Ethambutol; and continuation phase (5 months duration) comprising of Moxifloxacin- high dose, Clofazimine, Pyrazinamide and Ethambutol. Total duration of treatment being 9 to 11 months. Dosage of drugs depend upon body weight of patient and weight band (16-29 kg, 30-45 kg, 46-70 kg, and >70 kg) to which patient belong.
We conclude that primary multidrug-resistant tuberculosis of breast should be considered in the differential diagnosis of chronic multiple sinuses in the breast. Discharging pus should be investigated for Mycobacterium tuberculosis and culture- DST should be done to find out the susceptibility pattern.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- WHO. Global tuberculosis report 2016 (WHO/HTM/TB/2016.13). 2016. www.who.int/tb/publications/global_ report/en/Date last accessed: November 7, 2016.].
- Marinopoulos S, Lourantou D, Gatzionis T, Dimitrakakis C, Papaspyrou I, Antsaklis A. Breast tuberculosis: Diagnosis, management and treatment. Int J Surg Investig Case Reports 2012; 31:548-550.
- Sen M, Gorpeligoglu C, Bozer M. Isolated primary breast tuberculosis-Report of three cases and review of literature. Clinics (Sao Paulo) 2009; 64:607-610.
- Hiremath BV, Subramaniam N. Primary breast tuberculosis: Diagnostic and therapeutic dilemmas. Breast Dis 2015; 35:187-193.
- Chowdri NA, Parray FQ, Dar RA, Malik AA, Mushtaque M, Malik RA. Tubercular mastitis–A rare presentation. Int J Surg 2010; 83:398-400.
- Kumar P, Sharma N. Primary MDR-TB of the breast. Indian J Chest Dis Allied Sci 2003;45:63-65.
- Kumar R, Kshetrimayum S, Kumar S, Garg R. Primary Tuberculosis of Breast: A Rare Presentation. Journal of Case Reports 2017; 7:127-129.
- Prathima S, Kalyani R, Parimala S. Primary tubercular mastitis masquerading as malignancy. J Nat Sci Bio Med 2014; 5:184-186.
- Gupta A, Bains L, Yadav D, Durgapal P, Agrawal MK. Tubercular mastitis: an institutional experience from a tertiary care centre of northern India. Asian J Med Sci 2017; 8:72-75.
- Gambhir S, Ravina M, Rangan K, Dixit M, Barai S, Bomanji J. Imaging in extrapulmonary tuberculosis. Int J Infect Dis 2017; 56:237-247.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.