Prosthodontic Management of Hypohidrotic Ectodermal Dysplasia with Anodontia: A Case Report in Pediatric Patient and Review of Literature
- *Corresponding Author:
- Dr. Ruchi Ladda
Department of Prosthodontics, Rural Dental College, Loni - 413 736, Maharashtra, India
E-mail: drruchikasat@gmail.com
Abstract
Ectodermal dysplasias are rare hereditary disorders characterized by abnormal development of certain tissues and structures of ectodermal origin. The condition is important for dentists as it affects teeth resulting in hypodontia or anodontia and dentist plays an important role in rehabilitation of the patient. Affected young children with anodontia not only have difficulties in eating and speaking but can also feel that they look different from their contemporaries. Well‑fitting and functioning prosthesis could be a great help during their schooling years as it will improve appearance and thus boost their self confidence. We report a case of hypohidrotic ectodermal dysplasia in an 8‑year‑old boy who exhibited anodontia and was successfully rehabilitated with conventional complete dentures in both maxillary and mandibular arches. The aim of the treatment was to improve psychological development apart from promoting better functioning of the stomatognathic system.
Keywords
Anodontia, Complete dentures, Dental implants, Ectodermal dysplasia
Introduction
Ectodermal dysplasias represent a large and complex nosological group of congenital diseases which were first described by Thurnam in 1948 and later in 19th century by Darwin. In 1921, Thadani assigned ectodermal dysplasia to the X chromosome.[1] EDs are rare and has an estimated incidence of 1 in 1 00 000 births. There exist more than 170 clinically distinct hereditary syndromes in which ectodermal dysplasia (ED) is present.[2-4]
This hereditary disorder is characterized by abnormal development of certain tissues and structures of ectodermal origin such as hair, nails, skin and teeth.[3-5] There are two major types of this condition: (1) anhidrotic or hypohidrotic (Christ-Siemens-Touraine syndrome), and (2) hidrotic (Clouston’s syndrome).[2,4,6,7] Clinical manifestations depend on the specific syndrome afflicting an individual. The most frequently reported ED syndrome is Christ-Siemens-Touraine syndrome.[5,8] The dentition and hair are affected similarly in both types, but the hereditary patterns, nail and sweat gland manifestations tend to differ.
Orofacial characteristics of this syndrome include anodontia or hypodontia, hypoplastic conical teeth, underdevelopment of the alveolar ridges, frontal bossing, a depressed nasal bridge, protuberant lips, and hypotrichosis.[5] It can affect both the primary and permanent dentition. The objectives of prosthetic dental treatment in young ED patient with anodontia are preservation of bone, early development of correct patterns of chewing, swallowing, speaking and restoring normal facial characteristics. Thus it facilitates development of normal emotional and psychological profile.
Case Report
An eight-year-old male patient reported to the Rural Dental Hospital with the complain of missing teeth causing difficulty in mastication and speech. He was accompanied by his father who gave the history of missing teeth of his son since infancy. He mentioned that child was intolerant to heat and prefers to be in cold environment. Patient also reported about absence of sweating. Family history revealed that he was the second kid of parents with non consanguineous marriage and none of the other members or relatives had similar condition.
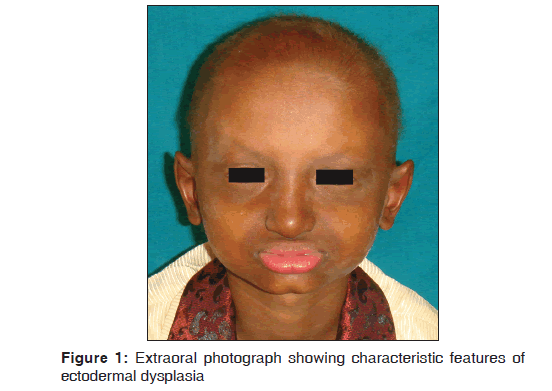
The boy was moderately built and poorly nourished with BMI value of 12.5 kg/m2. His skin was dry with scanty body hair. The nails were not affected. Extraoral examination revealed the typical features of ectodermal dysplasia like sparse scalp hair, frontal bossing, absent eyebrows, loss of eyelashes, hyper pigmentation around the eyes and mouth, saddle nose and protuberant lips. A diminished lower facial height contributed to a senile facial expression [Figure 1].
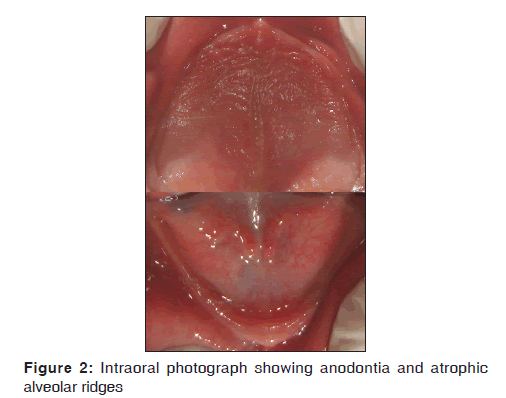
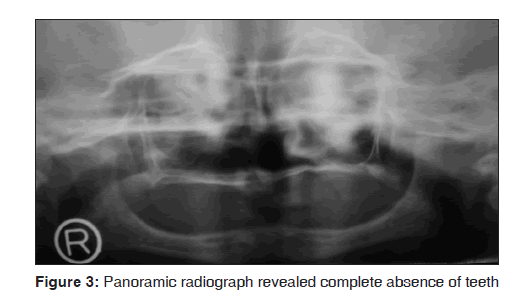
Intraoral examination revealed thin, atrophic and complete edentulous maxillary and mandibular alveolar ridges [Figure 2]. Anodontia as well as underdevelopment of alveolar ridges was also confirmed by panoramic radiography [Figure 3]. Correlating clinical, radiographic and skin biopsy findings, the boy was diagnosed with hypohidrotic ectodermal dysplasia with complete anodontia.
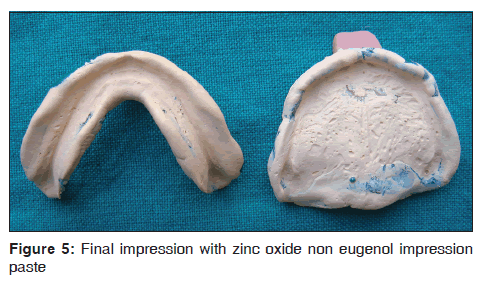
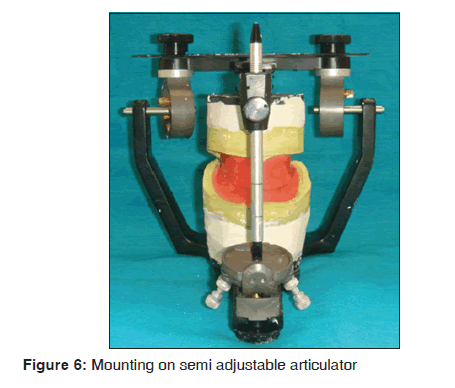
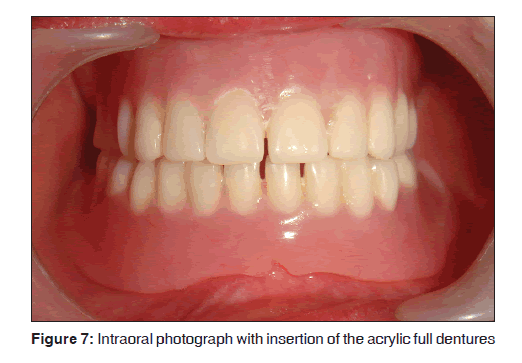
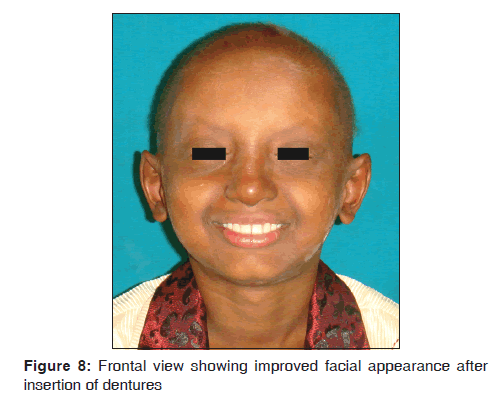
Treatment plan was discussed with patient and his father. Informed consent was obtained for the agreed treatment. The child was rehabilitated with removable maxillary and mandibular complete dentures. Routine procedures were followed for the construction of the complete dentures which included preliminary impressions with irreversible hydrocolloid [Figure 4], fabrication of special trays using autopolymerizing acrylic resin after applying spacers, border-molding with low fusing compound, final impression with zinc oxide non eugenol impression paste [Figure 5], recording of maxillomandibular relations and mounting the casts on semi adjustable articulator [Figure 6]. Rather than primary tooth forms, permanent tooth forms were selected in order to provide better static and dynamic occlusion. Teeth arrangement was done and bilateral balanced occlusion was given. Trial dentures were checked for retention, phonetics, occlusion and esthetics. The denture base was processed through compression molding using heat cure fiber reinforced acrylic material (DPI, Mumbai, India) for stability and longevity. The processed dentures were finished and polished. Occlusal equilibrium was confirmed. After the insertion of dentures [Figure 7], postplacement instructions were given to child and his parents. The facial profile and expression improved significantly with complete dentures [Figure 8].
Patient was very cooperative throughout the clinical procedures. Recall appointments were scheduled after 24 hours, 1 week, and 4 weeks. After 4 weeks the patient was able to function well with both maxillary and mandibular dentures. In order to accommodate growth and development, the patient was scheduled for ongoing follow up visits every 6 months. At recall appointments, good retention was observed and the parents reported a significant improvement in terms of speech and mastication.
Discussion
Freire-Maia defined the nosologic group of ED as any syndrome that exhibits at least two of the following features: (1) trichodysplasia (abnormal hair), (2) abnormal dentition, (3) onchodysplasia (abnormal nails), and (4) dyshidrosis (abnormal or missing sweat glands).[5] ED follows all possible modes of Mendelian inheritance, i.e., autosomal dominant or recessive or X-linked dominant or recessive and also sporadic cases have been reported.[2,3] Pathogenesis is thought to involve an altered epithelium-mesenchymal interaction. About 30 causative genes have been isolated [2] and mutations in the ectodysplasin-A and ectodysplasin-A receptor genes is thought to be responsible for X-linked and autosomal hypohidrotic ectodermal dysplasia.
There are two major types of this condition depending on the number and functionality of the sweat glands: (1) anhidrotic or hypohidrotic, where sweat glands are either absent or significantly reduced in number and the condition shows X-linked recessive inheritance severely affecting males, while females show only minor defects (Christ-Siemens-Touraine syndrome), and (2) hidrotic, where sweat glands are normal and the condition is inherited as autosomal dominant trait (Clouston’s syndrome).[2,6,7] In the present case hypohidrotic form was present.
The anhidrotic/hypohidrotic ED is the more severe form and is associated with more dental defects.[5] It exhibits the classical triad of hypohidrosis (diminished perspiration), hypotrichosis (decreased amounts of hair), and hypodontia (decreased number of teeth). Partial or complete absence of sweat glands is responsible for inability to perspire and accounts for intolerance to heat and hyperthermia. Hair of scalp, eyebrows and eyelashes tend to be fine, scanty and blond.[2,9] Dental findings usually reveal multiple congenitally missing teeth, conoid incisors and taurodontic primary second molars.[2] Anodontia causes lack of alveolar ridge development leading to reduced vertical dimension, vermilion border disappears and lips become prominent. The face of an affected child usually has the appearance of old age. The diagnosis of hypohydrotic ED is usually performed by a biopsy of the skin that shows absent or hypoplastic sweat glands. Additionally, for some subtypes of ED genetic testing is available.[3]
There is no definitive time to begin dental treatment, but Pigno, et al. suggest that an initial prosthesis should be provided before school age of the patient.[5] Prosthodontic treatment commenced at an early age of 3-4 years helps to normalize the function of masticatory and perioral muscles and consequently the growth pattern of basal bones, thus giving a psychological boost to the self-image of the child.[1] Prosthodontic treatment of ED patient can include fixed, removable, or implant-supported prostheses used individually or in combination to provide an optimal result. Fixed prostheses are seldom used exclusively in the treatment of ED because of the presence of a minimal number of teeth and interference with jaw growth in young patients due to rigid connectors if the prosthesis crosses the midline.[5]
Removable prosthesis (complete dentures, partial dentures or overdentures) is the most frequently reported treatment modality for the dental management of ED in childhood because these can be easily modified during periods of rapid growth.[5,9] In the present case, conventional complete dentures in both arches were planned. Although dentures are poor alternatives to healthy dentition, they maintain a normal, satisfactory daily diet, thus helping to set up a lifelong dietary pattern at an early age.[1] It is known that from around nine years of age, children with disabilities realize that they will remain different from other children. Therefore, prosthetic intervention in this case at the age of eight is valuable in terms of psychological development.
For an adult ED patient, dental implants have become the treatment of choice, because growth is stabilized by adulthood and the implants can be used to support, retain and stabilize the prosthesis. Guckes, et al. presented 90% implant stability at second-stage surgery in a group of ED patients aged 13-69.[6] Though literature describes placement of implants as early as 3 years,[10] it is not recommended to place implants in growing children as a routine practice (especially in maxilla).[11] According to the guidelines of National Foundation for ED, implants are recommended for the anterior mandible in children older than school age (7 years or older).[12] A 1989 Consensus Conference on Implantology concluded that implants should be placed after maximum jaw growth has occurred (15 years of age).[13] Cronin, et al.[11] concluded that implants placed after age 15 years for girls and 18 years for boys provided the most predictable prognosis.
Number of authors have mentioned possible consequences of oral implants, if placed before dental and skeletal maturation.[3,6,10] Experimentally, it is shown that endosseous implants placed in young pigs behave similar to ankylosed teeth,[14] resulting in functional and esthetic problems.[3] Implants don’t participate in the maxillary growth process of drift and displacement resulting in unpredictable implant dislocations, implant exposure because of bone resorption, limitation of jaw growth (maxilla) if implants are connected by a rigid prosthesis that crosses the midline,[14] infraocclusion relative to the adjacent natural dentition.[3,4,6,11] Adjacent tooth germs exhibit morphologic changes and disorders of eruption, however, in anodontic child this problem can be neglected.[3]
In the mandible, the transversal skeletal or alveolo-dental changes are less dramatic as in the maxilla.[3] As the lateral growth of the anterior mandible is usually completed by 3 years of age, implant placement can be considered if anodontia exists in this area. A limiting factor is the necessity to remake the prostheses to accommodate changes in the occlusal plane as the person matures.[6] In present case, implant therapy was not considered due to ongoing growth and development and insufficient alveolar bone support.
Conclusion
In this case report, prosthetic rehabilitation of a hypohidrotic ectodermal dysplasia with anodontia in a young patient was described. Early prosthetic treatment led to significant improvements in appearance, speech and masticatory function. Young ED patients should be recalled periodically for the prosthetic modification that is required due to continuing growth and development. The transitional prosthesis should be replaced by more definitive prosthesis once the skeletal growth is completed.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Kaul S, Reddy R. Prosthetic rehabilitation of an adolescent with hypohidrotic ectodermal dysplasia with partial anodontia: Case report. J Indian Soc Pedod Prev Dent 2008;26:177-81.
- Gupta S, Tyagi P. Prosthodontic management of anhidrotic ectodermal dysplasia. Indian J Dent Res 2011;22:348-51.
- Kramer F, Baethge C, Tschernitschek H. Implants in children with ectodermal dysplasia: A case report and literature Review. Clin Oral Impl Res 2007;18:140-6.
- Kearns G, Sharma A, Perrott D, Schmidt B, Kaban L, Vargervik K. Placement of endosseous implants in children and adolescents with hereditary ectodermal dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:5-10.
- Pigno MA, Blackman RB, Cronin RJ, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of the literature. J Prosthet Dent 1996;76:541-5.
- Guckes A, Scurria M, McCarthy G and Brahim J. Prospective clinical trial of dental implants in persons with ectodermal dysplasia. J Prosthet Dent 2002;88:21-5.
- Pinheiro M, Freire Maia N. Ectodermal dysplasias: A clinical classification and casual review. Am J Med Genet 1994;53:153-62.
- Tarjan I, Gabris K, Rozsa N. Early prosthetic treatment of patients with ectodermal dysplasia: A clinical report. J Prosthet Dent 2005;93:419-24.
- Ramos V, Giebink DL, Fisher JG, Christensen LC. Complete dentures for a child with hypohidrotic ectodermal dysplasia: A clinical report. J Prosthet Dent 1995;74:329-31.
- Guckes AD, McCarthy GR, Brahim J. Use of endosseous implants in a 3-year old child with ectodermal dysplasia: Case report and 5-year follow-up. Pediatr Dent 1997;19:282-5.
- Cronin RJ Jr, Oesterle LJ, Ranly DM. Mandibular implants and the growing patient. Int J Oral Maxillofac Implants 1994;9:55-62.
- Mascoutah, IL. Parameters of oral health care for individuals affected by ectodermal dysplasia syndromes. Muncie, Indiana: National Foundation for Ectodermal Dysplasias; 2003. p. 1-28.
- Tetsch P, Ackermann KL, Behneke N, Galandi M, Geis-Gerstorfer J, Kerschbaum TH, et al. Proceedings of a concensus conference on implantology, October 18,1989, Mains, West Germany. Int J Oral Maxillofac Implants 1990;5:182-7.
- Sennerby L, Odman J, Lekholm U, Thilander B. Tissue reactions towards titanium implants inserted in growing jaws: A histological study in the pig. Clin Oral Impl Res 1993;4:65-75.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.