RECONSTRUCTIVE TRIUMPH: ZYGOMATIC IMPLANT REHABILITATION FOLLOWING TOTAL MAXILLECTOMY IN NON-COVID MUCORMYCOSIS
Received: 31-Jan-2025, Manuscript No. Amhsr-24-160813; Editor assigned: 03-Feb-2025, Pre QC No. Amhsr-24-160813 (PQ); Reviewed: 17-Feb-2025 QC No. Amhsr-24-160813; Revised: 24-Feb-2025, Manuscript No. Amhsr-24-160813 (R); Published: 03-Mar-2025
Citation: Hota CC, et al. Reconstructive Triumph: Zygomatic Implant Rehabilitation Following Total Maxillectomy in Non-Covid Mucormycosis. Ann Med Health Sci Res. 2025; 1086-1089
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Mucormycosis is a rare but aggressive fungal infection requiring prompt intervention to prevent life-threatening complications. Non-COVID-related cases continue to present significant challenges in diagnosis and management. A 55-year-old male presented with facial swelling, nasal obstruction, and persistent pain in the maxillary region, significantly impacting his quality of life. Clinical examination and radiological investigations confirmed non-COVID mucormycosis with extensive maxillary involvement. The patient underwent total maxillectomy under general anesthesia to remove necrotic tissue, followed by reconstruction with zygomatic quad implants for functional and aesthetic rehabilitation. The surgical approach achieved successful infection control, with restoration of facial contours and oral function, leading to significant improvement in the patient’s overall well-being. Early diagnosis, aggressive surgical debridement, and advanced implant-based rehabilitation are crucial in managing extensive maxillary defects caused by mucormycosis. A multidisciplinary approach ensures optimal functional and aesthetic outcomes.
Keywords
Non-COVID mucormycosis; Total maxillectomy; Zygomatic implants; Maxillary rehabilitation; Fungal infection; Immunocompromised
Introduction
In recent Mucormycosis is an opportunistic fungal infection caused by the Mucorales order, commonly affecting immunocompromised patients [1-3]. It can lead to extensive tissue destruction, often necessitating radical surgical intervention such as total maxillectomy [4-6]. The resulting maxillary defect presents significant functional and aesthetic challenges. Zygomatic implants offer an effective rehabilitation option by anchoring prosthetic solutions in patients with insufficient maxillary bone [7-9]. This report discusses a case of non-COVID mucormycosis managed successfully with total maxillectomy followed by zygomatic quad implant placement.
Procedure
A 55-year-old male patient with past medical history of diabetes mellitus with no past history of COVID-19, presented to the Department of Oral and Maxillofacial Surgery with complaints of facial swelling, pain, and difficulty breathing. Radiographic and clinical examination confirmed the presence of an extensive fungal infection, diagnosed as non-COVID associated mucormycosis. The patient underwent a thorough preoperative evaluation, including blood tests, imaging studies (CT scan of the maxillofacial region), and histopathological examination of the affected tissues. The diagnosis of non-COVID mucormycosis was confirmed, and the decision was made to proceed with surgical intervention due to the aggressive nature of the infection.
Antifungal medication like Amphotericin B was administered intravenously prior to surgical procedures to prevent fungal infections. The patient was taken to the operating room, where general anesthesia was induced with appropriate monitoring and airway management. A secure airway was established via endotracheal intubation, and the patient was positioned supine with the head slightly elevated to allow optimal access to the maxillofacial region. The infected tissues, including necrotic bone and soft tissues, were identified through direct visualization. A total maxillectomy was performed, with complete removal of the maxilla, palatal mucosa, and surrounding infected structures to ensure complete excision of the necrotic tissue. Thorough haemostasis was achieved using electro-cautery and suture ligatures as necessary. The soft tissue was closed in layers, ensuring appropriate tension-free closure. The patient was monitored in the postoperative recovery area for any signs of complications, including infection, bleeding, or respiratory distress. Postoperative antibiotics were administered to prevent secondary bacterial infections, and antifungal therapy was continued as per the infectious disease team’s recommendations. The patient was advised to maintain regular follow-up visits to monitor the surgical site and assess for recurrence of the infection. On follow-up visits, the surgical site showed appropriate healing, with no signs of infection or recurrence of mucormycosis.
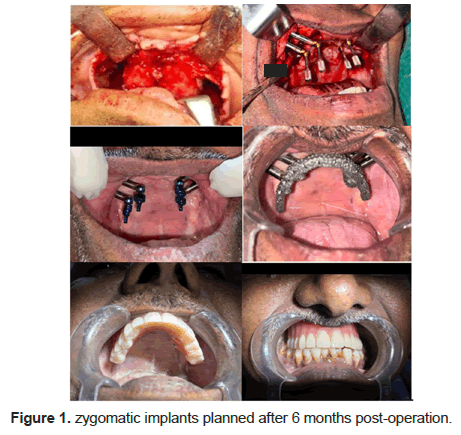
Maxillectomy rehabilitation using zygomatic implants planned after 6 months post-operation. Implant size is determined based on patient-specific anatomy, defect extent, and radiographic evaluation. After zygomatic implant placement, precise impressions capture the implant positions, enabling accurate prosthesis fabrication. A custom titanium framework is designed to ensure stability and support for the prosthesis. Trial fittings are conducted to assess fit, aesthetics, and function, allowing adjustments as needed. The final prosthesis, crafted with durable acrylic teeth and gingival components, restores aesthetics, speech, and mastication. This comprehensive approach ensures functional and cosmetic success, enhancing the patient’s quality of life (Figure 1).
Literature Review
This Mucormycosis is a rare but aggressive fungal infection caused by molds of the order Mucorales, predominantly affecting immunocompromised individuals. While the COVID-19 pandemic led to a surge in mucormycosis cases due to viral-induced immune suppression and prolonged corticosteroid use, non-COVID-related mucormycosis continues to be a significant concern, particularly in patients with uncontrolled diabetes mellitus and other immunosuppressive conditions [10]. The disease progresses rapidly, often involving the paranasal sinuses, maxilla, orbit, and brain, leading to significant morbidity and mortality if not diagnosed and managed promptly [11].
Non-COVID mucormycosis shares similar clinical manifestations with COVID-Associated Mucormycosis (CAM), but the underlying causes differ [12]. While CAM is primarily linked to factors such as prolonged corticosteroid use, hyperglycemia, and immune suppression associated with SARS-CoV-2 infection, non-COVID mucormycosis arises in individuals with metabolic disorders, hematological malignancies, or those undergoing immunosuppressive therapy. The management of mucormycosis involves antifungal therapy and aggressive surgical debridement, with maxillectomy being a common procedure to remove necrotic tissue and control disease progression.
Maxillectomy, however, leads to extensive functional and aesthetic deficits, significantly affecting the patient's quality of life. The loss of maxillary bone impacts mastication, speech, and facial appearance, making prosthetic rehabilitation a complex challenge [13]. Traditional methods, such as removable dentures and obturators, often fail to provide adequate retention and stability, especially in patients with severe maxillary resorption. Conventional dental implants require sufficient bone volume for successful placement, which is often compromised in post-maxillectomy patients.
Zygomatic implants have emerged as a reliable alternative for the rehabilitation of patients with severe maxillary bone loss. These implants anchor into the dense zygomatic bone, bypassing the need for bone grafting and enabling immediate prosthetic loading [14]. This approach not only reduces treatment time but also improves patient comfort and functional outcomes. The quad-cortical stabilization mechanism of zygomatic implants enhances primary stability, making them an ideal choice for complex maxillary reconstructions, including post-maxillectomy rehabilitation.
This study presents a case of non-COVID-related mucormycosis necessitating maxillectomy, followed by successful prosthetic rehabilitation using zygomatic implants [15]. The biomechanical advantages, high survival rates, and long-term success of these implants highlight their significance in restoring function and aesthetics in patients with extensive maxillary defects. By eliminating the need for bone grafting and providing a stable foundation for prosthesis placement, zygomatic implants offer a predictable and durable solution for maxillary rehabilitation.
Mucormycosis is an opportunistic fungal infection caused by molds belonging to the order Mucorales, particularly Zygomycetes. This aggressive disease primarily affects immunocompromised individuals, with uncontrolled diabetes mellitus being a significant risk factor. It progresses rapidly, often invading the paranasal sinuses, maxilla, orbit, and brain, necessitating prompt diagnosis and intervention to prevent fatal outcomes [10]. The disease has gained considerable attention due to the surge in cases during the COVID-19 pandemic, where COVID-Associated Mucormycosis (CAM) became a major complication among patients recovering from severe viral infections.
The increased incidence of CAM was attributed to several factors, including prolonged corticosteroid use, immune dysregulation caused by SARS-CoV-2, and uncontrolled diabetes. Unlike non-COVID mucormycosis, which primarily affects individuals with chronic metabolic disorders and immunosuppressive conditions, CAM developed in patients who had no prior history of immunodeficiency but acquired it due to the systemic effects of the viral infection and its treatment. Despite the differences in etiology, both forms of mucormycosis share similar clinical presentations and require aggressive management involving antifungal therapy and surgical debridement.
Maxillectomy is a widely performed surgical intervention for extensive mucormycosis cases, particularly when the infection involves the maxilla and adjacent structures. However, this procedure results in significant functional and aesthetic deficiencies, affecting speech, mastication, and facial appearance. The rehabilitation of post-maxillectomy patients remains a major challenge due to the severe loss of maxillary bone, making conventional prosthetic solutions inadequate. Traditional removable prostheses often lack stability and retention, particularly in patients with extensive maxillary
Dental implants have revolutionized prosthetic rehabilitation by providing a fixed alternative to removable dentures. However, conventional implant placement is often unfeasible in maxillectomy cases due to the extensive loss of maxillary bone. In such situations, zygomatic implants offer a viable solution by anchoring into the dense zygomatic bone, bypassing the need for bone grafting and providing a stable foundation for prosthetic rehabilitation. These implants facilitate immediate prosthetic loading, improving functional and aesthetic outcomes while reducing treatment time and patient discomfort.
The use of zygomatic implants has expanded over time, making them a preferred choice for patients with severe maxillary atrophy and post-maxillectomy defects. Their quad-cortical stabilization mechanism ensures high primary stability, resistance to micromovement, and efficient load distribution, making them a predictable and long-term solution for complex maxillary reconstructions. By eliminating the need for additional bone augmentation procedures, zygomatic implants significantly enhance the efficiency and success of maxillary rehabilitation.
This article discusses a case of non-COVID-related mucormycosis requiring maxillectomy, followed by successful rehabilitation using zygomatic implants. The biomechanical advantages and clinical outcomes of these implants highlight their role in restoring function and quality of life in patients with extensive maxillary defects. The study further explores the indications, surgical pathway, and long-term success of zygomatic implants, emphasizing their importance in modern maxillofacial rehabilitation.
Implant-supported rehabilitation of the maxilla represents a significant surgical challenge when bone volumes are inadequate for the placement of conventional implants. Various treatment modalities have been explored to address this issue. Patients often face prolonged treatment durations, significant morbidity from donor harvest sites, and increased costs associated with biomaterials. Additionally, prosthodontic rehabilitation may be delayed when primary stability is not achieved or when hard tissue reconstruction is required before implant placement. These challenges can serve as barriers to care that could otherwise improve patient’s quality of life.
The use of the zygoma as an anchorage site was first explored by Brånemark in 1988, utilizing customized, increased-length conventional implants. This technique was first reported in the literature by Aparicio, who stabilized a graft in the pre-maxilla using the zygomatic process of the maxilla for anchorage. Zygomatic Implants (ZIs) provide an opportunity to bypass the need for hard tissue regeneration and reduce treatment timelines. Over time, ZI designs have evolved to meet growing clinical demands, including oncologic resections, trauma rehabilitation, and the retention of obturators or use in combination with free flap reconstructions.
Zygomatic implants are indicated in cases where conventional implant placement is not feasible due to inadequate bone volume, including severe posterior maxillary resorption, extensive bone loss from trauma, and oncologic resections. Treatment modalities involve splinting ZIs to conventional implants in the anterior maxilla or utilizing a quad zygoma approach for fixed or removable prosthetic reconstructions. Initially, a two-stage approach was preferred, but immediate loading has gained popularity due to improved survival outcomes. The Anterior-Posterior (AP) spread for prosthetic reconstruction can be enhanced in cases of significantly pneumatised sinuses, where options for tilted implants are limited [16].
Traditional rehabilitation of the atrophic maxilla has relied on extensive bone grafting procedures, including iliac crest grafts, Le Fort I osteotomies, and maxillary sinus lifts. These procedures pose multiple challenges, such as the need for multiple surgical interventions, morbidity associated with extraoral donor sites, and prolonged rehabilitation periods [17]. Zygomatic implants have emerged as an effective alternative by utilizing the zygomatic bone for anchorage, eliminating the need for bone grafting while reducing overall treatment time.
When considering zygomatic implant rehabilitation, the patient must exhibit posterior alveolar crest resorption that precludes conventional implant placement. Additionally, sufficient bone volume in the anterior maxilla at least 10 mm in height and 4 mm in width is required for the placement of 2-4 conventional implants. In cases where anterior maxillary bone volume is insufficient, conditions must be favorable for onlay bone grafting or Guided Bone Regeneration (GBR) techniques [18]. Maxillary sinus lift procedures remain a predictable option for implant placement, but they require a suitable bone donor site, which may be intraoral (chin, mandibular ramus, or retromolar trigone) or extraoral (iliac crest, skull, or tibia). Depending on residual bone volume and quality, maxillary sinus lift and implant placement may be performed in one or two phases. When primary implant stability is unattainable, bone grafting is performed first, followed by implant placement after six months.
Clinical studies have highlighted the limitations of traditional bone grafting techniques. Lekholm et al. conducted a multicenter retrospective study with a three-year follow-up of 150 edentulous maxillae treated with various grafting techniques. The study reported a 23% failure rate for implants placed simultaneously with bone grafting and a 10% failure rate for implants placed in a two-stage procedure. Keller et al. presented 12-year follow-up results for inlay autologous bone grafts used in maxillary reconstruction, reporting an 87% implant survival rate and 95% prosthetic function success. Despite the high success rates, the need for multiple interventions and prolonged treatment durations remains a drawback [19].
The introduction of zygomatic implants has streamlined the rehabilitation of atrophic maxillae by reducing surgical interventions and shortening treatment timelines. Various authors have documented the use of zygomatic implants in the functional and esthetic reconstruction of palatal deformities, post-maxillectomy defects, and developmental anomalies like ectodermal dysplasia, yielding satisfactory outcomes.
Recent studies evaluating zygomatic implant survival rates have shown promising results. A study assessing 101 zygomatic implants placed in highly resorbed maxillae reported a survival rate spanning 1-72 months. These findings reinforce the reliability of zygomatic implants as an alternative to extensive grafting procedures, providing predictable long-term results for patients requiring maxillary reconstruction. However, complications such as sinus pathology and oro-antral communications must be considered [20].
Overall, zygomatic implants represent a transformative approach in maxillary rehabilitation, offering high survival rates, immediate-loading capabilities, and enhanced prosthetic outcomes while minimizing the need for extensive grafting procedures. Further long-term studies are warranted to evaluate patient-reported outcomes and optimize treatment protocols.
Conclusion
In conclusion, this case demonstrates the effective management of non-COVID mucormycosis using a multidisciplinary approach, combining maxillectomy and rehabilitation with zygomatic implants. Early diagnosis, timely surgical intervention, and tailored prosthetic rehabilitation were instrumental in achieving favourable outcomes. This approach aligns with the growing body of evidence supporting zygomatic implants in complex cases of maxillary defects. By integrating expertise from multiple disciplines, the treatment paradigm outlined in this case can serve as a model for addressing similarly challenging clinical scenarios.
References
- Hernández JL, Buckley CJ. Mucormycosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2025.
- Sharma A, Goel A. Mucormycosis: Risk factors, diagnosis, treatments, and challenges during COVID-19 pandemic. Folia Microbiol (Praha). 2022;67(3):363-387.
[Crossref] [Google Scholar] [PubMed]
- Azhar A, Khan WH, Khan PA, Alhosaini K, Owais M,et al. Mucormycosis and COVID-19 pandemic: Clinical and diagnostic approach. J Infect Public Health. 2022;15(4):466-479.
[Crossref] [Google Scholar] [PubMed]
- Minase DA, Sathe S, Borle A, Mundada BP, Doshi K. Zygomatic Implants in a Patient With History of Mucormycosis: A Case Report. Cureus. 202;16(7):e65512.
[Crossref] [Google Scholar] [PubMed]
- Narita N, Ito R, Mimura M, Oyama T, Tanaka Y, et al. Comparative study for closure methods of maxillary defects after maxillectomy, a free flap versus a maxillary obturator. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology. 2021;33(1):39-42.
- Aparicio C, Manresa C, Francisco K, Claros P, Alández J, et al. Zygomatic implants: indications, techniques and outcomes, and the zygomatic success code. Periodontol. 2014;66(1):41-58.
[Crossref] [Google Scholar] [PubMed]
- Kumar L, Verma A, Pal US, Mattoo K, Algarni YA, et al. Influence of prosthodontic rehabilitation using zygomatic implants in Covid 19 related mucormycosis (rhino–orbital–cerebral) maxillectomy patients upon post-operative stress, anxiety and functional impairment: A prospective cohort study. Clinical Interventions in Aging. 2023:1201-19.
[Crossref] [Google Scholar] [PubMed]
- Yadav S, Sharma A, Kothari N, Bhatia PK, Goyal S, et al. Mucormycosis: A Case Series of Patients Admitted in Non-COVID-19 Intensive Care Unit of a Tertiary Care Center during the Second Wave. Indian J Crit Care Med. 2021;25(10):1193-1196.
[Crossref] [Google Scholar] [PubMed]
- Salem AA, Shakel EA, Sadakha AA, Kassem EM, El-Segai AA. Evaluation of Zygomatic implant retained obturator in rehabilitation of partial palato-maxillectomy patients. Tanta Dental Journal. 2015;12(1):35-40
- Balushi AA, Ajmi AA, Sinani QA, Menon V, Berieki ZA, et al. COVID-19-associated mucormycosis: An opportunistic fungal infection. A case series and review. Int J Infect Dis. 2022;121:203–10.
[Crossref] [Google Scholar] [PubMed]
- kothari N, Goyal A, Sharma A, Goyal S, Bhatia PK, Yadav S. Mucormycosis: A case series of patients admitted in non-COVID-19 intensive care unit of a tertiary care center during the second wave. Indian J Crit Care Med [Internet]. 2022;25(10):1193–6.
[Crossref] [Google Scholar] [PubMed]
- AK, Gupta V. Rhino-orbital cerebral mucormycosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
- Ramezanzade S, Yates J, Tuminelli FJ, Keyhan SO, Yousefi P, et al. Zygomatic implants placed in atrophic maxilla: an overview of current systematic reviews and meta-analysis. Maxillofac Plast Reconstr Surg. 2021;43(1):1
[Crossref] [Google Scholar] [PubMed]
- Bedrossian E, Brunski J, Al-Nawas B, Kämmerer PW. Zygoma implant under function: biomechanical principles clarified. Int J Implant Dent. 2023;9(1).
[Crossref] [Google Scholar] [PubMed]
- Wu Y, Tao B, Lan K, Shen Y, Huang W, et al. Reliability and accuracy of dynamic navigation for zygomatic implant placement. Clin Oral Implants Res. 2022;33(4):362-376.
[Crossref] [Google Scholar] [PubMed]
- Vosselman N, Glas HH, Merema BJ, Kraeima J, Reintsema H, et al. Three-Dimensional Guided Zygomatic Implant Placement after Maxillectomy. J Pers Med. 2022;12(4):588.
[Crossref] [Google Scholar] [PubMed]
- Aparicio C, Olivo A, de Paz V, Kraus D, Luque MM, et al. The zygoma anatomy-guided approach (ZAGA) for rehabilitation of the atrophic maxilla. Clin Dent Rev [Internet]. 2022;6(1).
[Crossref] [Google Scholar] [PubMed]
- Tzerbos F, Bountaniotis F, Theologie-Lygidakis N, Fakitsas D, Fakitsas I. Complications of Zygomatic Implants: Our Clinical Experience with 4 Cases. Acta Stomatol Croat. 2016;50(3):251-257
[Crossref] [Google Scholar] [PubMed]
- Brennand Roper M, Vissink A, Dudding T, Pollard A, Gareb B, et al. Long-term treatment outcomes with zygomatic implants: a systematic review and meta-analysis. Int J Implant Dent.
[Crossref] [Google Scholar] [PubMed]
- Hackett S, El-Wazani B, Butterworth C. Zygomatic implant-based rehabilitation for patients with maxillary and mid-facial oncology defects: A review. Oral Dis. 20221;27(1):27-41.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.