Refining the Journal Club Presentations of Postgraduate Students in Seven Clinical Departments for Better Evidence‑based Practice
- *Corresponding Author:
- Dr. Anita Herur,
Department of Physiology, S. Nijalingappa Medical College, Navanagar, Bagalkot - 587 102, Karnataka, India.
E-mail: dranitaherur@yahoo.co.in
Citation: Herur A, Kolagi S, Ramadurg U, Hiremath CS, Hadimani CP, Goudar SS. Refining the journal club presentations of postgraduate students in seven clinical departments for better evidence-based practice. Ann Med Health Sci Res 2016;6:185-9.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: A gap between best practice and actual clinical care exists and this can be overcome by evidence‑based practice (EBP), which is essential to improve the clinical decision making. A strategy to reduce deficits in care provision is to train the postgraduate students in the practice of EBP in the journal clubs as evidence from medical colleges in India reveals that current format of journal club presentations is unsatisfactory. Aim: The aim of the present study was to refine the journal club presentations of postgraduate students of clinical departments and to study the effectiveness of EBP training in them for better EBP. Subjects and Methods: This study was conducted in S. Nijalingappa Medical College, Bagalkot, Karnataka, India, and it was a pre‑ and post‑trial. This study was a pre‑ and post‑trial done during the journal club presentations of postgraduate students from clinical departments. Postgraduate students’ understanding of concepts about EBP was assessed using Fresno test questionnaire in traditional journal club presentation. A hands‑on session incorporating steps of EBP was imparted to them. Soon after the session, each student was assessed. In the next journal club presentation, 1 week later, the students were assessed again with the same questionnaire by the same faculty. Scores of the postgraduate students, before and after intervention (immediate and 1 week later), were compared. Data were analyzed by paired t‑test using SPSS. Results: An increase in mean posttest scores was seen immediately and also 1 week later as compared to the pretest scores. The scores also increased significantly, when each step of EBP was considered. Conclusions: Incorporating teaching of EBP in journal club presentations improved the competencies of postgraduate students in clinical decision making.
Keywords
Evidence‑based practice, Journal club, Postgraduate training
Introduction
The World Federation of Medical Education has proposed an- international framework for quality of postgraduate medical- education and developed global standards.[1] In line with this,- the medical council of India laid down the general objectives of- postgraduate training which included training them in research- methodology, critical appraisal, ethics, self‑directed learning,- and making them clinically competent.[2]
A gap between best practice and actual clinical care exists- and this can be overcome by evidence‑based practice (EBP),- which is essential to improve the clinical decision making.- Evidence‑based clinical guidelines have become a major- feature of health care provision to bridge the gap between- best evidence and clinical care. However, studies suggest that- clinical use of these guidelines does not occur that between 10 and 40% of patients do not receive care based on current- scientific evidence and that ≥20% of care provided is not- needed or is potentially harmful to the patients.[3,4] A strategy to- reduce these deficits in care provision is to increase the number- of EBP training programs;[5] their goal being to improve- outcomes for patients by increasing postgraduate health care- knowledge, skills, and attitudes toward EBP.[6]
“Evidence‑based medicine” was coined and defined by Sackett- et al. in 1996 as “the conscientious, explicit, and judicious use- of the current best evidence in making decisions about the care- of individual patients.” This became EBP, as the principles- and process were adopted by many disciplines in health and- social care.[7]
The EBP process can be considered as a series of steps:[7]
1. Ask practice‑focused questions, and frame the questions- to find an answer
2. Search, identify, and access the potential evidence
3. Evaluate the quality of evidence and decide what is best- evidence
4. Apply the best evidence to the specific case
5. Evaluate the EBP care provided, and the processes by which- care decisions were reached.
The first step of EBP, i.e., formulating a focused answerable- question can be done using PICO model:
• P = Patient/patient’s problem
• I = Intervention/investigation intended
• C = Comparison intervention/investigation
• O = Outcome (patient‑oriented).
Having defined the question, the next step is to locate all the- evidence from the literature that may be pertinent. One of the- most cited hierarchies of evidence is that by Guyatt et al. at- the highest level are the systematic reviews and meta‑analyses,- followed by randomized controlled trials with definitive results,- randomized controlled trials with nondefinitive results, cohort- studies, case–control studies, cross‑sectional studies, and at the- lowest level are the case reports.[7]
The third step, being the critical appraisal, is a judgment about- what is the best evidence available and is it valid, reliable,- and applicable. The fourth step ensures that the evidence- is applicable to the practice context, and the final step is to- evaluate the EBP care provided, the processes by which care- decisions were reached and to update our knowledge.[7]
Journal Clubs are a part of the postgraduate medical education- of all disciplines. They have been used to teach critical- appraisal, research designs, and biostatistics and to improve- reading habits.[8,9] In recent times, they have been seen as a- mechanism for overcoming barriers associated with EBP.[10]- In traditional models of journal clubs, the presenter chooses- an article at random and summarizes the article in terms of- the authors’ results and conclusions. Most presenters do not appraise the quality of studies. The articles discussed are- not necessarily relevant to clinical practice; hence, there is a- decline in the attendance.[11] Evidence from Indian medical- college also reveals that the current format of journal club- presentations is unsatisfactory.[12]
In one study, the journal club at a university‑based residency- program was restructured to introduce, reinforce, and evaluate- residents’ understanding of the concepts of EBP. The authors- developed pre‑ and post‑tests for use during each Journal Club,- which showed significant improvement, better understanding,- and utilization of the concepts of EBP.[13]
Only two validated assessment tools have been developed- to specifically assess all aspects of EBP competence. Of- the two tools, Berlin and Fresno tools, only the Fresno tool- comprehensively assesses EBP competency across all relevant- domains.[14‑16]
There is no evidence in the Indian literature, to the best of- our knowledge, of training postgraduate students in EBP in- journal clubs. Hence, the present study was undertaken to- refine the journal club presentations of postgraduate students- of clinical departments and to study the effectiveness of EBP- training in them for better EBP. The objectives set forth- for the students were that at the end of the EBP training- session, the postgraduate student should be able to perform- all the steps of EBP, as assessed by Fresno questionnaire- and rating scale.
Subjects and Methods
Study design and setting
This study was a longitudinal pre‑ and post‑trial conducted at- S. Nijalingappa Medical College, Bagalkot, Karnataka, India.
All the postgraduate students (n = 30) from clinical- departments were included in the study, namely students- from the Departments of General Medicine (n = 4), General- Surgery (n= 4), Obstetrics and Gynecology (n = 4),- Pediatrics (n = 5), Ophthalmology (n = 5), Anesthesia (n = 4),- Orthopedics (n = 2), ENT (n = 1), and Dermatology (n = 1).
Ethical issues
Ethical clearance was obtained from the institution and- informed consent from all the postgraduate students.
Procedure and intervention
This study was done on thirty clinical postgraduate students.- The postgraduate students’ understanding of the concepts about- EBP was assessed using a validated Fresno test questionnaire [17]- in the traditional journal club presentation. A hands‑on session- incorporating all the steps of EBP was imparted to them.- Students were trained in formulating a pertinent, focused and- answerable question using problem, intervention, comparisons, and outcomes (PICO) model. They were also involved- hands‑on in the various means of literature search to find the- best evidence and critically appraise the evidence searched.- Later, they were trained in making a clinical decision based on- the evidence searched, using clinical scenarios. Soon after the- session, each student was assessed by a faculty who was trained- in EBP and its evaluation. In the next journal club presentation,- 1 week later, the students were assessed again with the same- questionnaire by the same faculty. Scores of the postgraduate- students, before and after intervention (immediate and 1 week- later), were compared with respect to each department. Further,- a cumulative data from all the departments was also obtained- statistically.
Statistical analysis
Data were analyzed by paired t‑test and Pearson’s correlation- using SPSS version 20.0 (IBM, Armonk, NY). P < 0.05 was- considered as significant.
Results
The total number for participants was thirty, among which- 19 were male and 11 female students. The mean age in years- was 27.9 (3.7).
An increase in the mean posttest scores was seen in all steps- immediately and also 1 week later as compared to the pretest- scores. The posttest scores taken after 1 week, however,- deteriorated as compared to the posttest scores obtained- immediately after the session [Table 1].
| Fresno test scores | Pretest (I) | Posttest 1 (II) | Posttest 2 (III) | t and P | t and P for | t and P for |
|---|---|---|---|---|---|---|
| for I and II | I and III | II and III | ||||
| Overall score (steps 1+2+3) | 20.40 (8.76) | 93.53 (13.66) | 71.83 (12.42) | -29.30 | -22.05 | 38.64 |
| (maximum score=121) | <0.001* | <0.001* | <0.001* | |||
| Step 1 (EBP question) | 0.47 (0.73) | 2.90 (0.30) | 2.43 (0.67) | -14.84 | -10.10 | 3.50 |
| (maximum score=3) | <0.001* | <0.001* | <0.01* | |||
| Step 2 (literature search) | 6.30 (2.79) | 12.00 (2.01) | 11.07 (2.08) | -13.71 | -10.16 | 3.61 |
| (maximum score=14) | <0.001* | <0.001* | <0.01* | |||
| Step 3 (critical appraisal) | 13.63 (7.03) | 78.63 (13.53) | 58.33 (12.08) | -25.68 | -19.48 | 40.90 |
| (maximum score=104) | <0.001* | <0.001* | <0.001* | |||
| Step 4 (application of evidence) | 1.93 (0.86) | 4.83 (0.37) | 4.63 (0.49) | -19.78 | -16.15 | 1.98 |
| (5-point Likert scale) | <0.001* | <0.001* | 0.056 | |||
| EBP rating (5-point Likert scale) | 4.03 (1.09) | 4.60 (0.56) | 4.63 (0.49) | -2.48 | -2.75 | -0.25 |
| <0.01* | <0.01* | 0.801 |
*Statistically significant, EBP: Evidence-based practice
Table 1: Fresno test questionnaire overall scores and scores in each step of evidence-based practice.
The pretest, immediate posttest, and 1 week later posttest- scores are depicted as a mean (SD) in Table 1 (overall and split- step‑wise) and Table 2 (department‑wise scores).
| Department | Pretest (I) | Posttest 1 (II) | Posttest 2 (III) | t and P | t and P for | t and P for |
|---|---|---|---|---|---|---|
| for I and II | I and III | II and III | ||||
| Medicine + Dermatology (n=5) | 20.80 (12.25) | 88.80 (10.70) | 67.40 (10.23) | -12.71 | -9.25 | 35.66 |
| <0.001* | <0.01* | <0.001* | ||||
| Surgery (n=4) | 25.75 (4.19) | 102.00 (9.48) | 80.75 (6.39) | -13.03 | -13.27 | 12.14 |
| <0.01* | <0.01* | <0.01* | ||||
| Obstetrics and Gynecology (n=4) | 21.00 (9.59) | 99.75 (17.72) | 77.00 (17.35) | -7.36 | -5.25 | 47.52 |
| <0.01* | <0.01* | <0.001* | ||||
| Pediatrics (n=5) | 14.40 (8.41) | 81.00 (3.67) | 62.20 (2.49) | -20.59 | -12.24 | 19.39 |
| <0.001* | <0.001* | <0.001* | ||||
| ENT + Ophthalmology (n=6) | 21.00 (4.56) | 96.83 (11.95) | 71.83 (11.33) | -19.14 | -13.23 | 17.39 |
| <0.001* | <0.001* | <0.001* | ||||
| Orthopedics + Anesthesia (n=6) | 20.50 (11.04) | 94.83 (17.64) | 74.17 (16.41) | -9.54 | -7.44 | 21.65 |
| <0.001* | <0.01* | <0.001* |
*Statistically significant. ENT: Ear, nose, and throat
Table 2: Department-wise distribution of the Fresno test questionnaire overall scores.
The scores increased significantly when each step of EBP- was considered. Scores of the students from every department- showed a positive change; highest scores were seen in the- students from the Department of Surgery [Table 2].
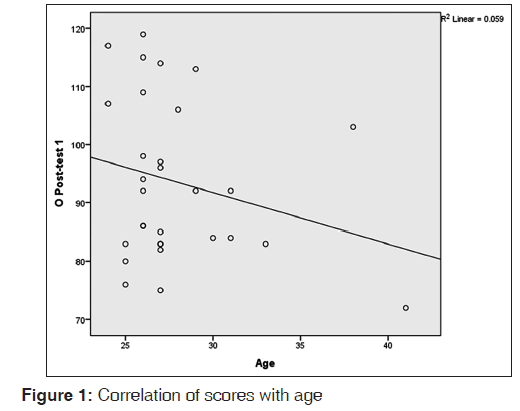
There was also no correlation between the scores and- age [Figure 1].
Discussion
The results of the present study reveal the beneficial effects of- training the postgraduate students in the practice of EBP during- their journal clubs. A very low mean pretest score on the Fresno- questionnaire indicates the ignorance of the students toward the steps of EBP. But, a considerably high score obtained on rating- EBP as an important tool for clinical decision making, makes- us aware of the fact that the postgraduate students realize the- importance of EBP. Most of the students performed well in- Steps 1, 2, and 4 but lacked in Step 3. Students formulated a- pertinent, focused and answerable question using PICO model.- They could demonstrate the various means of literature search- to find the best evidence with not much of difficulty. They- could also make a clinical decision based on the evidence- searched. As Step 3 involves a critical appraisal of the evidence- including biostatistics, majority of them found the calculation- of statistical parameters difficult to remember and understand.- This was one of the main reasons for a significant deterioration- of the posttest scores after 1 week in Step 3.
All the students were benefitted from the EBP session, but- most benefitted were from the Department of Surgery. Age- did not affect the process of learning as evident by Pearson’s- correlation. It would not be appropriate to reason out such- benefits as the sample size was small when each department- or the age group was considered.
In traditional models of journal clubs, the presenter or the- moderator of the journal club chooses an article at random- which may not be clinically relevant. This would result in a- decline in the attendance and also interest in the journal clubs.[11]- Most of the articles are just read and not critically appraised.[11]- The results of the present study are similar to a study in which- the journal club was restructured to introduce, reinforce, and- evaluate residents’ understanding of the concepts of EBP. The- authors here developed pre‑ and post‑tests for use during each- journal club, which showed significant improvement, better- understanding, and utilization of the concepts of EBP.[13]
As a part of the present study, training was also imparted to a- few selected faculty members prior to this postgraduate session- for better compliance in continuing the practice of EBP in the- journal clubs. The faculty members were happy and keen in- learning the steps of EBP and assured that they would use the journal clubs as platforms for the practice of EBP and also- formulate some practice guidelines for the department.
At the end of the training, all the postgraduate students expressed- great pleasure in having learned the steps of EBP which would- help them in clinical decision making and above all the journal- clubs would be more fruitful henceforth in making use of the- daily patient encounters to formulate a focused question, search- the literature for appropriate evidence, critically appraise that- evidence, and finally apply it to the patient.
The limitation of the present study was the small sample size- when each department was considered and due to the small- sample size, a stronger study design, such as randomized- controlled trial (RCT) with cross‑over could not be done.- However, the information generated is very relevant for post- graduate medical education
Conclusions and Implications
It can be concluded that incorporating the teaching of EBP in- journal club presentations has improved the competencies of- the postgraduate students in clinical decision making, thereby- refined the journal clubs by making them more effective and- relevant in clinical practice.
Scope for future research
Future research can be directed toward having a study with- large sample size involving multiple centers, for which an- RCT with cross‑over can be designed. The results obtained- can also be compared and correlated with the anxiety scores- of the postgraduate students.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Postgraduate Medical Education. WFME Standards for Quality Improvement. Available from: http://www.wfme. org/. [Last cited on 2012 Oct 29].
- Medical Council of India. Postgraduate Medical Education Regulations; 2000 (Amended UPTO MARCH 2012). Available from: http://www.mciindia.org/RulesandRegulations/PGMedicalEducationRegulations2000.aspx. [Last cited on 2012 Oct 29].
- Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients? care. Lancet2003;362:1225-30.
- Leape LL, Weissman JS, Schneider EC, Piana RN, Gatsonis C,Epstein AM. Adherence to practice guidelines: The role ofspecialty society guidelines. Am Heart J 2003;145:19-26.
- Hatala R, Guyatt G. Evaluating the teaching of evidence-basedmedicine. JAMA 2002;288:1110-2.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB,Richardson WS. Evidence based medicine: What it is andwhat it isn?t. BMJ 1996;312:71-2.
- Cluett ER, Bluff R. Principles and Practice of Research in Midwifery. 2nd ed.. London, UK: Churchill Livingstone; 2006. p. 34-51.
- Ebbert JO, Montori VM, Schultz HJ. The journal club in postgraduate medical education: A systematic review. Med Teach 2001;23:455-61.
- Khan K, Dwarakanath LS, Pakkal M, Brace V, Awonuga A.Postgraduate journal club as a means of promoting evidence-based obstetrics and gynaecology. J Obstet Gynaecol Can 1999;19 Suppl 3:231-4.
- Goodfellow LM. Can a journal club bridge the gap between research and practice? Nurse Educ 2004;29:107-10.
- Khan K, Gee H. A new approach to teaching and learning in journal club. Med Teach 1999;21 Suppl 3:289-93.
- Saroshe S, Khandelwal V, Mehta SC. Perceived utility of journal club by residents of a private medical college of central India. Indian J Community Health 2012;24:243-7.
- Cramer JS, Mahoney MC. Introducing evidence based medicine to the journal club, using a structured pre and post test: A cohort study. BMC Med Educ 2001;1:6.
- Ramos KD, Schafer S, Tracz SM. Validation of the Fresno test of competence in evidence based medicine. BMJ 2003;326:319-21.
- Shaneyfelt T, Baum KD, Bell D, Feldstein D, Houston TK, Kaatz S, et al. Instruments for evaluating education in evidence-based practice: A systematic review. JAMA 2006;296:1116-27.
- Ilic D. Assessing competency in evidence-based practice: Strengths and limitations of current tools in practice. BMC Med Educ 2009;9:53.
- Ramos KD. Fresno Test of Evidence Based Medicine. Available from: http://www.uthscsa.edu/gme/documents/PD%20Handbook/EBM%20Fresno%20Test%20grading%20rubric.pdf. [Last cited on 2012 Oct 29].




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.