Rehabilitation of Atrophic Maxilla with Zygomatic Implants-Case Report on Extra Sinus Approach Zygomatic Implants
Received: 07-May-2020, Manuscript No. AMHSR-23-10435; Editor assigned: 12-May-2020, Pre QC No. AMHSR-23-10435 (PQ); Reviewed: 26-May-2020 QC No. AMHSR-23-10435; Revised: 19-Jul-2023, Manuscript No. AMHSR-23-10435 (R); Published: 16-Aug-2023
Citation: Ahmed SE. Rehabilitation of Atrophic Maxilla with Zygomatic Implants-Case Report on Extra Sinus Approach Zygomatic Implants. Ann Med Health Sci Res. 2023;13:762-768.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The successful treatment of patients with implants has signi icantly in luenced restorative dentistry treatment planning, with a success rate above 90%. Implant supported prostheses for replacing missing teeth are an established treatment option with favourable success and patient acceptance rates, that are available to us today, but there are certain areas and situations where the placement and restoration is technique sensitive. Insu icient height and/or width of the alveolar ridge when placing implants for oral rehabilitation in the atrophied maxilla is a challenge.
Keywords
Patient; Dentistry treatment; Alveolar ridge; Oral rehabilitation
Introduction
Restoration of posterior maxilla with conventional dental implants is often jeopardised due to various reasons such as excessive bone resorption, poor quality of bone and pneumatisation of the maxillary sinus.
To overcome these problems, many surgical techniques to increase the bone volume have been employed. The techniques to increase the bone volume include onlay bone grafting and grafting of the maxillary sinus with autogenous bone or bone substitute. These procedures are either complex or time consuming. So to avoid these complex procedures, different therapeutic treatments options were developed which include placement of implants in the pterygoid and zygoma. The placement of implants in the zygomatic bone as an alternative option in the rehabilitation of the atrophic maxilla is considered nowdays [1].
Branemark performed the original protocol of placing the zygomatic implants. The zygomatic implants were placed intrasinusly in this technique. Stella and Warner later introduced the sinus slot technique of zygomatic implant placement. The other technique of placing zygomatic implants is extra sinus approach. This case study describes the prosthetic rehabilitation of the atrophic maxilla with zygomatic implants placed in extra sinus approach [2].
Case Presentation
Diagnostic and pre-operative phase
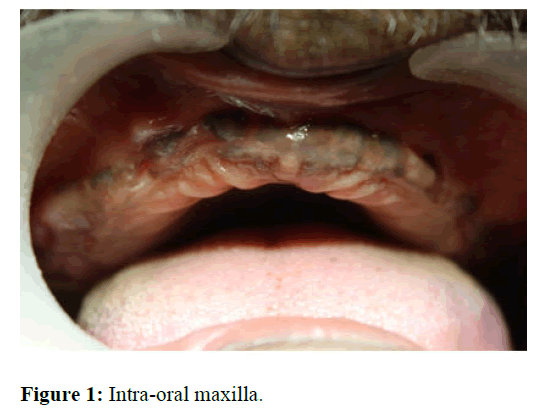
Patient aged 58 years reported to the clinical section of department of prosthodontics with a chief complaint of missing teeth in relation to both upper and lower arches (Figure 1). Patient gave history of ill-fitting complete dentures in both upper and lower arches. Clinical examination revealed completely edentulous maxillary and mandibular arches with adequate bone width in both the arches. The arch form and shape of maxilla and mandibular arches were U and V shape respectively. After examining the intra oral features, it was found that the vestibular depth was minimal in both the arches. To investigate the available bone height Ortho Pantomo Graph (OPG) was advised to the patient. Orthopantamograph (OPG) revealed adequate bone height in anterior and posterior regions of mandibular whereas in maxilla the bone height in the anterior region was adequate and in the posterior region it was inadequate. This discrepancy in the bone height in maxilla can be due to the pneumatisation of the maxillary sinus and amount of bone resorption in posterior region of maxilla.
After analysing the past history and intra oral features including the bone height and width it was concluded that, implant supported complete denture prostheses is the best treatment option for the patient. Since the bone height in the posterior region of maxilla was insufficient for placing implants, options such as on lay bone grafting over the posterior region of maxilla were discussed. Patient was not interested in such extensive surgical procedures and wanted the prostheses in shorter duration of time, so it was decided to place bilateral zygomatic implants in the posterior region, two axial implants in the anterior region in maxilla and later rehabilitate with implant supported prostheses. Two implant supported over denture was decided to be the treatment option in the mandibular arch. Both the zygomatic implants were decided to be placed in extra sinus approach rather than the classical approach as the patient gave the history of sinusitis [3].
Preliminary impressions were made in upper and lower arches with alginate impression material. Border moulding and secondary impressions were made with addition silicone putty light body wash. Master casts were fabricated along with record bases and occlusal rims. Tentative jaw relation and wax try-in was done establishing the vertical dimension.
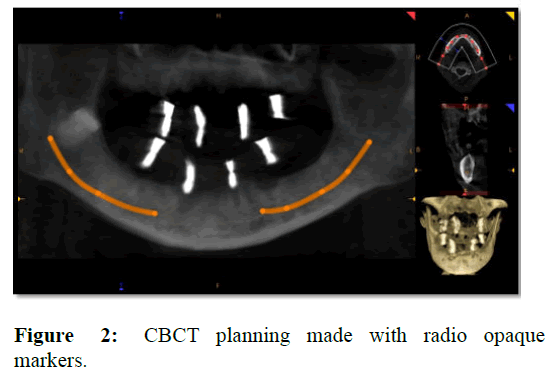
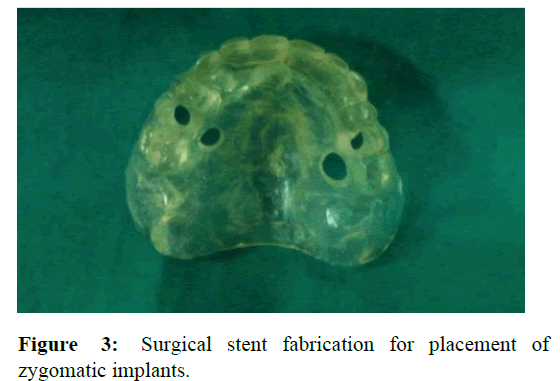
The trial denture was then duplicated and radiopaque markers were incorporated in the duplicated denture. Cone Beam Computed Tomography (CBCT) was advised to the patient to assess the quantity of the existing bone available and the approximity of the vital structures (Figure 2). Routine blood investigations were assessed. Surgical stent was fabricated from the trail denture (Figure 3). CBCT data was analysed and the regions of implant placement both in maxilla and mandible were selected. As per the CBCT data, modifications were made in the surgical stent [4].
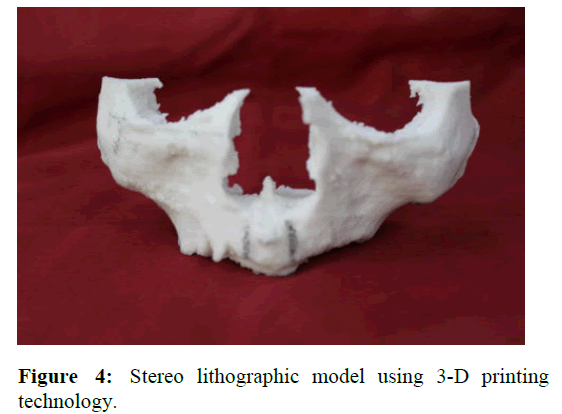
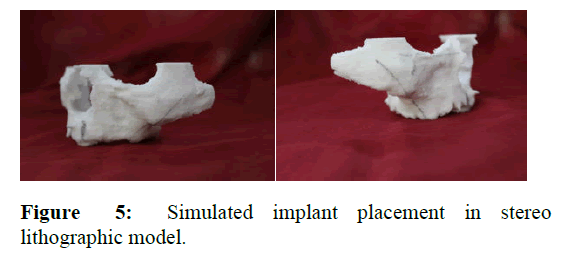
With the help of CBCT data, a stereolithographic model was fabricated using 3-D printing technology (Figure 4). A simulated implant placement was done in the model to analyse the position and angulation of the implants (Figure 5).
Surgical phase
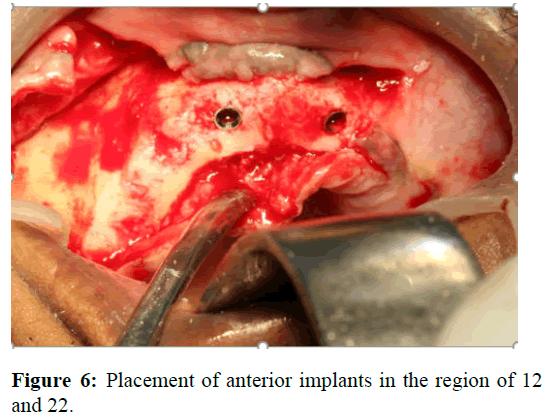
The entire treatment procedure was carried out under general anaesthesia. After administering local anaesthesia, midcrestal incisions were placed all along the maxillary arch from maxillary tuberosity of one side to another. The mucoperiosteol flap was elevated and the excess bony spicules were reduced with help of osteotomy burs. Surgical stent was placed in the upper arch and the desired osteotomy sites were marked. Implant osteotomy procedure was carried out with the help of surgical stent in the region of 12 and 22. Nobel active implants of size 4.3 mm × 11.5 mm were placed in the selected region of 12 and 22 (Figure 6).
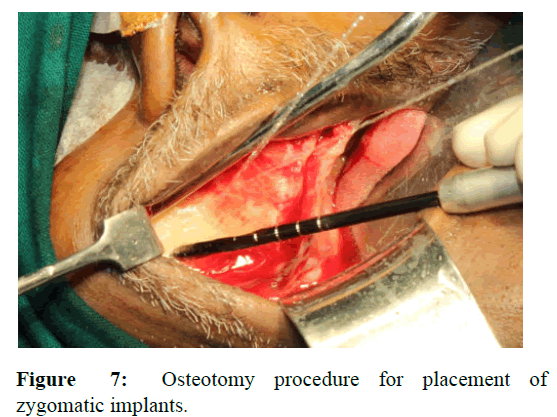
Nobel zygoma 450 implants of size 45 mm in length were selected. With the help of surgical stent the regions of implant placement was marked bilaterally. The entire mucoperiosteal flap was elevated till the zygomatic bone. The initial osteotomy was done with round bur in the zygoma on both the sides. After the site was marked with round bur, pilot drill 3.5 mm short (length 75 mm) and twist drill 2.9 short and 3.5 short were used for osteotomy procedure (Figure 7). Since the implant placement was an extra sinus approach, groove running down from zygoma to the maxillary alveolar ridge was created. Once the osteotomy was completed, zygoma implants of size 45 mm in length was placed bilaterally. The implant head was oriented on the premolar region of the alveolar ridge bilaterally [5].
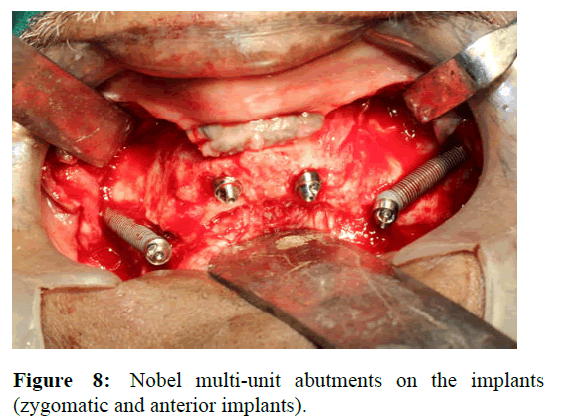
Nobel 170 multi-unit abutments were placed on the implants and torqued with the help of driver (Figure 8). To these multi-unit abutments, multi-unit healing cap was connected. Simple sutures were placed, with horizontal mattress sutures to ensure correct flap closure, using reabsorbable 4/0 polyglactin 910 suture.
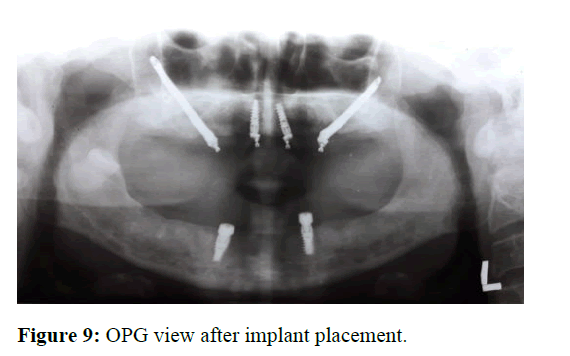
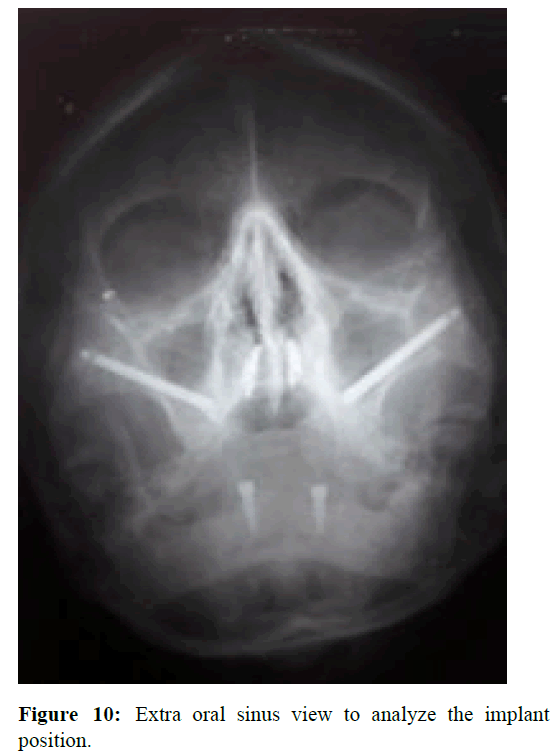
Two nobel active implants of size 4.3 mm × 11.5 mm were placed in the region of 33 and 43. Healing abutments of 5 mm height were connected to the implants. Orthopantomogram (OPG) and sinus view extraoral x-ray was taken to analyse the implants position (Figures 9 and 10). Antibiotic amoxicillin plus clavulanic acid combination drug 625 mg, (1 tablet every 8 hours for 5 days), antiinflammatory diclofenac 100 mg, (1 tablet every 8 hours for 3 days) were prescribed, together with rinses 0.12% chlorhexidine gluconate, twice daily for 15 days.
Prosthetic phase
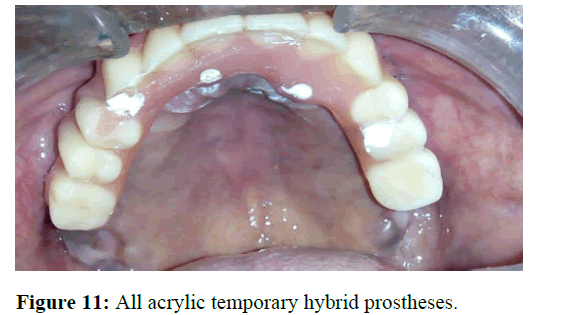
The prosthetic phase was divided into two parts-immediate temporary prostheses and definitive prostheses. The temporary prostheses was fabricated chair side on the day of surgery. The existing upper and lower denture of the patient was modified as temporary all acrylic prostheses. The labial and buccal flange of the existing upper denture was trimmed 1 mm-2 mm short of the vestibular depth. Light body consistency of addition silicone impression material was injected onto the denture and an index in the denture was made for identification of multiunit abutment position. Holes were made on the denture corresponding to the position of the multiunit abutments in the index. Later temporary abutments were connected to the multi-unit abutments and the pickup of the temporary abutments was done with auto polymerising acrylic resin. Screw retained temporary hybrid prostheses was fabricated for the upper arch. The hybrid prostheses was inserted and the abutment screws were torqued to 15 Ncm torque. The screw access holes were closed with non-eugenol temporary luting cement (Figure 11).
For the lower arch, the locator abutments were connected to the respective implants and the corresponding attachments (locator metal housing) were picked up in the lower denture with auto polymerising resin with cap inside the metal housing [6]. Patient was asked to report for regular periodic visits to review the temporary prostheses.
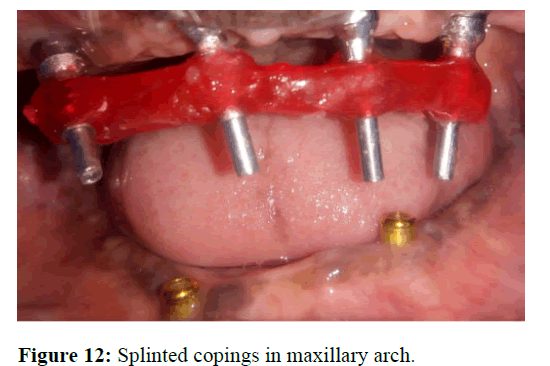
The definitive prostheses was done six months after the surgical procedure. The existing temporary prostheses was inspected and it was removed. The oral health status and the condition of the abutments were checked. Multi-unit healing caps were connected to the abutments and an alginate impression was made for the fabrication of special tray. Open tray impression copings were attached to the multiunit abutments. The copings were splinted with the help of pattern resin by brush bead technique (Figure 12).
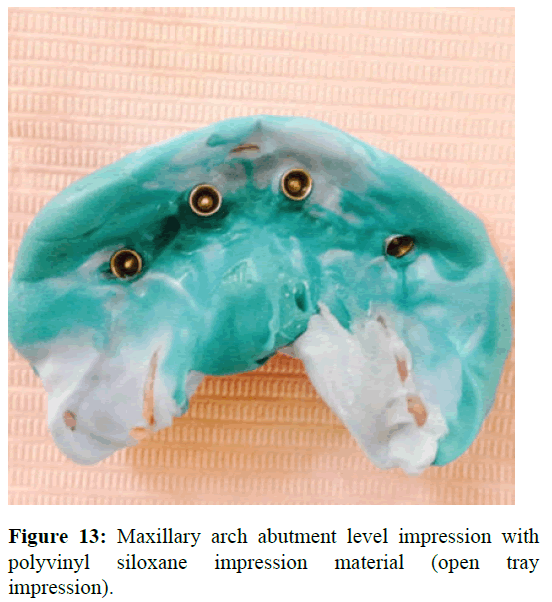
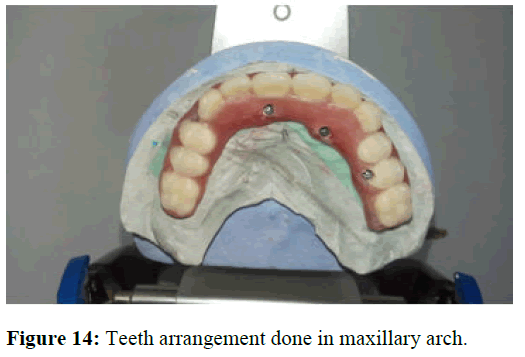
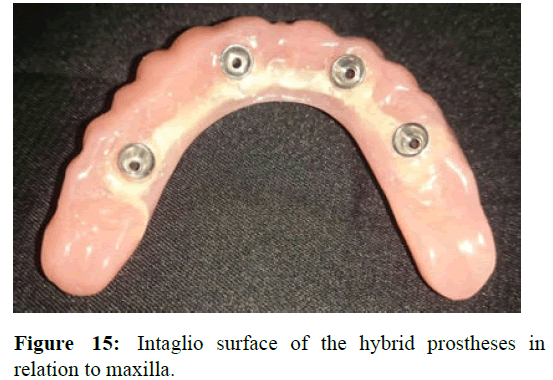
The fit of the special tray was checked intraorally and later the impression copings were picked up by PVS putty wash impression. In the lower arch, special tray was constructed. Border molding and secondary impression was made with polyvinyl siloxane impression material (Figure 13). Master cast was fabricated with type IV dental stone for both upper and lower arches. On the upper master cast abutments were connected to the cast and a jig trial of pattern resin was made. It was checked intraorally to verify the accuracy and position of the abutments picked up in the impression. After the jig verification, cobalt chromium framework was fabricated. Face bow transfer and jaw relation was done following which teeth arrangement was carried on (Figure 14). Bilateral balanced occlusion was decided as the scheme of occlusion for this case. Wax try in was inserted, factors such as esthetics and phonetics were evaluated. After the trial verification, denture processing was carried out. Hybrid prostheses with metal framework for upper arch and in lower arch locator attachment overdenture was fabricated (Figure 15).
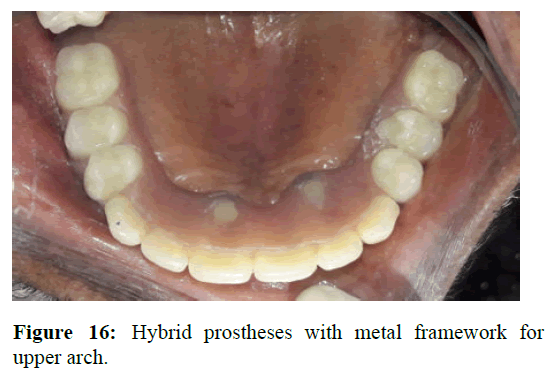
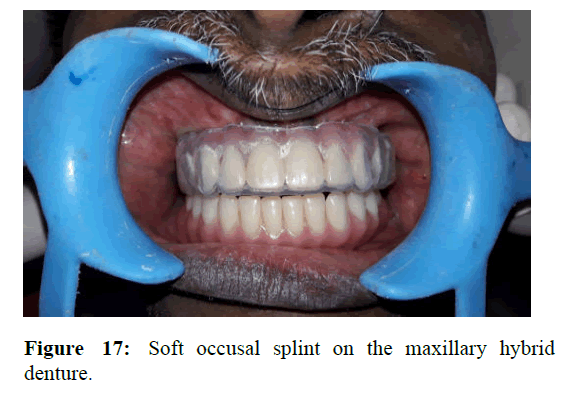
The screw retained hybrid prostheses was inserted and the abutment screws were torqued to 15 Ncm. The screw access holes were later closed by light cure composite resin (Figure 16). Lower arch over denture was fabricated similar to the steps followed in temporary prostheses. Occlusion was checked and occlusal prematurities were removed. Soft occusal splint was fabricated for the maxillary arch covering the hybrid denture. The splint was given to decrease the occusal stress and harmonise the occusal force distribution. The patient was asked to wear the splint for fifteen days to a month duration (Figure 17). Periodic review was followed up after the treatment [7].
Discussion
Restoring the edentulous maxilla poses a greater challenge. Factors such as masticatory function and phonetics plays an important role in fabrication of the prostheses. So a systematic pre-treatment approach is needed for edentulous patients for a better treatment outcome. Three factors are considered as key determinants for successful treatment of completely edentulous maxilla. These factors are:
• Presence or absence of composite defect.
• Visibility or lack thereof of the residual ridge crest
without denture in place, with normal smile.
• The amount of bone available in 3 separate zones of the
maxilla as seen in panoramic radiograph.
The maxillary anterior region is designated as zone 1, the premolar region is zone 2 and the molar region as zone 3. This analysis aids the surgical and restorative team to plan and execute the treatment. Other prosthetic factors to be considered are extra-oral features, aesthetic lip line, interarch space, bone quality, bone quantity, existing occlusal plane, maxillo-mandible relationship, arch-form and existing prosthesis [8].
The extensive surgical procedures for bone graft harvesting and time taken for the final treatment lead to many disadvantages such as multiple surgeries, morbidity of donor site possibility of graft failure, waiting periods (3 to 6 months to heal), additional number of implants considering failure of any, lack of provisional restorations, only delayed loading, decreased patient comfort. To overcome these disadvantages newer advanced techniques without grafting for treatment of edentulous patients were developed. One such technique was the placement of zygomatic implant developed by Branemark in 1998, which was later modified by Stella and Warner.
There are many surgical techniques for the placement of zygomatic implants, the initial classic technique was first described by Branemark. The survival rates of the zygomatic implants is around 98%-100%. The thick cortical layer of the zygoma bone provides dense and prolonged anchorage. This type of solid and tricortical anchorage supports the masticatory forces applied at the occlusal level thereby increasing both the success and survival rate. The main advantages of the zygomatic implants are elimination of the donor site morbidity and infection in the graft material and decreased treatment time. Zygomatic implants despite of their advantages, have some complications and problems. Complications such as soft tissue inflammation around the abutments, sinusitis, oroantral fistula with or without sinusitis are more commonly seen after the placement of implant.
Soft tissue inflammation can cause gingival problems around the implant. No such complaints were seen in our case, since proper oral hygiene and periodic follow up was done (three months once). No reports of sinusitis and oral antral fistula was reported in our case. The success rate of the zygomatic implants is around 97%. Fixed ceramo-metal restoration, implant-tissue supported prostheses (Hybrid prostheses and bar retained prostheses) are considered better prosthetic options in restoring the zygomatic implants. The prostheses should be firm in nature resisting the forces causing deformation and deviation as these forces can lead to implant loss and other screw loosening problems. Hybrid denture prostheses (FP3 type) was considered in our case to restore the maxilla. Implant supported hybrid prostheses were decided to be fabricated since the intra-arch distance was around 33 mm for patient. It has been observed that hybrid dentures offer good masticatory efficiency and better psychological satisfaction to the patients than the conventional over dentures. These prostheses can also be used in cases of combination of tilted and axial implants. Cantilever length is also an important parameter that is to be evaluated when deciding to fabricate implant supported hybrid prosthesis. In the current case, cantilever length was 13 mm, respectively which is in line with the suggested values [9].
The other important factor during the manufacturing of implant-supported hybrid prosthesis is obtaining a passive fit of the framework. In the current case, verification index was fabricated, the material of choice of the index was pattern resin. This index was checked intraorally to confirm the accuracy of the implant positions seen in master cast. Other important factor to be consider when fabricating implant supported complete prosthesis is the framework material. In the current scenario, base metal alloy was used to fabricate the frameworks of the prostheses. Cobalt-chromium alloy was used as the material of choice, the reason for the choice was its cost effectiveness and its easiness to section and solder the framework [10].
Conclusion
In conclusion treatment of atrophic maxilla using zygomatic implants is a good treatment option because of its high success rate, evading the complicated grafting procedures and the option of immediate function. Thus the use of zygomatic implants have a lot of advantages over its disadvantages improving the overall patient comfort. No implant failure, peri-implantitis, a soft-tissue complication related to prosthesis design, fracture of prosthesis frameworks, screw fractures or screw loosening or difficulty in oral hygiene were noted in the patient during the follow-up period. Further, many studies suggest that a rigid material can diminish the bending moment of the framework and this was other reason for the choice of cobalt-chromium framework as the alloy has shown to generate the least amount of strain on the implants.
References
- Malo P, de Araujo Nobre M, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: A pilot study. J Prosthet Dent. 2008;100:354-366.
[Crossref] [Google Scholar] [PubMed]
- Tzerbos F, Bountaniotis F, Theologie-Lygidakis N, Fakitsas D, Fakitsas I. Complications of zygomatic implants: Our clinical experience with 4 cases. Acta Stomatol Croat Int J Oral Sci. 2016;50:251-257.
[Crossref] [Google Scholar] [PubMed]
- Araujo PP, Sousa SA, Diniz VB, Gomes PP, da Silva JS, et al. Evaluation of patients undergoing placement of zygomatic implants using sinus slot technique. Int J Implant Dent. 2016;2:1.
[Crossref] [Google Scholar] [PubMed]
- Bedrossian E, Sullivan RM, Fortin Y, Malo P, Indresano T. Fixed-prosthetic implant restoration of the edentulous maxilla: A systematic pretreatment evaluation method. J Oral Maxillofac Surg. 2008;66:112-122.
[Crossref] [Google Scholar] [PubMed]
- Prithviraj DR, Vashisht R, Bhalla HK. From maxilla to zygoma: A review on zygomatic implants. J Implant Dent. 2014;4:44.
- Aghabeigi B, Bousdras VA. Rehabilitation of severe maxillary atrophy with zygomatic implants. Clinical report of four cases. Br Dent J. 2007;202:669-675.
[Crossref] [Google Scholar] [PubMed]
- Egilmez F, Ergun G, Cekic-Nagas I, Bozkaya S. Implant-supported hybrid prosthesis: Conventional treatment method for borderline cases. Eur J Dent. 2015;9:442-448.
[Crossref] [Google Scholar] [PubMed]
- Ali SA, Karthigeyan S, Deivanai M, Kumar A. Implant rehabilitation for atrophic maxilla: A review. J Indian Prosthodont Soc. 2014;14:196-207.
[Crossref] [Google scholar] [PubMed]
- Candel-Martí E, Carrillo-Garcia C, Penarrocha-Oltra D, Peñarrocha-Diago M. Rehabilitation of atrophic posterior maxilla with zygomatic implants. J Oral Implantol. 2012;38:653-657.
[Crossref] [Google Scholar] [PubMed]
- Duarte LR, Filho HN, Francischone CE, Peredo LG, Brånemark PI. The establishment of a protocol for the total rehabilitation of atrophic maxillae employing four zygomatic fixtures in an immediate loading system-a 30 month clinical and radiographic follow‐up. Clin Implant Dent Relat Res. 2007;9:186-196.
[Crossref] [Google scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.