Retained Foreign Bodies: A Serious Threat in the Indian Operation Room
- *Corresponding Author:
- Mr. Gaurav Sharma
Department of Biomedical and Pharmaceutical Science, College of Pharmacy, Idaho State University, Pocatello, Idaho, USA.
E-mail: shargaur@pharmacy.isu.edu
Citation: Sharma G, Bigelow JC. Retained foreign bodies: A serious threat in the Indian operation room. Ann Med Health Sci Res 2014;4:30-7.
Abstract
Retained foreign bodies (RFBs) are a surgical complication resulting from foreign materials accidently left in a patient’s body. This review attempts to give an overview of different types of RFBs, problems related to them and their management after the surgical operation. The internet was searched using the Google and Google scholar. In addition, relevant electronic journals from the University’s library such as Entrez (including PubMed and PubMed central), Since Direct, Scirus, NIH.gov, Medknow.com, Medscape.com, Scopus, MedHelp.org, Cochrane library, WebMD.com, and World Health Organization Hinari. It shows that the major reasons of RFBs are emergency surgical operation with unplanned changes, patient high body mass index, and poor communication. To prevent this textile material should be radiopaque marked and must be counted once at the start and twice at the conclusion of all surgical procedures. If the count is incorrect, then radiography or manually re‑exploration should be performed. Ultrasonography, computerized tomography, magnetic resonance imaging and radio frequency identification are also used in the proper identification of RFBs. Safety practice should be robust and simple enough to protect patient under the most chaotic of circumstances. Proper communication among the personnel participating in surgery aimed at preventing this medical negligence would help in mitigating such errors. Finally, the surgeon should not only follow the standard recommended procedure, but also report cases of RFBs.
Keywords
Medical negligence, Radiography, Retained foreign bodies
Introduction
Retained foreign bodies (RFBs) is a term for a surgical complication resulting from foreign materials accidently left in a patient’s body.[1,2] The term “gossypiboma” (Gossypium: Latin, cotton; Boma: Swahili, a place of concealment) refers to a mass composed of cotton matrix retained within the human body.[3] Other reported foreign bodies that may be forgotten in the abdomen include abdominal towels, artery forceps, pieces of broken instruments or irrigating sets and rubber tubes.[4] RFBs are rarely reported in the literature because symptoms are usually non‑specific and some patient remains asymptomatic and are never discovered or documented.[5]
The actual incidence of RFBs is difficult to determine, possibly due to reluctance to report an occurrence arising from fear of legal repercussions [6] and are most frequently discovered in the abdomen.[7] The occurrence varies between 1 in 100 and 1 in 5,000 for all surgical interventions and 1 in 1,000‑1,500 for all laparatomies.[8,9] It has been estimated that more than 1,500 cases of RFBs occur annually in the USA.[8,10] It has been estimated that one case of a retained item post‑surgery occurs at least once a year in any hospital where 8,000‑18,000 major procedures are performed annually.[10] This estimate is based on claims data, but there likely have been uncounted cases settled outside the legal system. Mortality related to RFBs is as high as 11% to 35%,[11] emphasizing the need to prevent this medical complication. The major reasons of RFBs are emergency interventions and unplanned changes during the operations.[8] Moreover, obese patients with a higher body mass index (BMI) and female patients due to difficult gynecological procedures were reported to be the risk groups for this iatrogenic complication.[8,10,12] RFBs is frequently located in the abdominal and pelvic cavities after gynecologic, thoracic, and upper abdominal surgical separations, but can also occur after orthopedic, urological, and neurological procedures.[8,12]
Case reports of RFBs are rarely published because it makes health‑care workers hesitate to report errors for fear of losing their own jobs or fear of some other form of reprisal. The scares information about the reason and management of errors, and numerous single information and so far not considered in recent reviews warrant a summary of the current knowledge about these medical errors. The current review is focused on finding the causes and reasons of RFBs after the surgical operation. Relevant publications until December 2012 are reviewed in this paper. Information on RFBs from previous publications was supplemented and systemized. As criteria of systemization, the different types of RFBs cases in Indian hospitals was taken into consideration as well as a problem related to Retained Foreign Bodies are discussed. In addition, different technology used to reduce medical errors was included in this review. In India, the case is more severe and multiple cases of RFBs have been reported. As such there is an acute need for reviewing the various aspects of these medical errors to decrease the morbidity and mortality arising thereof from these errors. We stressed the importance of this operative iatrogenic complication.
Methods for Literature Search
The internet was searched using the Google and Google scholar. In addition, relevant electronic journals from the University’s library including Entrez (including PubMed and PubMed central), Since Direct, Scirus, NIH.gov, Medknow. com, Medscape.com, Scopus, MedHelp.org, Cochrane library, WebMD.com, and World Health Organization Hinari. The alert system of big publishers (ASM, Blackwell, Elsevier, Oxford and Springer) was used for this review with the search strategy of RFBs in the operation theater, described anywhere in the text and without limitation of time span and language (01 January 2013). Reference lists of related articles were studied to detect articles not traced by this search strategy.
Types of RFBs
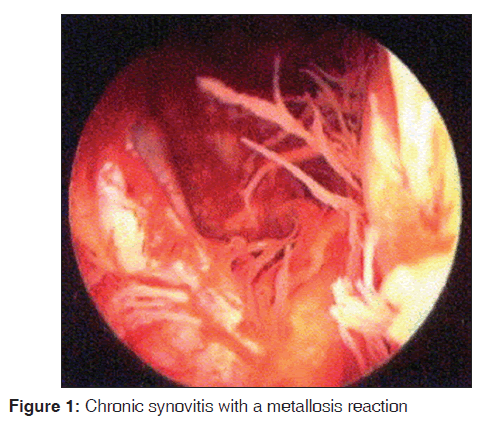
The first case of RFBs in the medical literature was reported by Wilson in 1884.[13‑15] Since, then, many case reports about gossypiboma have been published.[15] Some common instruments, which are left behind during the surgery are needles, knife blades, safety pins, scalpels, clamps, scissors, sponges, abdominal towels, and electrosurgical adapters, tweezers, forceps, suction tips and tubes, scopes, ultrasound tissue disruptors, asepto bulbs, cryotomes and cutting laser guides, and measuring devices.[16] Among the reported cases of foreign bodies retained post‑operatively, laparotomy sponge is the most common [17] and is reported mostly after open cholecystectomy.[18] It may cause mild discomfort and pain and malabsorption symptoms of the severe pain of peritonitis or obstruction and can appear after a long time.[17‑20] Moreover, a sponge can migrate into the intestinal lumen, urinary bladder to thorax.[18‑20] Transmural migration of a foreign body can occur in various intra‑abdominal locations and is directly related to a seromuscular incision of the intestine if made.[16] Hussaini et al.reported an unusual case of gossypiboma in the scrotum of the patient.[21] In another case, a scalpel was found after 10 years in the knee joint of a patient, which causes a chronic synovitis [Figure 1].[18,22] In a different case, a scalpel blade was detached from its handle and lodged into the patient’s knee. It was realized after the incision was closed. They reopened the portals that had previously been sutured closed. While removing the blade its thin edge hit soft‑tissue, bent, and broke into two pieces. It took a long time to remove the second part of the blade. Finally, the patient suffered from persistent problem with pain in the knee, which limits her walking and weight bearing activities.[23] A 7 inch forceps were founded after magnetic resonance imaging (MRI) scans in the stomach of the patient who suffered from the severe pain [24] and also causes severe injury in the abdomen of the patient.
According to the Turkish Penal Code (Article 280), if a health care giver behaves contrary to his responsibility, he/she may face penal sanctions. Gossypiboma is a situation in which experts failed to achieve the standard of care required. Standard care is a care needed for a medical doctor who has same situations and same conditions in consideration of scientific and technique developing level of medical science, labor conditions, and education level of medical doctors.[25] In most cases, the surgeon is held responsible for the errors of other members of the surgical team.[26] This is the responsibility not only of the surgeon, but of the assistant(s) and operating theater nurses as well.
Epidemiology
RFBs cases have rarely been reported. In many cases, when the patient came to know about the gossypiboma and the second surgical operation needed to remove it; may cause legal problem between the patient and the surgeon. Shah and Lander reported 103 reports of RFBs after surgery with the mean age of 11.5 years. Moreover, it causes increases in the medication charge and mean length of stay in the hospital for the patient.[27] Egorova et al. reported that in coronary artery by pass graft surgery the rate of RFBs to be 1 of 7,000 (0.0143%) surgeries.[28] The rate of RFBs after emergency trauma surgery on cavitary locations (abdomen, thorax, and others) was reported to be 0.12%.[29] Ugwu et al. studied seven cases of forgotten foreign bodies in Nigeria.[30] The major reason of medical errors are emergencies, time‑consuming operations, hemorrhagic procedures, sponge counting while closing, operation in anatomic regions hard to reach and alteration in operating theater personnel.[31‑33]
Some of the common risk factors related to RFBs are complex surgical procedures, emergency surgical procedures, increasing BMI, including more than one surgical team, long surgical operations, unexpected change in the course of a surgical operation and use of small size sponges.[34]
Pathophysiology
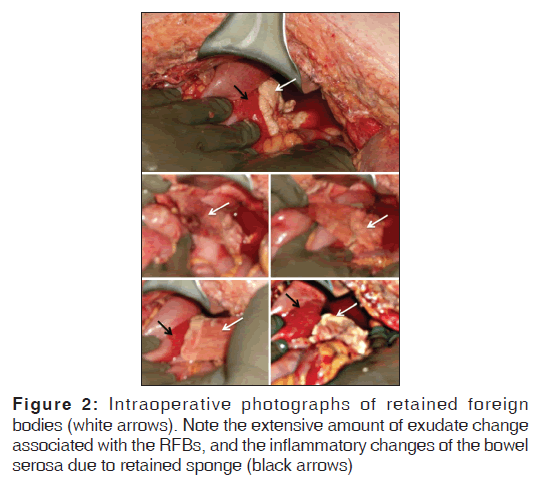
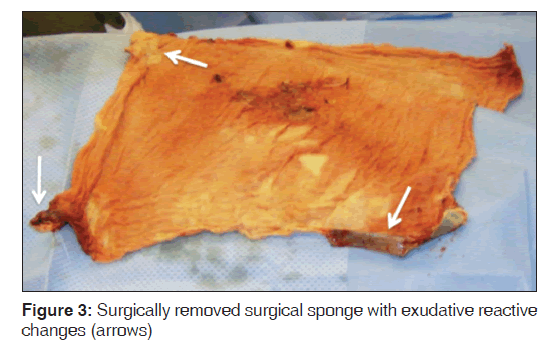
The fate and the symptomatology of RFBs fully depend on the type of foreign body reaction. There are two types of body reactions in RFBs;[35] first is an aseptic fibrous response, resulting in the formation of a granuloma, which can then undergo calcification and decomposition. This response is usually clinically silent and only incidentally discovered. The second is an inflammatory reaction, resulting in an abscess [Figure 2].[73] In the body’s attempt to expel RFBs, fistulization, perforation of viscera, and bowel obstruction have been shown to occur.[35‑37] Gawande et al. reported that RFBs are serious and require re‑operation in 69% of cases of removal.[10] Small‑bowel fistulas, obstruction, or visceral perforation is found in 22% cases. Kester et al. reported a pulmonary embolism caused by pieces of a migrating surgical sponge.[39] Sometimes, RFBs can be misdiagnosed by a new primary tumor, recurrent tumors, and post‑surgical collections. This is due to heterogeneous appearances on different imaging techniques.[38,40‑43] The remnants of a decomposed surgical sponge have even masqueraded as an intrathoracic mass associated with bronchiectasis [44] [Figure 3].
Surgical sponges may cause adverse effect such as sepsis, intestinal obstruction, fistulization, perforation and its complication may lead to death with the death incidences ranging from 15% to 22%.[46,47]
RFBs: Indian cases
There are many examples of RFBs in India and most of them are highlighted by the media and not by the medical journal. Which intern humiliates the surgeon and the hospital authorities, but it does not come up with the solution of the problem.
Abdominal towel
In a case of All India Institute of Medical Sciences (AIIMS) surgeons left a piece of cloth in a patient’s stomach while operating for a gall bladder stone.[48] In a different case surgeons removed an abdominal towel stuck in a 30 year Indian patient’s intestine following a cesarean section. Moreover, it was found that most of the towel parts were rotted away.[49] In a computerized tomography (CT) scan, an abdominal towel was detected as a foreign body, which was left behind in a women’s abdomen during a gall bladder surgery.[50] During a hernia operation, a towel was left behind in the abdomen in an Indian hospital.[51]
Scissors
A pair of scissors was found from the ashes of a woman who had died after undergoing a cesarean operation.[52] Scissors were found in the stomach of 60 years old man and it took 2 years to find it.[53] In a different case a pair of scissors was left in a women’s abdomen at a hospital during a surgery. Four years after the continuing pain, she had to undergo two more surgeries‑one to remove her uterus and second to remove a pair of surgical scissors, which an X‑ray showed was lodged in her belly.[54] In an appendix related operation, surgeon left a pair of scissors and forceps inside the stomach of a person admitted to the hospital.[55] It took three long hours for a surgery to remove scissors from the stomach of the 60 year old patient. Moreover, scissors were stuck with the small intestine of the patient.[56]
Forceps
After 1 year, a woman came to know about that surgeons forgot the forceps in her abdomen during the cesarean operation.[57] In a different case of cesarean surgery, a five‑inch long surgical forceps were removed from the abdomen of women over 4 years.[58] A patient undergoes a second operation to remove the forceps, but she develops an infection in the stomach and later died of heart failure from multiple complications.[59] Surgeons of AIIMS Institute left artery forceps in the stomach of a 30‑year‑old woman who underwent a second operation. The operation included the removal of the left kidney and urethra, and the reconstruction of the urinary bladder. In a routine check‑up forceps was found in an X‑ray examination of the patient.[60]
Scalpel
At 2 hours after a surgery; a patient had to have a second surgery as a Dhaka Medical College Hospital surgeon left a scalpel blade in his body and stitched up the wound.[61] A patient suffered agonizing pain for 6 days as a surgical instrument (30 cm blade) was left inside.[62]
Safety pin
A patient went to a hospital as she accidentally swallowed a safety pin. Later, it was revealed that that along with a safety pin forceps is also lodged in her abdomen. It turned out the forceps were left behind in her abdomen after she underwent a cesarean section at the same hospital. Moreover, surgeons refused to give the medical records to her husband.[63]
Needle
A needle was left inside the body of a woman during stitching after delivery is an example of blatant medical negligence.[64]
Clinical diagnosis and technical investigation
Some common symptoms related to RFBs are abdominal palpable mass, nausea, pain, fever, weight loss, and vomiting, diarrhea, and rectal bleeding. Coughing, dyspnea, and dysuria may be due to the exogenous compression on the urinary or respiratory tract.
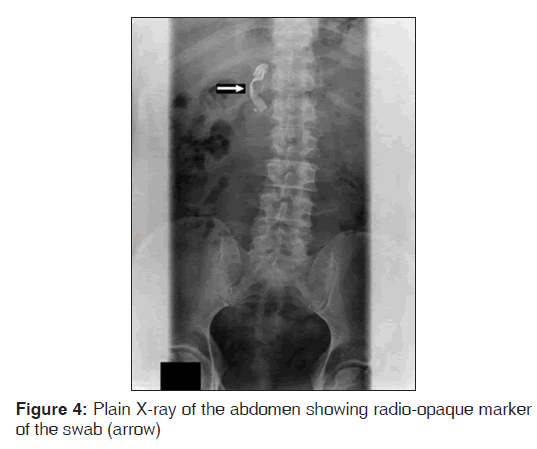
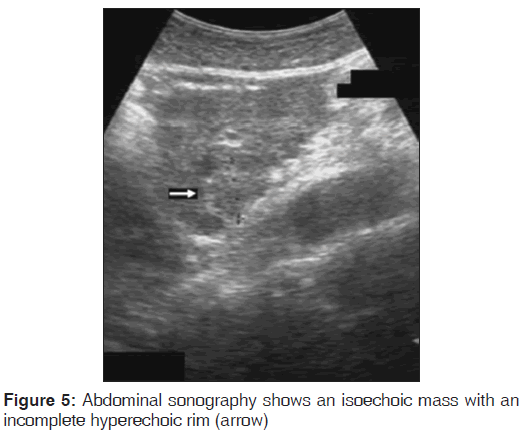
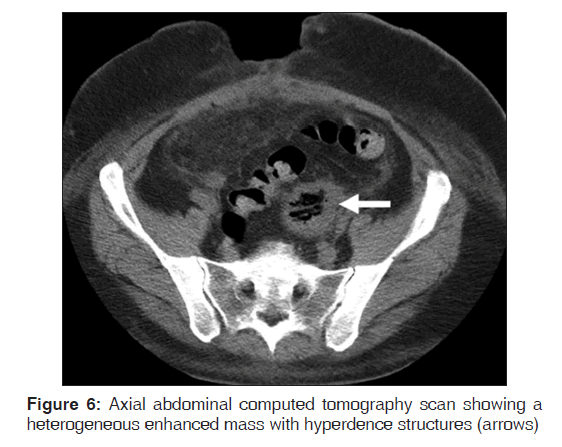
There are various techniques that can be used for the identification of RFBs in the body like Radiopaque marking. In this technique, sponges can be soaked through with radio‑opaque marker before the operation, so that sponges are easily visible on the plain radiographs.[65] However, the use of radiopaque markers is not generalized and they may get distorted, folded, twisted or may get attached to the bone; they may get degenerated over the time period. X‑ray can be used for the identification of RFBs [Figure 4].[66] Unfortunately, it is very difficult to detect the missing needle and hence, even a high resolution X‑ray does not ensure that the needle is not actually inside the patient. In Ultrasonography, gossypiboma can be diagnosed by the presence of bright echogenic wavy structures with a cystic mass showing posterior acoustic shadowing that changes in parallel with the direction of the ultrasound beam [Figure 5].[67] Ultrasonography diagnoses the nature (solid or liquid) of the mass in three dimensions. However, the technique is not good in the presence of fat or gas in the abdomen. In another technique of CT: A surgical sponge will show bubbles on soft‑tissue masses. The flaw with this technique is that gossypibomas are easily confused with abscesses [Figure 6].[68] Retained sponges of CT typically are seen as soft‑tissue‑density masses with a whorled texture or spongiform patterns because of air trapping within the synthetic fibers of the sponge. Longer‑existing gossypiboma may cause mottled calcification and gas bubbles to appear. Kopka et al. showed that the CT of 8 surgical sponges placed in a water bath for 6 months document the presence and persistence of gas bubbles. Compared to the ultrasonography, CT gives less characteristic and poorly constant image. When no radio‑opaque marker is seen on X‑ray or CT, the characteristic internal structure of the gauze granuloma is best visualized on MRI. It may appear as a low‑signal‑intensity lesion on T2‑weighted image with wavy, striped or spotted appearance.[45]
Compared to CT it provides an image in 3 dimensions. A rim‑enhanced wall or calcified rim may be seen as well [69] in a different technique for radio frequency identification (RFID): Surgical sponges embedded with passive RFID tags presents a high probability of reducing or eliminating instances of gossypiboma or retained surgical sponges.[70] A case of gossypiboma was diagnosed by skeletal scintigraphy.[71] In some cases, gossypiboma has been diagnosed by endoscopy (esophagogastroscopy, endoscopic retrograde cholangiopancreatography‑ERCP, and colonoscopy) when symptoms of obstruction are present or if it enters the bowel lumen.[31]
Macario et al. hypothesized a handheld wand‑scanning device to detect commonly used surgical gauze sponges, which has been tagged with a RFID chip. It was found that the wand device has a 100% successful detection, specificity, and sensitivity.[46] About one‑third correct pre‑operative diagnosis is made in RFB cases.[11] Among these most cited tentative diagnosis are tumor or tumor recurrence, invagination, post‑operative adhesions, and intraoperative abscess.[13]
Management
In the operation room (OR), a team of professionals performs exacting tasks under considerable time pressure, which is highly complex and internally dynamic work. This work environment mandates durable and systemically applied processes of care. These safety practices must be robust enough to protect patients under the most chaotic of circumstances yet be simple enough to be applied and understood by all health‑care professional, from the novice to the master. Each and every person working in the OR has a common ethical, legal, and moral responsibility to do whatever possible to provide proper outcome.[72] Gibbs et al. reported that RFBs are due to poor communication between the personnel involved in the OR. For instance; surgeon dismissing reports of a miscount as erroneous, multiple intraoperative personnel changes without accurate cross‑informational reporting, and mixed messages between team members about the timing for the emergence from anesthesia if intraoperative X‑ray to detect a missing item is needed.[72] Berguer et al. compared 235 cases and found that most of them were emergency surgical procedure, unplanned changes in the procedure performed and body‑mass index.[73] The Association of perioperative Registered Nurses Practice Committee presents detailed guidelines and best practices for avoiding retained surgical devices.[74] According to them accurate counting (baseline and final) should be carried out and if it is incorrect a radiograph shall be obtained to ensure that RFBs has not been unintentionally retained. Moreover, a good communication is necessary before and during the surgical operation, at staff changes, at handoffs and transitioning to the OR.[74]
According to association of OR nurses standards; sponges detectable on radiography should be used and they should be counted once at the start and twice at the conclusion of all surgical procedures.[75] Textile materials used should be impregnated with radiopaque markers.[76] Moreover, the instrument should be counted in all cases involving an open cavity. If a count is incorrect‑then radiography or manual re‑exploration is to be performed. Many cases of RFBs that have been reported to result from a failure to adhere to these standards.[32,77] However, in the majority of cases, foreign bodies go undetected despite proper procedures. Previous descriptive studies have been unable to establish the human and system‑related factors involved.[77] Although surgery is the recommended mode of treatment, prevention is the best course and should be emphasized. A clear record of all foreign materials, which are used during the surgery, should be made.
In spite of the latest advancement in surgical procedures and technical evolution intended to protect the patient in the operating theater, the problem of RFBs after surgery is still unresolved. The solution of the problem can only be carried out by the surgeons and staff available in the operation theater. Not only surgeons should report cases of RFBs in the medical literature in the future, but also follow the standard recommended procedures in the operation theatre.[78]
In asymptomatic RFBs cases, the patient should be informed and motivated for a reoperation: A wait‑and‑see policy might be life‑threatening. According to our view the surgeon should not remain silent but should inform the patient about the RFBs an effort should be made to contact the surgeon who performed the former intervention.
Conclusion
RFBs are mainly caused because of multiple major surgical procedures being done at a same time. RFB is potentially life‑threatening. It may cause serious medical and legal problems between the patient and the doctor. Therefore, extreme care should be taken in the handling of instruments during the surgical procedures is highly advisable. Training of the surgeon is very important to maximize patient safety. Proper communication among the personnel participating in surgery aimed at preventing this medical negligence would help in mitigating such errors. Finally, stronger laws against the responsible surgeon may help in providing justice to the patient.
Source of Support:
Nil.
Conflict of Interest:
None declared.
References
- Yaycioglu O, Ulusan S, Ezer A, Guvel S. Ureteroappendiceal fistula due to gossypiboma. Urol Int 2007;79:187-8.
- Sun HS, Chen SL, Kuo CC, Wang SC, Kao YL. Gossypiboma ? Retained surgical sponge. J Chin Med Assoc 2007;70:511-3.
- Wan YL, Ko SF, Ng KK, Cheung YC, Lui KW, Wong HF. Role of CT-guided core needle biopsy in the diagnosis of a gossypiboma: Case report. Abdom Imaging 2004;29:713-5.
- Sharma D, Pratap A, Tandon A, Shukla RC, Shukla VK. Unconsidered cause of bowel obstruction ? Gossypiboma. Can J Surg 2008;51:E34-5.
- Garg M, Aggarwal AD. A review of medico legal consequences of gossypiboma. J Indian Acad Forensic Med 2010;32:358-61.
- Kiernan F, Joyce M, Byrnes CK, O?Grady H, Keane FB, Neary P. Gossypiboma: A case report and review of the literature. Ir J Med Sci 2008;177:389-91.
- Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: Pictorial review. AJR Am J Roentgenol 2009;193:S94-101.
- Bani-Hani KE, Gharaibeh KA, Yaghan RJ. Retained surgical sponges (gossypiboma). Asian J Surg 2005;28:109-15.
- Asuquo ME, Ogbu N, Udosen J, Ekpo R, Agbor C, Ozinko M et al. Acute abdomen from gossypiboma: A case series andreview of literature. Niger J Surg Res 2006;8:174-6.
- Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med 2003;348:229-35.
- Chorvat G, Kahn J, Camelot G, Henriet P, Gillet JY, Gillet M. Pleural textilome discovered after the cure of persistent arterial canal. Tunis Med 1976;30:643.
- Iwase T, Ozawa T, Koyama A, Satake K, Tauchi R, Ohno Y. Gossypiboma (foreign body granuloma) mimicking a soft tissue tumor with hip hemiarthroplasty. J Orthop Sci 2007;12:497-501.
- Garg M, Aggarwal AD. A review of medicolegal consequences of gossypiboma. J Indian Acad Forensic Med 2010;32:358-61.
- Yildirim S, Tarim A, Nursal TZ, Yildirim T, Caliskan K, Torer N, et al. Retained surgical sponge (gossypiboma) after intraabdominal or retroperitoneal surgery: 14 cases treated at a single center. Langenbecks Arch Surg 2006;391:390-5.
- Lauwers PR, Van Hee RH. Intraperitoneal gossypibomas: The need to count sponges. World J Surg 2000;24:521-7.
- Sakhel K, Hines J. To forget is human: The case of the retained bulb. J Robot Surg 2009;3:45-7.
- Dhillon JS, Park A. Transmural migration of a retained laparotomy sponge. Am Surg 2002;68:603-5.
- Kim CK, Park BK, Ha H. Gossypiboma in abdomen and pelvis: MRI findings in four patients. AJR Am J Roentgenol 2007;189:814-7.
- Lone GN, Bhat AH, Tak MY, Garcoo SA. Transdiaphragmatic migration of forgotten gauze sponge: An unreported entity of lung abscess. Eur J Cardiothorac Surg 2005;28:355-7.
- Sinha SK, Gupta S, Behra A, Khaitan A, Kochhar R, Sharma BC, et al. Retained surgical sponge: An unusual cause of malabsorption. Trop Gastroenterol 1999;20:42-4.
- Hussaini MY, Muhammed A, Ahmad B, Hafeez AO, Hycinth MN. Gossypiboma in the scrotum with unusual cutaneous manifestations. Arch Int Surg 2012;2:33-6.
- Rajadhyaksha AD, Mont MA, Becker L. An unusual cause of knee pain 10 years after arthroscopy. Arthroscopy 2006;22:1253.e1-3.
- Gruson KI, Ilalov K, Youm T. A broken scalpel blade tip: An unusual complication of knee arthroscopy. Bull NYU Hosp Jt Dis 2008;66:54-6.
- Docs left 7in forceps in me, 2010. Available from: http:// www.thesun.co.uk/sol/homepage/news/2846757/ Doctors-left-seven-inch-forceps-inside-mum-after-routine-operation.html. [Cited on 2012 Jun 8].
- Tarik U, Gokhan DM, Sunay YM, Mahmut A. The medico-legal importance of gossypiboma. In: Proceedings of the 4th Mediterranean Academy of Forensic Science Meeting; 2008 Oct 14-18. Antalya-Turkey: Abstract CD of Poster Presentation; 2009. p. 82-3.
- Tumer AR, Yasti AC. Medical and legal evaluations of the retained foreign bodies in Turkey. Leg Med (Tokyo) 2005;7:311-3.
- Shah RK, Lander L. Retained foreign bodies during surgery in pediatric patients: A national perspective. J Pediatr Surg 2009;44:738-42.
- Egorova NN, Moskowitz A, Gelijns A, Weinberg A, Curty J, Rabin-Fastman B, et al. Managing the prevention of retained surgical instruments: What is the value of counting? Ann Surg 2008;247:13-8.
- Teixeira PG, Inaba K, Salim A, Brown C, Rhee P, Browder T, et al. Retained foreign bodies after emergent traumasurgery: Incidence after 2526 cavitary explorations. Am Surg 2007;73:1031-4.
- Ugwu BT, Isamade ES, Misauno MA, Mohammed AM, Uwumarogie OL, Liman HU, et al. Forgotten foreign bodies in the abdomen. Niger J Surg Res 2004;6:137-40.
- Tan VE, Sethi DS. Gossypiboma: An unusual intracranial complication of endoscopic sinus surgery. Laryngoscope 2011;121:879-81.
- Rappaport W, Haynes K. The retained surgical sponge following intra-abdominal surgery. A continuing problem. Arch Surg 1990;125:405-7.
- Guiard JM, Bonnet JC, Boutin JP, Plane D, Guilleux MH, Delorme G. ?Textiloma?: X-ray computed tomographic aspect. Apropos of a case. Ann Radiol (Paris) 1988;31:49-52.
- Stawicki SP, Evans DC, Cipolla J, Seamon MJ, Lukaszczyk JJ, Prosciak MP, et al. Retained surgical foreign bodies: A comprehensive review of risks and preventive strategies. Scand J Surg 2009;98:8-17.
- D�x M, Ganten M, Lubienski A, Grenacher L. Retained surgical sponge with migration into the duodenum and persistent duodenal fistula. Eur Radiol 2002;12:S74-7.
- Robinson KB, Levin EJ. Erosion of retained surgical sponges into the intestine. Am J Roentgenol Radium Ther Nucl Med 1966;96:339-43.
- Prasad S, Krishnan A, Limdi J, Patankar T. Imaging features of gossypiboma: Report of two cases. J Postgrad Med 1999;45:18-9.
- Gonzalez-OjedaA, Rodriguez-AlcantarDA, Arenas-MarquezH, Sanchez Perez-Verdia E, Chavez-Perez R, Alvarez-Quintero R, et al. Retained foreign bodies following intra-abdominalsurgery. Hepatogastroenterology 1999;46:808-12.
- Kester NL, Hassien JD. Pulmonary embolism caused by a surgical sponge. AJR Am J Roentgenol 1992;158:757-9.
- Hoeffner EG, Soulen RL, Christensen CW. Gelatin sponge mimicking a pelvic neoplasm on MR imaging. AJR Am J Roentgenol 1991;157:1227-8.
- Okten AI, Adam M, Gezercan Y. Textiloma: A case of foreign body mimicking a spinal mass. Eur Spine J 2006;15:626-9.
- Dane C, Yayla M, Dane B. A foreign body (gossypiboma) in pregnancy: First report of a case. Gynecol Surg 2006;3:130-1.
- Sandrasegaran K, Lall C, Rajesh A, Maglinte DT. Distinguishing gelatin bioabsorbable sponge and postoperative abdominal abscess on CT. AJR Am J Roentgenol 2005;184:475-80.
- Suwatanapongched T, Boonkasem S, Sathianpitayakul E, Leelachaikul P. Intrathoracic gossypiboma: Radiographic and CT findings. Br J Radiol 2005;78:851-3.
- Kopka L, Fischer U, Gross AJ, Funke M, Oestmann JW, Grabbe E. CT of retained surgical sponges (textilomas): Pitfalls in detection and evaluation. J Comput Assist Tomogr. 1996 20;6:919-23.
- Macario A, Morris D, Morris S. Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch Surg 2006;141:659-62.
- Vento JA, Karak PK, Henken EM. Gossypiboma as an incidentaloma. Clin Nucl Med 2006;31:176-7.
- Towel left in the stomach at AIIMS, 2007. Available from: http://www.thehindu.com/todays-paper/tp-national/ tp-newdelhi/towel-left-in-the-stomach-at-aiims/ article1889248.ece. [Cited on 2012 Aug 10].
- Bizarre medical error: Towel stuck inside woman?s bowel, removed, 2011. Available from: http:// www . themedguru . com/20110108/newsfeature/ bizarre-medical-error-towel-stuck-inside-womans-bowel-removed-86143276.html. [Cited on 2012 Jan 8].
- Surgeon suspended for leaving towel in woman?s stomach, 2010. Available from: http://www.articles.timesofindia. indiatimes.com/2010-06-25/kanpur/28294444_1_ stomach-towel-ct-scan. [Cited on 2012 Jun 25].
- Malpractice: Compensation demanded from ?negligent doctor?, 2011. Available from: http://www.tribune. com.pk/story/100079/malpractice-compensation-demanded-from-negligent- doctor/. [Cited on 2012 Jan 7].
- Women dies with scissors in stomach, 2006. Available from: http://www.articles.timesofindia.indiatimes. com/2006-03-08/india/27811223_1_scissors-ashes-doctor. [Cited on 2012 Mar 8].
- Scissors removed from man?s tummy after two years, 2010. Available from: http://www.ibnlive.in.com/news/ scissors-removed-from-mans-tummy-after-2-yrs/108108-13. html. [Cited on 2012 Oct 31].
- Six years on, victim compensated for scissors in stomach, 2009. Available from: http://www.twocircles.net/2009aug26/ six_years_victim_compensated_scissors_stomach. html. [Cited on 2012 Aug 26].
- Doctors find scissors, forceps in patient?s stomach, 2007. Available from: http://www.dnaindia.com/india/ report_doctors-find-scissors-forceps-in-patient-s-stomach_ 1095565. [Cited on 2012 Jun 8].
- Scissors taken out from man?s stomach after two years, 2007. Available from: http://www.newkerala.com/news/ fullnews-23057.html. [Cited on 2012 Jun 8].
- Forceps left in woman after caesarean operation, 2006. Available from: http://www.dailytimes.com.pk/default. asp?page=2006\02\24\story_24-2-2006_pg7_8. [Cited on 2012 Jun 8].
- Mother left with seven-inch forceps inside her body for three months in shocking toll of 750 NHS blunders, 2013. Available from: http://www.dailymail.co.uk/news/article-2321975/ Mother-left-SEVEN-INCH-forceps-inside-body-months-shocking-toll-750-NHS-blunders.html. [Cited on 2012 Jun 3].
- Pakistani women die after forceps removed, 2006. Available from: http://www.bhatkallys.com/news/news. asp?aid=1319. [Cited on 2012 Jun 8].
- Express News Service. Forceps left in stomach after surgery, AIIMS orders probe, 2011. Express India. Available from: http://expressindia.indianexpress.com/story_print. php?storyId=264885. Express India. [Cited on 2008 Jan 24].
- A date with Dr. Nightmare, 2009. Available from: http:// www.archive.thedailystar.net/newDesign/news-details. php?nid=110801. [Cited on 2012 Oct 22].
- Agony after operation knife ?left in? during hysterectomy surgery, 2011. Available from: http://www.news. com.au/national-news/agony-after-op-knife-left-in/ story-e6frfkvr-1226094378806. [Cited on 2012 Jul 14].
- Safety pin? No, it?s forceps left by doctors during C-section, 2010. Available from: http://www.indianexpress.com/news/ safety-pin--no-it-s-forceps-left-by-doctors-during-csection/ 578325/. [Cited on 2012 Feb 11].
- Needle left inside woman after delivery, 2011. Available from: http://www.articles.timesofindia. indiatimes.com/2011-07-30/bhubaneswar/29835976_1_ needle-nurse-treatment. [Cited on 2012 Jul 30].
- Takigami I, Itoh Y, Itokazu M, Shimizu K. Radio-opaque marker of a surgical sponge appearing as an intra-articular foreign body after total hip arthroplasty. Arch Orthop Trauma Surg 2008;128:1167-8.
- Cheng TC, Chou AS, Jeng CM, Chang PY, Lee CC. Computed tomography findings of gossypiboma. J Chin Med Assoc2007;70:565-9.
- Sugano S, Suzuki T, Iinuma M, Mizugami H, Kagesawa M, Ozawa K, et al. Gossypiboma: Diagnosis with ultrasonography. J Clin Ultrasound 1993;21:289-92.
- Wan YL, Huang TJ, Huang DL, Lee TY, Tsai CC. Sonography and computed tomography of a gossypiboma and in vitro studies of sponges by ultrasound. Case report. Clin Imaging 1992;16:256-8.
- Kalovidouris A, Kehagias D, Moulopoulos L, Gouliamos A, Pentea S, Vlahos L. Abdominal retained surgical sponges: CT appearance. Eur Radiol 1999;9:1407-10.
- Rogers A, Jones E, Oleynikov D. Radio frequency identification (RFID) applied to surgical sponges. Surg Endosc2007;21:1235-7.
- Yeo EE, Low J. Intra-abdominal retained surgical sponges presenting as a photopenic mass on scintigraphy. Clin Nucl Med 1991;16:543-4.
- Gibbs VC, McGrath MH, Russell TR. The prevention of retained foreign bodies after surgery. Bull Am Coll Surg 2005;90:12-4, 56.
- Berguer R, Heller PJ. Preventing sharps injuries in the operating room. J Am Coll Surg 2004;199:462-7.
- Prevention of unintentionally retained foreign objects in surgery, 2007. Available from: http://www.icsi.org/ home/retained_foreign_objects_in_surgery_prevention_of_ unintentionally_protocol_21475.html. [Cited on 2012 Jun 8].
- Pierson MA. Patient and environmental safety. In: Meeker M, Rothrock J, editors. Alexander?s Care of the Patient in Surgery. 10th ed. St. Louis: Mosby?Year Book; 1995. p. 19-34.
- Gencosmanoglu R, Inceoglu R. An unusual cause of small bowel obstruction: Gossypiboma ? Case report. BMC Surg 2003;3:6.
- O?Connor AR, Coakley FV, Meng MV, Eberhardt SC. Imaging of retained surgical sponges in the abdomen and pelvis. AJR Am J Roentgenol 2003;180:481-9.
- Grassi N, Cipolla C, Torcivia A, Bottino A, Fiorentino E, Ficano L, et al. Trans-visceral migration of retained surgical gauze as a cause of intestinal obstruction: A case report. J Med Case Rep 2008;2:17.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.