Retrospective analysis of Standard Analgesia versus Erector Spinae Plane Catheters in the Major Open Hepatobiliary Surgery : A pilot study
2 Department of Anaesthesiology, National Maternity Hospital ,Dublin 4, Ireland
3 Department of Biostatistician, Medical student, Kings College Hospital, London, UK
4 Department of Physiotherapy, St. Vincents University Hospital, Dublin 2, Ireland
Received: 05-Jul-2022, Manuscript No. AMHSR-22-75417; Editor assigned: 07-Jul-2022, Pre QC No. AMHSR-22-75417; Accepted Date: Jul 07, 2022 ; Reviewed: 22-Jul-2022 QC No. AMHSR-22-75417; Revised: 28-Jul-2022, Manuscript No. AMHSR-22-75417; Published: 03-Aug-2022
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Large upper abdominal incisions are required in major Hepatobiliary (HPB) surgery, and are associated with significant postoperative pain and respiratory complications. Erector Spinae Plane (ESP) blocks and catheters have shown promise as an alternate analgesic technique in thoracic and abdominal surgery. We conducted a retrospective analysis to determine the effect of ESP catheters versus standard analgesia on opiate requirements for the first 7 days post major HPB surgery. A total of 22 patients were included, 10 in the ESP group and 12 in the standard analgesia group. There was a reduction in total oral morphine equivalents from Day 0-7 in the ESP group, with a reduction from a mean of 54 in the standard analgesia group to a mean of 14.38 in the ESP group (p=0.05). There was no difference in the pain scores on Days 0-5 postoperatively between the two groups, either at rest or on movement, but there were reduced pain scores in the ESP group on postoperative Day 6-7, particularly on movement (p=0.02). There was also a decreased length of hospital stay in the ESP group from a median of 12 days in the standard analgesia group to a median of 8 days in the ESP group (p=0.06). Compared to standard analgesia, ESP catheters were associated with lower opiate consumption and decreased hospital length of stay, despite similar or improved pain scores in major HPB surgery. We plan to conduct a randomized controlled trial to investigate this further.
Keywords
Erector spinae block; Regional Anaesthesia; HepatoPancreatoBiliary; Coagulation
Introduction
Large upper abdominal incisions are required for surgical access in major open Hepatobiliary (HPB) surgery. Adequate analgesia is essential in these patients to minimize the risks of postoperative respiratory complications and the development of chronic pain [1–6]. Postoperative ileus is very common in these patients and is exacerbated by opioid administration, with the return of GI function related to opioid dosage and duration [7,8].
Although epidural analgesia is often considered to be ‘gold standard’ practice for major abdominal surgery [9], there are several limitations to placement specifically in HPB surgery, in particular in major liver resection. In patients post large volume liver resection, removal of epidural catheters can be problematic as postoperative synthetic liver dysfunction causes a coagulopathy that is compounded by major blood loss intraoperatively. Neither the size of the required liver resection nor the degree of blood loss is entirely predictable preoperatively. The postoperative coagulopathy typically peaks at day 2-3 postoperatively and often doesn't return to baseline until day 7 [10–12]. Waiting until day 7 to remove an epidural catheter increases the risk of infection[13,14].
Intrathecal morphine combined with opioid-based Patient-Controlled Analgesia (PCA) has been shown by De Pietri, et al. [15] to be to comparable to thoracic epidural analgesia in the initial 48 hours post major liver resection, albeit with increased intravenous opioid PCA usage in the intrathecal morphine group for the first 12 hours. Wound infusion catheters and abdominal wall blocks have also all shown promise when studied as alternative and less invasive techniques for analgesia after major HPB surgery [16–18].
Enhanced Recovery Programmes (ERP) advocate opioid free analgesia targeting different pain pathways through multi-modal analgesia [19,20]. The use of regional anaesthesia and other non-opioid analgesics can help to optimise analgesia and prevent adverse effects due to opioids such as nausea, vomiting, sedation, ileus, pruritus and respiratory depression. Limiting the use of opioids in the perioperative period can enhance recovery by facilitating early mobilisation and return of bowel function [21,22].
Analgesia for major open HPB surgery in our institution has evolved as such to utilise a multimodal approach, including a pre-induction intrathecal morphine injection (dose 5-10 micrograms/kilogram, ideal body weight), rectus sheath and Transversus Abdominal Plane (TAP) blocks with surgically-sited TAP catheters for 5 days postoperatively and analgesic adjuncts including paracetamol and Non-Steroidal Anti-Inflammatories (NSAIDs) where appropriate. Morphine-based PCA commenced on Day 1 postoperatively is used for breakthrough pain.
Erector Spinae Plane (ESP) blocks were first described by Forero, et al. in 2016 [23]. This regional analgesia technique involves deposition of local anaesthetic under ultrasound guidance into the space below the erector spinae muscles onto the transverse process. A catheter is then passed into the plane. Depending on the vertebral level at which the block is performed, the craniocaudal spread of local anaesthetic within this plane allows analgesia to be achieved over multiple thoracic vertebral levels. The analgesic effect was originally postulated to be as a result of blockade of dorsal and ventral rami of nerve roots, as well as anterior spread of local anaesthetic into the paravertebral space. A more recent cadaveric dye injection study did not show spread of dye anteriorly to the paravertebral space but showed staining of the dorsal ramus by dye as it exited the costotransverse foramen which was in close proximity to the injection point, and extension of the dye to the lateral cutaneous branches of the intercostal nerves lateral to the angle of the ribs [24]. Insertion of ESP catheters permit ongoing delivery of analgesia postoperatively. The block was initially described at the level of the T5 vertebra to facilitate thoracic analgesia, while upper abdominal surgical analgesia has been successful with insertion at the T7 vertebral level [25,26].
We initially trialled ESP catheters in a patient for Whipple’s procedure with an allergy to opioids, and as a rescue technique for uncontrolled pain following liver resection with good results [27]. Given our anecdotal clinical success utilising ESP catheters, we performed a retrospective study comparing ESP blocks and catheters performed at the level of the T7 vertebra with our standard analgesic practice in patients undergoing major HPB surgery. Our hypothesis was that patients would have greater analgesic benefit from the ESP catheters, requiring less overall breakthrough analgesia and with less opioid related side effects.
Methods
The study was approved by the St Vincent’s University Hospital clinical audit committee (Approval No. 2154). Approximately 250 major open HPB surgical procedures are carried out each year in St Vincent's University Hospital, comprising 80-100 pancreatic resections including pancreaticoduodenectomy and distal pancreatectomies, and 150-160 liver resections. Written informed consent was obtained from all patients.
Aim
This retrospective audit study was conducted in St Vincent’s University Hospital, Dublin, Ireland between October 2017 and March 2018, to determine the effect of ESP catheters versus standard analgesia on opiate consumption for 7 days post major HPB surgery. The total number of patients included was 22 (10 in the ESP group and 12 in the standard analgesia group).
Inclusion criteria
This retrospective audit study was conducted in St Vincent’s University Hospital, Dublin, Ireland between October 2017 and March 2018, to determine the effect of ESP catheters versus standard analgesia on opiate consumption for 7 days post major HPB surgery. The total number of patients included was 22 (10 in the ESP group and 12 in the standard analgesia group).
Exclusion criteria
Allergy to local anaesthetic agents
History of chronic pain or preoperative opioid consumption.
Study population
We included adult patients undergoing major open HPB surgery under two consultant surgeons, and occurring on specific weekdays (Wednesdays and Thursdays). All surgical procedures were performed through a unilateral or bilateral subcostal or reverse L incision.
Alternate weeks all patients received ESP blocks and catheters under the direct supervision of a single consultant anaesthetist who was performing this blocks for HPB surgery. The other weeks, patients received the standard analgesic regime with pre-incision TAP and rectus sheath blocks and the placement of surgically sited TAP catheters.
ESP catheter group
Pre-induction, with the patient seated upright, and after intravenous administration of 1-2 mg of midazolam, 5-10 mcg/kg of intrathecal morphine was injected.
The T7 vertebra was identified with ultrasound and the level marked. The upper back was then prepared in a sterile fashion. At the level of T7, by scanning from lateral to medial in a parasagittal plane, the transverse process was identified. The skin was infiltrated with subcutaneous lidocaine 1% and an 18G Tuohy needle (PAJUNK®) was inserted under ultrasound guidance using an in-plane approach in a caudal to cranial direction until contact was made with the transverse process. 20 ml of 0.25% bupivacaine was injected to open up the fascial plane between the transverse process and the erector spinae muscle, and a catheter was then introduced and left 5 cm in the space. If the surgical incision was planned to cross the midline of the abdomen, bilateral ESP catheters were placed.
Induction of anaesthesia then proceeded with intravenous fentanyl, propofol and rocuronium, and anaesthesia was maintained with sevoflurane in oxygen and air. Intraoperative analgesia included intravenous fentanyl boluses, paracetamol and a NSAID as appropriate. At the end of the surgery, a bolus of 10 ml of 0.25% bupivacaine was injected through each catheter and an infusion of 0.15% bupivacaine at 10ml/hour was commenced and continued for 5 days. Regular paracetamol and NSAIDs were administered in the absence of contraindications, and rescue analgesia was administered as required in the form of subcutaneous or oral oxycodone (OxyNorm).
Standard analgesia group
Pre-induction, with the patient seated upright, and after intravenous administration of 1 mg-2 mg of midazolam, 5 mcg/kg-10 mcg/kg of intrathecal morphine was injected.
Induction of anaesthesia then proceeded with intravenous fentanyl, propofol and rocuronium, and anaesthesia was maintained with sevoflurane in oxygen and air. After induction of anaesthesia and prior to incision, a rectus sheath and subcostal TAP block was performed bilaterally (40 mls-60 mls 0.25% bupivacaine). Intraoperative analgesia included intravenous fentanyl boluses, ketamine, paracetamol and a NSAID as appropriate. At the end of the surgery, unilateral or bilateral TAP catheters were placed by the surgical team. A bolus of 10 ml of 0.25% bupivacaine was injected through each catheter and an infusion of 0.15% bupivacaine at 10 ml/hour was commenced and continued for 5 days. Regular paracetamol and NSAIDs were administered in the absence of contraindications, and rescue analgesia was administered as required in the form of intravenous PCA morphine.
Postoperatively all patients in both groups were monitored overnight in a HDU and were reviewed by the anaesthetic registrar before discharge to a surgical ward the following day. Patients were followed up daily for the next 7 days.
Outcome measurements
The primary outcome measure was opioid consumption. We used Oral Morphine Equivalents (OME) for statistical analysis.
Secondary outcomes were
- Pain scores at rest and on movement
- Time to resumption of oral fluids
- Time to resumption of solids
- Nausea and vomiting
- Surgical complications
- Length of hospital stay
- Physiotherapy outcomes
- Number of physiotherapy contacts
- Postoperative day of return to functional baseline
- Postoperative day weaned off supplemental oxygen
- Occurrence of postoperative respiratory complications
We used a 2-page paper datasheet to record baseline demographic data and blood test results as well as intraoperative and postoperative analgesia, postoperative opioid requirements, pain scores at rest and with movement, incidence of nausea and vomiting, antiemetics required, time to resumption of oral fluids, time to resumption of solids, physiotherapy outcomes, surgical complications and length of hospital stay.
Information was obtained from a number of sources. Demographic details were in the admission note in the patient medical chart, a paper record in St Vincent’s University Hospital. The HDU nursing notes are recorded in paper form, and these notes are stored separately in the medical chart. They contained information from the first 24 hours on pain scores, analgesia, nausea and vomiting and antiemetics. For postoperative Day 2 to 7, the data was collected from the nursing notes, the early warning scoring chart, the PCA forms and acute pain nurse’s notes. The information on gastrointestinal function was recorded in the dietetic notes. The physiotherapy outcomes with predefined parameters were documented in the medical chart.
Data management
All data was collected on a paper audit form initially. This was subsequently recorded in a coded database, on a password protected file, in line with data protection regulations. No patient identifying data was removed from the grounds of St Vincent’s University Hospital.
Statistical analysis
We conducted our statistical analyses using R, running on rStudio Version 1.1.383. We performed simple descriptive statistics initially: Fisher’s exact test was used for categorical variables, t-tests were used for non-skewed continuous variables and Mann-Whitney U tests were used for skewed continuous variables.
We used a method derived by O’Keeffe, et al. [28], which assumes a positively skewed distribution for the outcome data, to calculate the power size. We used a 90% power, a 5% significance level and a target of a 50% reduction in opioid usage in the ESP block group.
We calculated a sample size of 24 for the full study. As we were performing a pilot, we used 0.2 to indicate significance.
Results
Study population
A total of 22 patients were studied, 10 in the ESP group and 12 in the standard analgesia group. In the ESP group 70% were female compared with 25% in the non-ESP group (p=0.08). There was a statistically significant difference in the BMI between the two groups, with the ESP group having a mean BMI of 22.02 and the standard analgesia group with a mean of 28.24 (p<0.001). There was no statistical difference between the groups in ASA classification, age, type of surgery or length of surgery (p values 1, 0.35, 1 and 0.34 respectively) [Table 1].
Intraoperative management
Intrathecal morphine was standard treatment in both arms. Ketamine boluses were given as part of standard intraoperative management in the standard analgesia group. In the ESP group more intraoperative fentanyl and ondansetron (p value 0.17 and 0.11 respectively) were given. There were no other significant differences between the groups [Table 2].
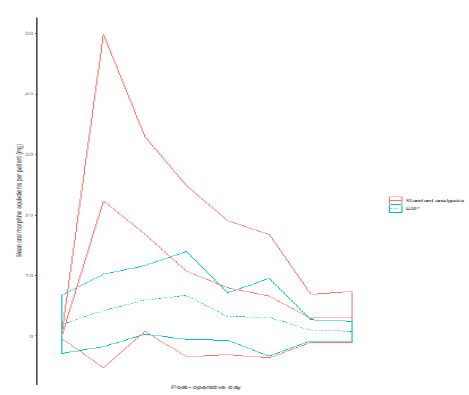
Primary outcome
There was a significant reduction in total oral morphine equivalents from Day 0-7 in the ESP group, with a reduction from a mean of 54 in the standard analgesia group to a mean of 14.38 in the ESP group (p=0.05). [Table 3] This reduction was most marked on Day 0-5. (Figure 1). There was no significant difference in the amount of iv fentanyl received in the first 24 hours postoperatively.
Secondary outcomes
There was no significant difference in the pain scores on Days 0-5 postoperatively between the two groups, either at rest or on movement. There were significantly reduced pain scores in the ESP group on postoperative Day 6-7, with the median pain score on movement 0 in the ESP group and 1.5 in the standard analgesia group (p=0.02) [Table 4].
There was no significant difference in the day at which patients returned to liquid diet between the two groups. However, 90% of the ESP group had returned to po solids by day 5 compared with only 50% of the standard analgesia group (p=0.07) [Table 5].
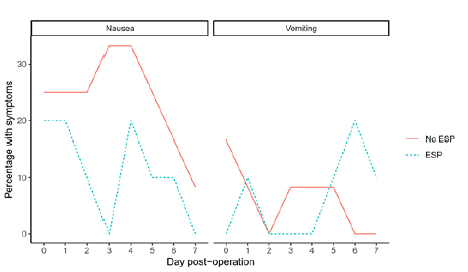
There was a trend towards reduced nausea on the earlier postoperative days in the ESP group (p=0.1 on Day 3) (Figure 2). However the risk of vomiting during day 6-7 in the ESP group was higher as a patient in the ESP group who had resumed PO solids on Day 3 then started vomiting on Day 6 and 7. This settled quickly with conservative management. Incidentally this patient had received no postoperative opiates at all. Fisher’s exact test was used to compare groups [Tables 6 and 7].
| Table 1: Patient demographics. | ||||
|---|---|---|---|---|
| ESP(n=10) | Standard analgesia(n=12) | p-value | ||
| Gender (%) | 7 (70%) female | 3 (25%) female | 0.08 | |
| Whipple’s procedure (%) | 6 (60%) | 8 (66.67%) | 1 | |
| Liver resection (%) | 4 (40%) | 4 (33.33%) | - | |
| Age (mean, SD) | 62.00 ± 9.39 | 66.92 ± 14.59 | 0.35 | |
| ASA (median,%) | 2 (100%) | 2 (80%) | 1 | |
| BMI (mean, SD) | 22.02 ± 1.54 | 28.24 ± 3.93 | <0.001 | |
| Length of Surgery in minutes (mean, SD) | 170.50 ± 79.00 | 206.25 ± 93.54 | 0.34 | |
| Table 2: Patient demographics. | ||||
|---|---|---|---|---|
| ESP(n=10) | Standard analgesia(n=12) | p-value | ||
| Intrathecal morphine (mcg) (mean, sd) | 685 ± 264 | 783 ± 180 | 0.33 | |
| IV Fentanyl (mcg) (mean, sd) | 255 ± 98 | 192 ± 110 | 0.17 | |
| IV Paracetamol (gm)(median, range) | 0 (0-1) | 0.50 (0-1) | 0.37 | |
| Ondansetron (mg) (mean, sd) | 4.40 ± 1.26 | 3.33 ± 1.56 | 0.11 | |
| Dexamethasone (mg)(median, range) | 4 (0-8) | 0 (0-16) | 0.54 | |
| Ketamine (mg) (median, range) | • | 0 (0-50) | 0.03 | |
| Table 3: Opioid requirements. |
|
|||
|---|---|---|---|---|
| ESP(n=10) | Standard analgesia(n=12) | P-value | ||
| Total oral morphine equivalents day 0-1 (mean, range) | 1.3 (0.0–30.0) | 17.8 (0.0–100.0) | 0.1 | |
| Total oral morphine equivalents day 2-5 (mean, range) | 10.1 (0.0–67.5) | 29.5 (2.5–160.5) | 0.12 | |
| Total oral morphine equivalents day 6-7 (mean, range) | 1.3 (0.0–5.0) | 2.5 (0.0–22.5) | 0.35 | |
| Total iv fentanyl day 0-1 (mean, range) | 50.0 (0.0–280.0) | 90.0 (0.0–200.0) | 0.81 | |
| Total oral morphine equivalents day 0-7 (mean, range) | 14.4 (0.0–102.5) | 54.0 (2.5–161.0) | 0.05 | |
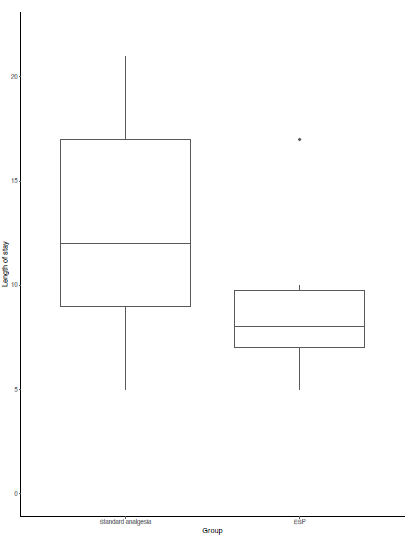
There was also a significantly decreased length of hospital stay in the ESP group from a median of 12 days in the standard analgesia group to a median of 8 days in the ESP group (p=0.06) [Table 8]. None of the patients in either the ESP group or the standard analgesia group had any respiratory complications. Patients in the ESP group were weaned from oxygen one day sooner than those in the standard analgesia group (p=0.02).
There were no serious adverse events or surgical complications reported in either group.
The box plot (Figure 3) shows that there is a reduced total length of stay in the ESP group of patients. Even the most extreme outlier in the ESP group only corresponded to the 3rd quartile in the standard analgesia group.
Discussion
The ESP block is a relatively new technique, which has been shown to be effective in thoracic, bariatric, hernia and breast surgery and for rib fracture pain amongst others [23,25,26,29,30]. There have been no studies to date looking at ESP blocks in major HPB surgery.
We performed a retrospective audit study to compare ESP blocks and catheters to standard analgesia in major HPB surgery. Our results show a significant reduction in opiate consumption after major HPB surgery in the ESP group, with an overall reduction in Day 0-7 oral morphine equivalents from 54 to 14.38 (p=0.05). This occurred despite no difference in pain scores from day 0-5 post-operatively between the 2 groups, and a reduction in pain scores in the ESP group on Day 6-7, especially on movement (p=0.02). This is consistent with the trend already seen in the reports of ESP blocks used elsewhere but our study demonstrates it with a comparison to a standard analgesia group. 90% of our patients in the ESP group returned to PO solids by Day 5 compared to only 50% in the standard analgesia group, presumably due to less GI side effects, although we were unable to show a significant difference in nausea and vomiting between the 2 groups. We also showed a significant decrease in length of hospital stay between the 2 groups with a reduction from a median of 12 days in the standard analgesia group to a median of 8 days in the ESP group.
| Table 4: Pain scores. | ||||
|---|---|---|---|---|
| ESP(n=10) | Standard analgesia(n=12) | P-value | ||
| Pain score at rest at day 0-5 (median, range) | 0 (0–3.67) | 0 (0–2.67) | 1 | |
| Pain score on movement day 0-5 (median, range) | 2.75 (0-5.83) | 3.25 (0–5.17) | 0.51 | |
| Pain score at rest day 6-7 (median, range) | 0 (0–0) | 0 (0–3) | 0.19 | |
| Pain score on movement day 6-7 (median, range) | 0 (0–3) | 1.5 (0–7) | 0.02 | |
| Table 5: Resumption of po fluids and solids. |
|
|||
|---|---|---|---|---|
| ESP(n=10) | Standard analgesia(n=12) | P-value | ||
| Percentage returned to liquid at day 0-6 | 10 (100%) | 11 (91.67%) | 1 | |
| Percentage returned to liquid at day 7+ | 0 (0%) | 1 (8.33%) | - | |
| Percentage returned to solid at day 0-6 | 9 (90%) | 6 (50%) | 0.07 | |
| Percentage returned to solid at day 7+ | 1 (10%) | 6 (50%) | • | |
| Table 6: Nausea. | ||||
|---|---|---|---|---|
| ESP | Standard analgesia | P-value | ||
| Day 0 | 20% | 25% | 1 | |
| Day 1 | 20% | 25% | 1 | |
| Day 2 | 10% | 25% | 0.59 | |
| Day 3 | 0% | 33.30% | 0.1 | |
| Day 4 | 20% | 33.30% | 0.65 | |
| Day 5 | 10% | 25% | 0.59 | |
| Day 6 | 10% | 16.70% | 1 | |
| Day 7 | 0% | 8.30% | 1 | |
| Table 7: Vomiting. | ||||
|---|---|---|---|---|
| ESP | Standard analgesia | P-value | ||
| Day 0 | 0% | 16.70% | 0.48 | |
| Day 1 | 10% | 8.30% | 1 | |
| Day 2 | 0% | 0% | _ | |
| Day 3 | 0% | 8.30% | 1 | |
| Day 4 | 0% | 8.30% | 1 | |
| Day 5 | 10% | 8.30% | 1 | |
| Day 6 | 20% | 0% | 0.21 | |
| Day 7 | 10% | 0% | 0.48 | |
Of note regarding patient demographics, there was a significant difference in BMI between the 2 groups with a mean BMI of 28.24 in the standard analgesia group, compared to a mean BMI of 22.02 in the ESP group. While a lower BMI probably makes the ultrasound guided ESP procedure technically easier, it is unlikely to translate to a reduced risk of postoperative pain after major open surgery.
The most obvious limitation of our study is the small sample size with only 12 patients in the standard analgesia group and 10 patients in the ESP group. It was limited to 3 consultant anaesthetists and 2 consultant surgeons with the total number of HPB anaesthetists and surgeons in our institution being 7 and 7 respectively. The reason for this is that a single Consultant Anaesthetist pioneered the use of ESP catheters in our institution for major HPB surgery in 2016. The technique has since been adopted into routine practice by a further 4 of 7 Consultant Anaesthetists.
The study was in the form of a retrorospective audit, so anaesthesia and analgesia, although practice is relatively standardized, was not administered in accordance with a protocol. Supplemental postoperative analgesia was in the form of nurse administered intravenous fentanyl, NSAIDs, paracetamol, tapentadol, oxycodone and patient administered PCA morphine. These are administered or not based on renal function, liver function and safe physiological parameters. This can introduce an element of bias, as there is potential for the dose administered and titration to be based on what is perceived to be adequate by the nurse rather than the patient.
HPB surgery poses unique challenges in terms of postoperative pain management, which has both visceral and somatic components, with the nerve supply to most HPB structures coming from the coeliac plexus, while the somatic component is mainly via the intercostal nerves. Epidural analgesia has been considered the optimal analgesic technique for HPB surgery, but with limitations. With novel techniques in regional anaesthesia, there is the potential to use lower risk techniques which can provide good quality analgesia and may alter patient outcomes. It is unclear whether ESP blocks provide both somatic and visceral analgesia or somatic analgesia alone [23,24]. From our clinical experience, it appears more likely that they provide good somatic analgesia but limited visceral analgesia, and an alternate adjunctive analgesic is required for the first 24 hours for visceral pain (hence our use of intrathecal morphine).
Enhanced recovery protocols are increasingly emphasizing opioid sparing or opiate free anaesthesia. Ultrasound-guided ESP block is a myofascial plane block that provides analgesia for thoracic or abdominal segmental innervation depending on the level of the injection site. The significant advantages of ESP block compared to epidural or paravertebral block relate to the relative ease, simplicity and safety of the block. Ultrasound is used to determine the vertebral level of insertion and identify the erector spinae muscle over the transverse process. Once the erector spinae plane has been opened with an initial bolus of local anaesthetic, a catheter can be threaded for continuous infusion of local anaesthetic postoperatively. As the ESP block is a relatively new block, it is difficult to define its exact risk profile. However, as the placement of the needle down onto the transverse process is performed in plane under ultrasound guidance, and the target plane is relatively remote from major neural or vascular structures and the pleura, theoretically safety should be improved. The rare but catastrophic risk of damage, either directly or indirectly, to neuraxial structures as with epidural and the up to 1% risk of pneumothorax with paravertebral block are theoretically much less of an issue with ESP block.
Conclusion
Major HBP surgery requiring large upper abdominal incisions will always present a challenge to the anaesthetist in terms of balancing adequate analgesia with the adverse effects of the mode of delivery of such analgesia. The ESP block in combination with a multi-modal analgesic approach offers a safe alternative to epidural and opiate based analgesia. Our study shows that the patients in the ESP group received significantly less opiates, had equivalent or lower pain scores, earlier resumption of PO solids and had a shorter lengths of hospital stay than the standard analgesia group. Given these positive trends, we plan to carry out a larger randomised control trial.
Acknowledgments
The authors would like thank the nursing staff in the post anaesthesia care unit, the Bloomfield High Dependency Unit, and the hepatobiliary theatre staff for accommodating and assisting with the conduct of this trial, and without whose support the trial would not have proceeded.
Declaration of Competing Interest
None
References
- Popping DM, Elia N, Marret E, Remy C, Tramer MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: A meta-analysis. Arch Surg. 2008, 143:990-9.
[Crossref], [Google Scholar], [Indexed]
- Wijeysundera DN, Beattie WS, Austin PC, Hux JE, Laupacis A. Epidural anaesthesia and survival after intermediate-to-high risk non-cardiac surgery: A population-based cohort study. Lancet. 2008, 372: 562–9.
[Crossref], [Google Scholar], [Indexed]
- Rigg JRA, Jamrozik K, Myles PS. Epidural anaesthesia and analgesia and outcome of major surgery: A randomised trial. Lancet. 2002, 359: 1276–82.
[Crossref], [Google Scholar], [Indexed]
- Park WY, Thompson JS, Lee KK. Effect of epidural anesthesia and analgesia on perioperative outcome: A randomized, controlled Veterans Affairs cooperative study. Ann Surg. 2001, 234: 560-569.
[Crossref], [Google Scholar], [Indexed]
- Rodgers A, Walker N, Schug S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trials. BMJ. 2000;321:1493.
[Crossref], [Google Scholar], [Indexed]
- Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: Causes and management. Br J Anaesth 2012, 109: 144–54.
[Crossref], [Google Scholar], [Indexed]
- Lee CH, Kim H, Han IW, Kim SM, Kwak BS, Baik YH, et al. Effect of polylactic film (Surgi-Wrap) on preventing postoperative ileus after major hepato-pancreato-biliary surgery. Ann Hepatobiliary Pancreat Surg. 2016, 20: 191–6.
[Crossref], [Google Scholar], [Indexed]
- Gan TJ, Robinson SB, Oderda GM, Scranton R, Pepin J, Ramamoorthy S. Impact of postsurgical opioid use and ileus on economic outcomes in gastrointestinal surgeries. Curr Med Res Opin. 2015, 31: 677–86.
[Crossref], [Google Scholar], [Indexed]
- Guay J, Nishimori M, Kopp S. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database Syst Rev. 2016; 7: CD001893.
[Crossref], [Google Scholar], [Indexed]
- Papadopoulos V, Filippou D, Manolis E, Mimidis K. Haemostasis impairment in patients with obstructive jaundice. J Gastrointestin Liver Dis. 2007;16: 177–86.
[Crossref], [Google Scholar], [Indexed]
- Shontz R, Karuparthy V, Temple R, Brennan TJ. Prevalence and risk factors predisposing to coagulopathy in patients receiving epidural analgesia for hepatic surgery. Reg Anesth Pain Med. 2009, 34: 308–11.
[Crossref], [Google Scholar], [Indexed]
- De Pietri L, Montalti R, Begliomini B, Scaglioni G, Marconi G, Reggiani A, et al. Thromboelastographic changes in liver and pancreatic cancer surgery: Hypercoagulability, hypocoagulability or normocoagulability? Eur J Anaesthesiol. 2010, 27: 608–16.
[Crossref], [Google Scholar], [Indexed]
- Wang LP, Hauerberg J, Schmidt JF. Incidence of spinal epidural abscess after epidural analgesia: A national 1-year survey. Anesthesiology. 1999, 91: 1928–36.
[Crossref], [Google Scholar], [Indexed]
- Lim HJ, Koay CK, Lee LS. Postoperative coagulopathy after liver resection--implications for epidural analgesia. Anaesth Intensive Care. 2006; 34: 118–9.
[Crossref], [Google Scholar], [Indexed]
- De Pietri L, Siniscalchi A, Reggiani A, Masetti M, Begliomini B, Gazzi M, et al. The use of intrathecal morphine for postoperative pain relief after liver resection: A comparison with epidural analgesia. Anesth Analg. 2006, 102: 1157–63.
[Crossref], [Google Scholar], [Indexed]
- Mungroop TH, Veelo DP, Busch OR, Dieren SV, Gulik TMV, Karsten TM, et al. Continuous wound infiltration versus epidural analgesia after hepato-pancreato-biliary surgery (POP-UP): A randomised controlled, open-label, non-inferiority trial. Lancet Gastroenterol Hepatol. 2016;1:105–13.
[Crossref], [Google Scholar], [Indexed]
- Abdelsalam K, Mohamdin OW. Ultrasound-guided rectus sheath and transversus abdominis plane blocks for perioperative analgesia in upper abdominal surgery: A randomized controlled study. Saudi J Anaesth. 2016;10: 25–8.
[Crossref], [Google Scholar], [Indexed]
- Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011, 66: 465–71.
[Crossref], [Google Scholar], [Indexed]
- Beverly A, Kaye AD, Ljungqvist O, Urman RD. Essential elements of multimodal analgesia in Enhanced Recovery After Surgery (ERAS) Guidelines. Anesthesiol Clin. 2017, 35: e115–43.
[Crossref], [Google Scholar], [Indexed]
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997, 78: 606–17.
[Crossref], [Google Scholar], [Indexed]
- Feldheiser A, Aziz O, Baldini G, Cox BPBW, Fearon KCH, Feldman LS, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: Consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016, 60: 289–334.
[Crossref], [Google Scholar], [Indexed]
- Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: A review. JAMA Surg. 2017, 152: 691–7.
[Crossref], [Google Scholar], [Indexed]
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016, 41: 621–7.
[Crossref], [Google Scholar], [Indexed]
- Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018, 43: 567–71.
[Crossref], [Google Scholar], [Indexed]
- Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral Erector Spinae Plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72: 452–60.
[Crossref], [Google Scholar], [Indexed]
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A report of 3 cases. Reg Anesth Pain Med. 2017;42: 372–6.
[Crossref], [Google Scholar], [Indexed]
- Nair S, McGuinness S, Masood F, Boylan JF, Conlon NP. Erector spinae plane blocks in major hepatopancreaticobiliary surgery: A case series. A A Pract. 2019;13: 332–4.
[Crossref], [Google Scholar], [Indexed]
- O’Keeffe AG, Ambler G, Barber JA. Sample size calculations based on a difference in medians for positively skewed outcomes in health care studies. BMC Med Res Methodol. 2017;17:157.
[Crossref], [Google Scholar], [Indexed]
- Selvi O, Tulgar S. Use of the ultrasound-guided erector spinae plane block in segmental mastectomy. Turk J Anaesthesiol Reanim. 2019;47:158–60.
[Crossref], [Google Scholar], [Indexed]
- Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: A retrospective cohort study. Anaesthesia. 2019, 74: 585–93.
[Crossref], [Google Scholar], [Indexed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.