Revisiting Public Health Challenges in the New Millennium
- *Corresponding Author:
- Dr. PR Sreelakshmi
Department of Community Medicine, Government Medical College, Thiruvananthapuram, Kerala, India.
E-mail: dr.pr2003@gmail.com
Abstract
Positive Health of the communities could only be brought out through the interrelationship between conventional health sector and other development sectors. It was a dream that came true when World Health Organization (WHO) accepted Primary Health Care (PHC) as the major tool to achieve its proposed goal of Health For All (HFA) by 2000 A.D., but we could not succeed as expected. Now we have the Millennium Development Goals (MDG), which place health at the heart of development but the achievements in health is still challenging. The literature search in this article has been conducted in Pub Med and Google scholar, with the aim to draw references to discuss the major health issues and ways to tackle them. The current article briefly narrates the burden and complexities of challenges faced by the present global health. Revisiting the concept of PHC and reaffirming our solidarity to this philosophy is the need of this hour.
Keywords
Asia, Development goals, Millennium, Public health, Public health challenges, Primary healthcare
Introduction
The organized efforts of humanity towards a healthier community are as old as the human civilization. It has faced lots of achievements as well as setbacks in its journey through history, but the revolution of knowledge that happened after the renaissance (15th century) and the public health initiatives thereafter, shaped the modern philosophy of health. The World Health Organization’s (WHO) definition of health added much to the concept.[1] As wellbeing is closely linked to the development sectors conventionally considered outside the purview of health,[2] the new definition of Health broadens to include health and development. Now it has entered the post modern era influenced much by the economic reforms and globalization. Eradication of smallpox by an international campaign (1977) and massive achievements in the control of communicable diseases had kindled lot of hope regarding the future of health.[3-5]
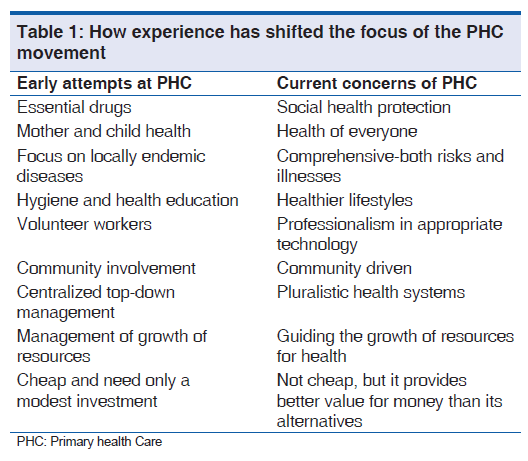
The acceptance of the principle of Primary Health Care (PHC) by the WHO has spearheaded many activities towards achieving its goal of Health For All (HFA) by 2000 A.D.[6] Although the member countries of WHO formulated their health policies according to the broad vision of HFA 2000, the campaign was not successful in bridging the huge health gap across the world.[7] The United Nation’s Millennium Development Goals (MDG), was introduced as a philosophical successor of WHO’s HFA by 2000 A.D. MDG envisaged the overall development as the outcome of improvements in health, education, poverty eradication, gender equity, environmental sustainability, and international co-operation. Health sector does not have independent existence. It is closely related to other sectors like education and agriculture. Interestingly, the commission on social determinants of health by the international health organization explained how the health of individuals and communities are affected by inputs from other developmental sectors.[8] Ill health can be tackled effectively only if social determinants are addressed to. Diseases are distally determined by certain social factors and poor health in turn leads to unfavorable social conditions. This acts as a vicious cycle and, therefore, the development of other related sectors becomes inevitable for improvements in health of a community. Poverty is a social evil closely related to ill health across the world, more evident in the under developed nations. The modern epidemic of Human Immunodeficiency Virus-Acquired Immuno Deficiency Syndrome (HIV-AIDS) is a striking example of this mechanism. Some studies conducted in Africa give evidence to suggest that the poorer sections of the population have a much higher risk of contracting HIV than the non poor community,[9] and there are other studies from the same region which describes the devastating effects of HIV on the socioeconomic conditions.[10] This mechanism has played a definite role in blowing up the disease burden into epidemic proportions. The situation in Scandinavian countries and Sri Lanka[11] set a positive example where the better health nurtured by the society had given its toll on overall social development. But the challenges faced now in the sector of global health are much more complex. Visualizing a direct linear relation between social development and the health of the community has become obsolete. The relation between community and health is largely altered by the time, place, and personal situations. The complexities of culture and customs, economic situations, geography, ethnicity, and political situations make the challenges related to public health specific for every nation. WHO along with all those interested in the well being of humanity is revisiting the concept of PHC and reaffirming their solidarity to this philosophy. This is the background of the comprehensive outlook of PHC that has appeared in the World Health Report of 2008 [Table 1]. The policy argued that the initiatives of primary healthcare could not be considered cheap because, the philosophy need much resources from the community other than the money to initiate and sustain the activity.
In this fast changing world, the challenges in the health sector are also dynamic. The principle of PHC as envisaged at Alma Ata should be highlighted and reiterated to suit the changing health needs. The World Health Report 2008 ‘Primary Health Care - now more than ever’ rightly discusses this concept in a comprehensive manner. The literature search in this article has been conducted with the aim to draw references to discuss the major health issues and ways to tackle them.
Materials and Methods
The article is based on a review of literature done through electronic databases. The search in pubmed/medline was conducted using ‘primary health care’, ‘economic development’, ‘human development’, ‘emerging communicable disease’ and ‘chronic disease’ as medical subject headings terms. These terms were used as key words in search in web (google scholar).
The Challenges
The challenges faced by the new world in the field of health can be broadly summarized in the following headings:
1. Old problems not yet solved
2. Health transition
3. Equity related issues and deprivation
4. Globalization
5. Economic and financial problems
6. Public health ethics
7. Environmental issues including climate change.
Old problems not yet solved
This heading brings into light some issues which have remained as major public health concerns for centuries. The absolute and relative magnitude of these issues in various communities may have changed, but they still stay back as serious public health concerns especially in the under developed countries. Health issues that are to be addressed are many, but in this article we have selected two prototypical sets of issues which have long been contributing to human suffering.
Maternal and child health including vaccine preventable diseases
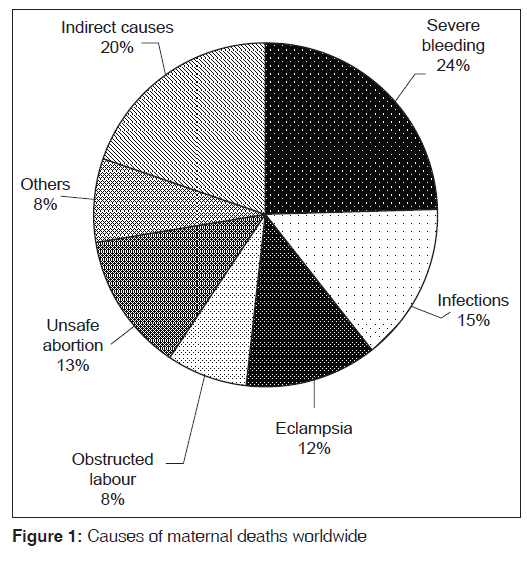
The indicators of maternal health are varying very much across the world. In developed nations the maternal mortality ratio averages at 13 per 100,000 live births; in developing world, this is 440 for the same denominator. The Figure 1 shows the causes of maternal deaths worldwide.[12]
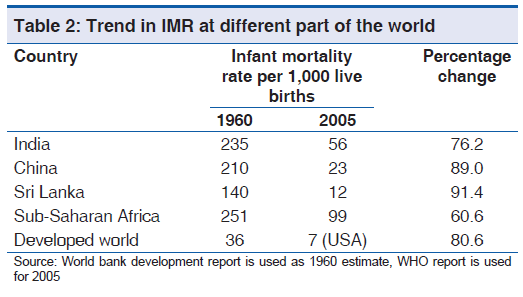
In global terms, child mortality rates in developing regions are continuously declining.[13] But 35% of Africa’s children face a greater risk of dying today, as compared to 10 years ago.[14] Almost half of all deaths among children under five occur in this region, where progress has slowed down due to lack of preventive care and treatment, fragile health systems, and socioeconomic stagnation due to conflicts, political instability and HIV/AIDS.[15-19] The condition in India is also not very satisfactory in this context.[20,21] The Table 2 shows that the achievements measured by infant mortality rate (IMR), in past 45 years are much less than other countries with comparable economies. The third world countries have not achieved what the developed nations achieved 50 years back.
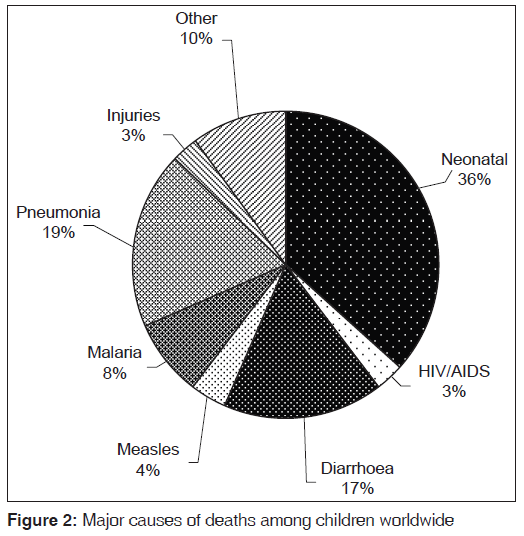
It is evident from various experiences that the political will and leadership is very crucial to make palpable improvements in maternal and child health issues. It is interesting to note that majority of child deaths worldwide are attributable to very few conditions like pneumonia, diarrheal diseases, measles, malaria, and malnutrition[22] [Figure 2] and most of them could be avoided through more wide spread use of existing interventions. Heavy toll of these deaths occur in third world countries. Vaccine preventable diseases are still highly prevalent in third world countries and these contribute significantly to the heavy death toll among children here.[23]
Food, nutrition, and poverty
Under-nutrition is still a major cause of death among children under the age of five years and poverty is considered as the most potent distal determinant of death. In this context, the United Nations has accepted the reduction of extreme poverty and hunger as the 1st goal in MDG. It is well-known that malnutrition in children make them more vulnerable to ill health due to communicable diseases especially to diarrheal diseases and pneumonia.[24] But evidences are accumulating that undernourished children are more prone for non-communicable diseases like diabetes in their future life.[25] Thus, it is logical to believe that the millions of children under starvation because of economic deprivation and political instability all around the world will contribute to the global burden of disease even at their adulthood.
The food safety of the world, especially that of African and Asian countries is again under threat in the context of climatic change and extreme weathers.[26] The political instabilities and economic crisis in these countries makes the situation. Millions still struggle for even a single meal per day and even deaths due to starvation are being reported from several African countries. Paradoxically, the beginning of the millennium is witnessing a paradigm shift in the utility of food crops. Reports are coming out that more and more food grains are used for energy production in developed countries. It is shameful that food materials are used as fuels[27] when about 1 billion people globally are living in extreme poverty on an income of below $1 a day and starving.
Health transition
Health transition means the changes in health that follow an identifiable pattern that occur over a relatively long period of time.[28] It includes changes in the pattern of disease, disabilities, death as well as changes in the type of organized social response to health conditions. Transformations are more complex in middle income countries where the social inequalities are deep. Infectious diseases have lost their previous predominance but still maintain a major position in the epidemiologic profile. At the same time absolute and relative importance of non-communicable diseases and injuries has increased. Another important attribute of the transition is that it is not always unidirectional from communicable diseases to non-communicable disease. A reversal of trend known as “counter transition” is occurring in some areas e.g. AIDS, TB, and Arboviral diseases. Some of the transition-related health issues are discussed below.
Emergence of non-communicable diseases
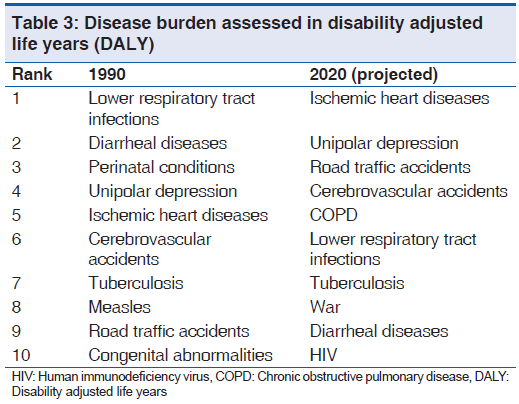
Increased mortality from non-communicable diseases in developing countries is reflecting shifting patterns of lifestyle. Ischemic heart disease and cerebrovascular disease combined constitutes 16% of deaths in 15-59 year age group.[29] The number of diabetic patients would be doubled by first quarter of the century to 366 million, greatly outnumbering the population growth.[30] Cancer has emerged as one among the major killer diseases, so are mental diseases and suicides [Table 3].[31] Health problems posed by visual impairment, accidents, injuries, unhealthy life style, and work related problems, conflicts, war, and terrorism are assuming bigger challenge now as shown in Table 3.[31]
HIV/AIDS, tuberculosis and malaria
The leading causes of deaths in the third world nations clearly indicate the socio-economic backwardness prevailing in those areas. After pneumonia and diarrheal diseases, HIV/AIDS has emerged as the most common cause of mortality in the third world nations.[32] It has become one of the leading causes of mortality among adults aged 15-59 years.[29] The development of drug resistance has emerged as a huge challenge for HIV and Tuberculosis (TB). The emergence of HIV-AIDS had made the burden of TB more intense and complicated. Resistance to conventional anti-TB drugs is well-documented, but the emergence of resistance to the second line drugs, the extensively drug resistant Tuberculosis (XDR-TB)[33-35] and totally resistant Tuberculosis (TDR-TB),[36-38] which is considered to be virtually untreatable, has added much burden to the already challenging scenario. The statistics available in the WHO’s regional data strongly indicate the existing health gap between countries [Table 4].[39] Malaria is another major problem to which half of the world population is at risk and it causes about 3,000 deaths every day. The deaths are mostly caused by a single species, Plasmodium falciparum. The burden of Malaria is accentuated by the increasing drug resistance and insecticide resistance. Recent data indicate that there are countries where death rate due to Malaria is as high as 2.4 per 1,000,[39] which is comparable to the overall death rate of some developed countries. The deaths due to Malaria is highest in African region with a median of 94 per 100,000 population.[39]
| WHO region | Morbidity in terms of prevalence per 100,000 population | Cause specific mortality in 100,000 population | ||
|---|---|---|---|---|
| TB without HIV infection (all age) | HIV (15-49 years) | TB without HIV infection | HIV | |
| Africa | 475 [398-563] | 4.7 [4.5-5.0] | 52 [48-58] | 177 [151-205] |
| America | 38 [30-48] | 0.5 [0.4-0.6] | 2.1 [1.8-2.6] | 18 [14-22] |
| South-east Asia | 278 [186-398] | 0.3 [0.3-0.3] | 27 [20-35] | 13 [12-15] |
| Europe | 63 [49-81] | 0.4 [0.3-0.4] | 6.9 [5.7-8.3] | 19 [15-23] |
| Eastern Mediterranean | 174 [116-253] | 0.2 [0.2-0.2] | 6 [5.6-7.4] | 17 [12-22] |
| Western Pacific | 160 [107-231] | 0.1 [0.1-0.1] | 13 [10-17] | 4 [2.9-4.8] |
HIV: Human immunodeficiency virus, WHO: World health organization’s, TB: Tuberculosis
Table 4: Global burden of tuberculosis and HIV across the WHO regions
Emergence of new mosquito-borne diseases
The emergence of arboviral infections contributed by the widened geographical distribution of Aedes mosquitoes is the hallmark of the transition. The world is experiencing a pandemic of Chikungunya along with Dengue.[40] Future trends also favoring huge morbidity by arthropod borne viruses in coming decades.[41] Multiple factors including the climate change, movement of people, lack of environmental sanitation, and enhanced adaptability of vectors make all communities vulnerable to such infections.
Equity related issues and deprivation
Globalization and neo liberalization has definitely improved the average health indicators. However, it has also led to widening of the existing health gap across countries, adding on to the health inequities existing worldwide. These inequities are linked to economic deprivation, gender status, cultural alienations, and ethnicity. The needy are often kept away in terms of access and provision of heath related services both in quantity and quality. Equity related issues exist even in basic amenities of human life such as food and water. For some individuals and communities, there is no food or resources that can be translated to food grains, for some the available food is not nutritious.[42] Compared to other goods and services, the cost of food is high in terms of purchasable parity. It requires as much attention as it was perceived at Alma-Ata.
Globalization
All over the world, social and economic integration has accelerated in the past decade. The World health report 2008 observes that, “globalization is putting the social cohesion of many countries under stress”. This has had direct and indirect consequences on health both in terms of communicable and non-communicable diseases.[43] One such effect is on the epidemiology of communicable diseases, opening of travel and trade routes between countries has been accompanied by the spread of diseases and their vectors.[44] At the same time, changing international rules concerning patent protection has decreased the access to essential medicines which widened the inequity related to health delivery.[45] Other issues like spread of diseases like severe acute respiratory syndrome and Avian flu, commercialization of medicine, cost escalation, reduced stake of the state in service provision etc., should also be considered as issues in this context.
Economical and financial issues
In India, the data of national sample survey organization 42nd Round observes that the contribution of Central Government in the field of health is only 1.65% of gross national product, and it provides only for 11.84% of the total health care expenditure. This bleak picture is repeated in almost every developing country. The healthcare expenditure is dominated by private sector in India and most of the African counties put much of the burden on the shoulders of the people through out-of-pocket treatment expenditure. Assistance from public funding and strategies of risk pooling are rudimentary in these settings which make the public vulnerable to catastrophic health expenditure. As compared to the affording sections that are covered by social or private insurance schemes, the underprivileged sector of the community is forced to make direct payments and are in a constant threat of heavy debts as public provision is grossly inadequate.[46] Financing in health sector is getting more and more complex now. External donors support the type of activities directed to achieve their vested interests. This process leads to a prioritization of health services which are different from the local needs.
Public health ethics
The ethical dimension of public health is largely based on the ‘Utilitarian principles’—‘Greatest good for greatest number’. But the voice of the third world, where almost 80% of the world population is residing, is often neglected during planning. The concerns of the marginalized people are often neglected in the planning at local level also. The science and technology has added different issues of ethical conflicts. A few of these have been mentioned below.
1. Organ and tissue transplant
2. Genetic engineering and cloning
3. Medical decisions against evidences – often driven by the market
4. Issues related to clinical trials – people from the third world countries are often subjected to clinical trials
Environment related issues
‘Protecting health from climatic change’ was the theme of world health day 2008. WHO has listed down impact of climate change in health.[47]
1. Extreme air temperatures and air pollution.
2. Floods, droughts and contaminated water raise disease risk.
3. Climatic effects on agriculture threaten increasing malnutrition.
4. A more extreme and variable climate can destroy houses, communities, and lives.
The growing problems related to urbanization, pollution of air, water and land, and exploitation of non-replenishable resources also add to the burden.
The Indian Perspective
India is a nation which suffers or is likely to suffer the ill effects of all the challenges listed above in a greater magnitude. It is the nation where more than one-sixth of the world population resides and is often challenged by its geographic and social diversities. The old world problems like high incidence of communicable diseases, low performance of maternal and child health indicators, and nutritional problems, especially that of women and children, are the issues that persist in almost all parts of the country even today. Health transition is also evident and will cause a great concern in future. It is expected that India will be facing the greatest burden of chronic non-communicable diseases like diabetes, hypertension, and heart disease in near future.[48] Deprivation related issues are often complicated by the caste system that strongly exists in the community apart from the economical and other social factors.[49,50] The globalization related issues also brings out additional risks to an Indian community as this country is considered as one of the largest markets and a growing economic power. Economic issues and provision in healthcare was always a concern in India where the public investment in health care, social assistance, and risk pooling are often meagre or made available only for a minority and the major share of healthcare expenditure is still out of pocket.[51] The provision from the central government was below one percentage of gross domestic product until recently. (It might have improved after the implementation of the new project, National Rural Health Mission).
The health system of the nation is limping in all core areas of PHC in terms of availability, acceptability, accessibility, and utilization of healthcare services. The provisions of basic facilities like institutional deliveries, attended by trained personnel have not been made widely available across the nation. As the practice of people in India is greatly governed by local beliefs and traditions, certain concepts like child birth in an institution still remains alien for a rural woman and her family (lack of acceptability). Coupled with ignorance, these acceptability issues lead to many unethical practices especially among the backward communities which are hazardous to health. The skewed distribution of the PHCs in rural areas along with poor transportation facilities leaves the needs of rural people unattended (lack of accessibility). The utilization of service is again limited by external factors. For example, the PHCs in most areas do not work round the clock and are not utilizable for the public in times of real need.
The lack of trained personnel is the major bottleneck in this country, hindering the provision of health services in various facilities. The country has widely adopted a system, which utilizes the services of multipurpose workers to deliver majority of the services.[52] The leadership in community health activities in rural seldom involves a doctor due to their scarcity. In this context, it is paradoxical that this country exports many of its health professionals to European and American nations. The regrettable fact is that this second most populous country in the world even finds it difficult to get trained multipurpose workers to serve in the field. International agencies like world bank have a definite role in identifying and accumulating resources in India whose health predict the global health because of the massive nature of its population. The role of each state inside the federal democratic system of India is crucial but often less discussed. As health, according to the constitution of India is a state subject, it is the primary responsibility of the state government to see the wellbeing of its public. The responsibility the individual states are not carried out satisfactorily at least in certain areas as evidenced by huge disparity of health indicators across the states. Decentralized planning which is implemented in India should help to generate local resources including human power. In short, the lack of resources in health could be tackled in four levels such as village level, state level, national level, and international level. However, the priority should be given to the lowest strata as what is envisaged in primary health care concept.
The Way Forward
We have to focus on risks rather than diseases, and primordial and primary prevention should be given emphasis because interventions in the distal determinants of health are more important in sustaining health and development of a nation.[8] Another suggestion is that it should focus on the comprehensive all-inclusive health of the community rather than the conventional maternal and child health centred approaches [Table 1].
Let us hope that the new initiative and the true spirit of PHC concept will help the humanity to face the challenges of the millennium in a better way. As Sir Rudolf Virchow (1849) has observed, “Medicine is a social science and Politics is medicine on a large scale”. We dream of a sustainable all-inclusive development through a decentralized and a democratic process. PHC is the way that we have, and we should have, in achieving our dreams.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19-22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
- Savedoff WD, de Ferranti D, Smith AL, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet 2012;380:924-32.
- Aylward B, Tangermann R. The global polio eradication initiative: Lessons learned and prospects for success. Vaccine 2011;29(Suppl 4):D80-5.
- Breman JG, de Quadros CA, Gadelha P. Smallpox eradication after 30 years: Lessons, legacies, and innovations. Introduction: Meeting objectives, summary and final statement. Vaccine 2011;29(Suppl 4):D3-5.
- Heymann DL, Brilliant L. Surveillance in eradication and elimination of infectious diseases: A progression through the years. Vaccine 2011;29(Suppl 4):D141-4.
- World Health Organization. Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978. Available from: http://www. who.int/hpr/NPH/docs/declaration_almaata.pdf [Last accessed on 2011 Dec 11].
- McIntyre E, Eckermann S. Health for all: Are we there yet? Aust J Rural Health 2007;15:390.
- World Health Organization. Commission on social determinants of health final report. Closing the gap in a generation. Available from: http://whqlibdoc.who.int/ publications/2008/9789241563703_eng.pdf [Last accessed on 2011 Dec 11].
- Magadi MA. The disproportionate high risk of HIV infection among the urban poor in Sub-Saharan Africa. AIDS Behav; 2012.
- Gentilini M, Chieze F. Socioeconomic aspects of human immunodeficiency virus (HIV) infection in developing countries. Bull Acad Natl Med 1990;174:1209-19.
- Country Health Profile Sri Lanka-South-East Asia R e g i o n a l O f f i c e . w w w . s e a r o . w h o . i n t / S r i _ l a n k a _ CountryHealthSystemProfile-SriLanka.
- World Health Organization. The World Health Report 2005: Make every mother and child count. Available from: http:// www.who.int/whr/2005/whr2005_en.pdf [Last accessed on 2001 Dec 11].
- Moser K, Shkolnikov V, Leon DA. World mortality 1950-2000: Divergence replaces convergence from the late 1980s. Bull World Health Organ 2005;83:202-9.
- World Health Organization. Changing history. The world health report 2004. Available from: http://www.who. int/whr/2004/en/report04_en.pdf [Last accessed on 2001 Dec 11].
- Walker N, Schwartländer B, Bryce J. Meeting international goals in child survival and HIV/AIDS. Lancet 2002;360:284-9.
- Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet 2003;361:2226-34.
- Ayieko P, Okiro EA, Edwards T, Nyamai R, English M. Variations in mortality in children admitted with pneumonia to Kenyan hospitals. PLoS One 2012;7:e47622.
- Macassa G, Ghilagaber G, Charsmar H, Walander A,Sundin Ö, Soares J. Geographic differentials in mortality of children in Mozambique: Their implications for achievement of Millennium Development Goal 4. J Health Popul Nutr 2012;30:331-45.
- Landes M, van Lettow M, Chan AK, Mayuni I, Schouten EJ, Bedell RA. Mortality and health outcomes of HIV-exposed and unexposed children in a PMTCT cohort in Malawi. PLoS One 2012;7:e47337.
- Patel V, Kumar AK, Paul VK, Rao KD, Reddy KS. Universal health care in India: The time is right. Lancet. 2011 Feb 5;377:448-9.
- Patwari AK. Risk factors for mortality in children hospitalized with pneumonia. Indian Pediatr 2012;49:869-70.
- Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child Health epidemiology research group. WHO estimates of the causes of death in children. Lancet 2005;365:1147-52.
- Miller MA, Sentz JT. Vaccine-preventable diseases. In: Jamison DT, Feachem RG, Makgoba MW, Bos ER, Baingana FK, Hofman KJ, et al., editors. Disease and Mortality in Sub-Saharan Africa. 2nd ed. Washington (DC): World Bank; 2006.
- Thörn LK, Minamisava R, Nouer SS, Ribeiro LH, Andrade AL. Pneumonia and poverty: A prospective population-based study among children in Brazil. BMC Infect Dis 2011;11:180.
- Montalvo W, Capitulo M. Is poverty the root cause of the epidemic of type 2 diabetes mellitus in children? MCN Am J Matern Child Nurs 2011;36:8-9.
- Lloyd SJ, Kovats RS, Chalabi Z. Climate change, crop yields, and undernutrition: Development of a model to quantify the impact of climate scenarios on child undernutrition. Environ Health Perspect 2011;119:1817-23.
- Indoor air pollution and health. Available from: http://www. who.int/mediacentre/factsheets/fs292/en/[Last accessed on 2011 Dec 11].
- Ramana GN, Sastry JG, Peters D. Health transition in India: Issues and challenges. Natl Med J India 2002;15(Suppl 1):37-42.
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006;367:1747-57.
- Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world: A growing challenge. N Engl J Med 2007;356:213-5.
- Lopez AD. The evolution of the Global Burden of Disease framework for disease, injury and risk factor quantification: Developing the evidence base for national, regional and global public health action. Global Health 2005;1:5.
- World Health Organization. The 10 leading causes of death by broad income group (2008). Available from: http://www. who.int/mediacentre/factsheets/fs310/en/index.html [Last accessed on 2011 Dec 11].
- Extensively drug-resistant tuberculosis (XDR-TB): Recommendations for prevention and control. Wkly Epidemiol Rec 2006;81:430-2.
- Minion J, Gallant V, Wolfe J, Jamieson F, Long R. Multidrug and extensively drug-resistant tuberculosis in Canada 1997-2008: Demographic and disease characteristics. PLoS One 2013;8:e53466.
- Michael JS, John TJ. Extensively drug-resistant tuberculosis in India: A review. Indian J Med Res 2012;136:599-604.
- Cegielski P, Nunn P, Kurbatova EV, Weyer K, Dalton TL, Wares DF, et al. Challenges and controversies in defining totally drug-resistant tuberculosis. Emerg Infect Dis 2012;18:e2.
- Arya SC, Agarwal N. Emergence of totally drug-resistant tuberculosis: Obscure and overlooked issues. Int J Tuberc Lung Dis 2012;16:852.
- Loewenberg S. India reports cases of totally drug-resistant tuberculosis. Lancet 2012;379:205.
- World Health Organisation. World Health Observatory. World Health Statistics Report 2011. Available from: http:// www.who.int/gho/publications/world_health_statistics/ EN_WHS2011_Full.pdf [Last accessed on 2011 Dec 11].
- Schuffenecker I, Iteman I, Michault A, Murri S, Frangeul L, Vaney MC, et al. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med 2006;3:e263.
- Weaver SC, Reisen WK. Present and future arboviral threats. Antiviral Res 2010;85:328-45.
- Friel S, Baker PI. Equity, food security and health equity in the Asia Pacific region. Asia Pac J Clin Nutr 2009;18:620-32.
- Popkin BM. Nutrition in transition: The changing global nutrition challenge. Asia Pac J Clin Nutr 2001;10(Suppl):S13-8.
- Tatem AJ, Hay SI, Rogers DJ. Global traffic and disease vector dispersal. Proc Natl Acad Sci USA 2006;103:6242-7.
- World Health Organization and World Trade Organization. WTO agreements and public health. A joint study by the WHO and the WTO Secretariat. Available from: http://www. wto.org/english/res_e/booksp_e/who_wto_e.pdf [Last accessed on 2011 Dec 11].
- Duggal R. Poverty and health: Criticality of public financing. Indian J Med Res 2007;126:309-17.
- World Health Organization. Protecting health from climate change. World Health Day 2008. Summary of issues paper. Available from: http://www.who.int/world-health-day/toolkit/2008_whd_issues_paper_summary_en.pdf [Last accessed on 2011 Dec 11].
- Chauhan LS. Public health in India: Issues and challenges. Indian J Public Health 2011;55:88-91.
- Adamson PC, Krupp K, Niranjankumar B, Freeman AH, Khan M, Madhivanan P. Are marginalized women being left behind? A population-based study of institutional deliveries in Karnataka, India. BMC Public Health 2012;12:30.
- Pascual Martínez F, Picado A, Roddy P, Palma P. Low castes have poor access to visceral leishmaniasis treatment in Bihar, India. Trop Med Int Health 2012;17:666-73.
- Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet 2011;377:505-15.
- Bajpai V, Saraya A. Healthcare financing: Approaches and trends in India. Natl Med J India 2010;23:231-5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.