RISK PROFILE AND OUTCOME MODIFIERS OF TRAUMATIC OCULAR INCIDENTS SEEN IN A TERTIARY HOSPITAL.
Received: 06-Jul-2022, Manuscript No. AMHSR-22-68638; Editor assigned: 08-Jul-2022, Pre QC No. AMHSR-22-68638(PQ); Reviewed: 22-Jul-2022 QC No. AMHSR-22-68638; Revised: 02-Nov-2022, Manuscript No. AMHSR-22-68638(R); Published: 09-Nov-2022
Citation: Nkemakonam EE, et al. Risk Profile and Outcome Modifiers of Traumatic Ocular Incidents Seen in a Tertiary Hospital. Ann Med Health Sci Res. 2022;12:1-5
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Injuries occasioning physical trauma is a global phenomenon with no foreseeable end. Increasing urbanization comes with increased human interaction and mobility leading to higher incidents of conflict and as well as accidents. An observational study involving consecutive new patients presenting with ocular injury was carried out in the outpatient and emergency department of our facility (Enugu State University Teaching Hospital) between October 1st 2019 and December 31st 2019.
Traumatic injuries in general and trauma to the globe in particular will represent a significant public health problem going forward. The present study, though limited by a small sample size, did not fail to show the ‘trauma cost’ of a hyperkinetic society and problems of poor law enforcement. Enforcement of work safety laws and regulation of activities of patent medicine dealers will reduce the incidence of ocular injuries and mitigate their eventual outcome in at risk individuals respectively. A larger study will aid a better understanding of these specific ocular trauma determinants and strengthen any advocacy efforts.
Keywords
Global phenomenon; Biomicroscope; Unilateral blindness; Traumatic ocular
Introduction
Injuries occasioning physical trauma is a global phenomenon with no foreseeable end. Increasing urbanization comes with increased human interaction and mobility leading to higher incidents of conflict and as well as accidents. Drug abuse and its associated violence has metastasized to our rural communities and can no longer be considered as a predominantly urban problem [1].
The Uber present internet with its trove of violent media has also been linked to destructive tendencies in young consumers of such media which in turn may lead to physical harm [2]. Trauma to the eye and its adnexa can be isolated or may accompany other injuries in patients with major trauma. Ocular trauma may well be visually inconsequential but can also result in permanent loss of sight and is indeed the commonest cause of unilateral blindness [3].
Even in the presence of one functional eye, individuals with unilateral blindness fall short in critical visual tasks. There is loss of stereopsis and contraction of their visual field which can result in reduced spatial orientation. Consequently, people with unilateral vision loss are more likely to trip and fall, be involved in road traffic accidents when they drive and might as well lose the fellow eye to trauma [4,5]. In all, their general physical and mental health will likely be impacted culminating in a noticeable reduction in their life expectancy [6,7]. The general and specific predispositions to this important but somewhat neglected cause of ocular morbidity and that will form the premise for the present study.
Materials and Methods
An observational study involving consecutive new patients presenting with ocular injury was carried out in the outpatient and emergency department of our facility (Enugu State University Teaching Hospital) between October 1st 2019 and December 31st 2019.
A pro-forma was formulated to record the relevant parameters for the study
The history of presenting complaint was analyzed and the following parameters were noted:
• Cause of injury
• Place of injury
• Duration of trauma before presentation.
• Nature of any treatment received prior to presentation and by who.
The findings on examination were entered as under:
• Presenting visual acuity (done with both literate and illiterate Snellen charts in verbal subjects and ageappropriate method in non-verbal children).
• Anterior segment findings using slit-lamp biomicroscope (Tagaki, Japan)
• Pupillary reactions using a pen-torch.
• Posterior segment evaluation with a slit-lamp and +780 Dioptre lens (VolkR aspheric Lens, USA).
The patient’s injury is then assigned a value in accordance with the Ocular Trauma Score (OTS) scoring system
• Lastly, the visual acuity six months post-presentation was taken and the candidate exited from the study.
• Only patients who gave informed consent were included in the study.
Data management
Retrieved data were cleaned and presented in prose, tables and figures using SPSSR version 23. Means of discreet data were calculated. Differences between means were evaluated by independent t-test. A value of p<0.05 was taken to be significant. Rules of ethical conduct in human research were adhered to as per Helsinki declaration.
Results
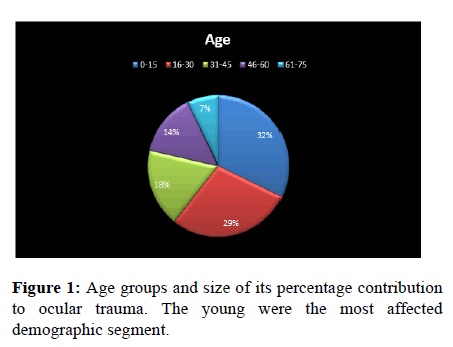
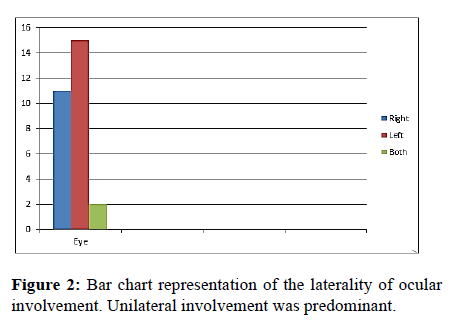
A total of five hundred and twenty eight (528) new patients were seen in our facility in the period under review. Ocular injury was the presenting complaint in twenty-eight (28) patients. This represented an ocular trauma incidence of 6%. Eighteen males representing 64% of the subjects were affected while ten females representing 36% of the cohorts were seen in (Tables 1-3). Average age of the subjects was 24.9 years with a range of 1 to 68 years. Their ages were further detailed down into four age strata as shown in Table 2. Ages of fifteen years and less were the most affected. Unilateral ocular involvement was the case in 92.9% of the subjects with left eye being affected more than the right eye. Only two subjects had bilateral ocular involvement in the study and both were females (Figures 1 and 2).
| Table 1: Demographic profile of the cohort. | |||
|---|---|---|---|
| Males | Females | Percentage | |
| Right Eye | 8 | 4 | 42.9 |
| Left Eye | 10 | 4 | 50 |
| Both Eyes | - | 2 | 7.1 |
| Affected segment Anterior | 15 | 10 | |
| + Posterior 0-15 | 3 | 0 | |
| Age in years 0-15 | 5 | 4 | 32.1 |
| 16-30 | 4 | 4 | 28.6 |
| 31-45 | 5 | - | 17.9 |
| 46-60 | 3 | 1 | 14.3 |
| 61-75 | 1 | 1 | 7.1 |
| Table 2: Ocular segment involvement and gender of the subjects. | ||||
|---|---|---|---|---|
| Diagnosis | Sex | Female | P-value | |
| Male | ||||
| Anterior | Frequency | 15 | 9 | 0.174 |
| Percent | 62.50% | 37.50% | ||
| Posterior | Frequency | 3 | 0 | |
| Percent | 100.00% | 0.00% | ||
| Not Applicable | Frequency | 0 | 0 | |
| Percent | 0.00% | 100.00% | ||
All the posterior segment injuries occurred in males.
| Table 3: Distribution of trauma with respect to anatomic location. | |||||||
|---|---|---|---|---|---|---|---|
| No | Mean trauma score | t-value | df (n-1) | Sig (2-tailed) | |||
| Domestic assault | 4 | 84.00 ± 18.54 | -0.713 | 6 | 0.503 | ||
| Domestic assault | 4 | 92.5 ± 15.00 | |||||
| Non-domestic accident | 15 | 73.60 ± 22.59 | -1.89 | 18 | 0.08 | ||
| Non-domestic assault. | 5 | 94.00 ± 13.42 | |||||
| All accidents | 18 | 76.11 ± 22.33 | -2.32 | 26 | 0.03* | ||
| All assaults | 10 | 94.00 ± 11.65 | |||||
| Ocular trauma from assault resulted in a statistically significantly poorer OTS (p=0.03) | |||||||
Seven days was the average duration between the occurrence of trauma and the time of presentation to our facility with a range of two hours to sixty days. Patients that sought for nonhospital treatment prior to presentation tended to present later than those who presented first to the hospital. This association was statistically significant. However, this did not result in a lower ocular trauma score (Tables 4 and 5).
| Table 4: Number of days prior to presentation in subjects that initially visited a patent medicine store versus those who did not. | ||||||
|---|---|---|---|---|---|---|
| N | Mean | Std. Deviation | Significance | t-value | Df (n-1) | |
| Pms | 20 | 15.5 | 16.06402 | 0.004 | 2.1 | 26 |
| NPMS | 8 | 3.375 | 2.6152 | |||
| Legend: Pms: Patent medicine store, NPMS: No-patent medicine store. | ||||||
| Table 5: OTS score of patients who patronized patent medicine store versus those who did not. | ||||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | Std. Deviation | Std. Error Mean | Sig | t | df | ||
| Pms | Pms | 20 | 80.86 | 20.512 | 4.476 | 0.807 | -0.352 | 26 |
| Npm | Npms | 8 | 84 | 20.29 | 7.669 | |||
| Legend: Pms: patent medicine store, NPms: No-Patent medicine store. A visit to a patent medicine store was associated with a poorer OTS. | ||||||||
Most traumas were accident related and tended to occur outside the home. There was no statistical difference between degree of injury and location. However, there was a statistically significant worse trauma outcome with respect to assault injuries.
Discussion
Ocular injury affects all ages and its epidemiologic characteristics reflect the way the world is evolving. In the present study, 6% of all our new consultations in the period under review were as a result of trauma to the globe. An earlier study in the same facility attributed only 1% of ophthalmic consultations to ocular injury [8-11]. Reported hospital prevalence of 6.2% and 5.6% in studies done in Ghana and Malawi respectively. It thus appears that the incidence of ocular injury is increasing. Males constituted 64.0% of our subjects (Table 1), a trend that has not changed with time. A combination of biological and socio-economic factors have been proposed asvehicles propelling the male gender down the path of self-trauma, including ocular related incidents [12-14]. Children and young adults (0-30 years) were equally dominant, accounting for 61.0% of our cohort. The restiveness that often accompanies youthfulness provides a fertile ground for trauma and the validation of this association is explicit in earlier studies [14-16]. About sixtyfour percent of the traumas were accidental in nature while the remaining 36% were due to assault (Table 3). Subjects with occupational ocular injury were not wearing any form of occupational safety device at time of the accident, highlighting a perennial indifference to use of such devices in the study area [17-20]. Why accident predominated in some studies and assault predominated in others is still debatable but jurisdictions with poor workplace safety practices or a preceding history of armed conflict could predict the ascendant mechanism for ocular injury. It is therefore not surprising that accidents predominated in our cohort since the law regulating occupational health and safety in Nigeria is merely symbolic, with little evidence of any form of enforcement. Delay of a few hours to 60 days with an average of 7 days prior to presentation characterized the health seeking behavior of the subjects. The factor associated with delay in presentation was a prior visit to a patent medicine store and this association was statistically significant (t=2.100, p=0.004). In addition, the patients who delayed their hospital presentation had poorer OTS but this was not statistically significant (t=-0.352, p=0.807). The reason(s) for the widespread patronage of patent medicine dealers may not be unconnected to lower cost of treatment and their accessibility. Unilateral ocular involvement was almost the rule except for two female subjects who had bilateral injury. Injuries were limited to the anterior segment in 85.7% of the subjects but associated posterior segment involvement was observed in 3 subjects representing 10.7% of the subjects. All the subjects with posterior segment involvement were males (Table 4). Seven subjects suffered unilateral blindness including the 3 subjects with additional posterior segment injuries. The hospital prevalence of unilateral blindness in our cohort was thus 25%. This was notably higher than findings from other studies.
Conclusion
Traumatic injuries in general and trauma to the globe in particular will represent a significant public health problem going forward. The present study, though limited by a small sample size, did not fail to show the ‘trauma cost’ of a hyperkinetic society and problems of poor law enforcement. Enforcement of work safety laws and regulation of activities of patent medicine dealers will reduce the incidence of ocular injuries and mitigate their eventual outcome in at risk individuals respectively. A larger study will aid a better understanding of these specific ocular trauma determinants and strengthen any advocacy effort.
Conflict of Interest
The authors wish to state that they do not have any conflict of interest. The study did not receive any external funding and all costs were borne by the authors.
Acknowledgement
The authors wish to thank all the medical and non-medical staff of department of ophthalmology, Enugu state university teaching hospital enugu especially the staff of medical records.
References
- Borders TF, Booth BM. Research on rural residence and access to drug abuse services: where are we and where do we go? J Rural Health. 2007;23:79-83. [Crossref][Googlescholar][Indexed]
- Huesmann LR. The impact of electronic media violence: scientific theory and research. J Adolesc Health. 2007;41:6-13. [Crossref][Googlescholar][Indexed]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; 390:1211-1259. [Crossref][Googlescholar][Indexed]
- Vu HTV, Keeffe JE, McCarty CA. AL impact of unilateral and bilateral vision loss on quality of life. Br J Ophthalmol. 2005;89:360-363. [Crossref][Googlescholar][Indexed]
- Fielder AR, Moseley MJ. Does stereopsis matter in humans? Eye (Lond). 1996;10:233-238. [Crossref][Googlescholar][Indexed]
- Chiang PP, Zheng Y, Wong TY, Lamoureux EL (2013) Vision impairment and major causes of vision loss impacts on vision-specific functioning independent of socioeconomic factors. Ophthalmology. 2013;120:415â??422. [Crossref][Googlescholar][Indexed]
- Foreman J, Xie J, Keel S. Prevalence and causes of unilateral vision impairment and unilateral blindness in australia: the national eye health survey. JAMA Ophthalmol. 2018;136:240-248. [Crossref][Googlescholar][Indexed]
- Pieramici DJ, Sternberg P Jr, Aaberg TM Sr. A system for classifying mechanical injuries of the eye (globe). the ocular trauma classification group. Am J Ophthalmol. 1997;123:820-831. [Crossref][Googlescholar][Indexed]
- Okoloagu NMN, Edeh AJ, Ekweremadu EN. Ocular Injuries in a Tertiary Hospital. JMSCR. 2020; 08:477-483.[Googlescholar][Indexed]
- Gyasi M, Amoaku W, Adjuik M. Epidemiology of hospitalized ocular injuries in the upper East region of ghana. Ghana Med J. 2007;41:171-175. [Googlescholar][Indexed]
- Zungu T, Mdala S, Manda C. Characteristics and visual outcome of ocular trauma patients at Queen Elizabeth Central Hospital in Malawi. PLoS ONE. 2021; 16:0246155. [Crossref][Googlescholar][Indexed]
- Okoye OI. Eye injury requiring hospitalisation in Enugu Nigeria: A one-year survey. Niger J Surg Res. 2006;8:34–37. [Crossref][Googlescholar]
- Fiebai B, Awoyesuku E. Ocular injuries among industrial welders in Port Harcourt, Nigeria. Clin Ophthalmol. 2011;5:1261-1263. [Crossref][Googlescholar][Indexed]
- Adamu MD, Muhammad N. Pattern of ocular trauma in Gusau, north west Nigeria. Niger J Ophthalmol 2017;25:11-3. [Crossref][Googlescholar][Indexed]
- Cillino S, Casuccio A, Di Pace F, Pillitterri F, Cillino G. A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol. 2008;8:1-6. [Crossref][Googlescholar][Indexed]
- Halperin SF, Bass JL, Mehta KA, Betts KD. Unintentional injuries among adolescents and young adults: a review and analysis. J Adolesc Health Care. 1983;4:275-281. [Crossref][Googlescholar][Indexed]
- Jiaquan Xu. WISQARS™ web-based Injury Statistics Query and Reporting System. Center for Disease Control and Prevention. United States. 2021.
- Titiyal GS, Prakash C, Gupta S, Joshi V. Pattern of ocular trauma in tertiary care hospital of Kumaon Region, Uttarakhand. J Indian Acad Forensic Med 2013;35:116-119.[Googlescholar]
- WHO. Adolescent and young adult health. World Health Organization. 2021. [Googlescholar]
- Raisanen AM, Kokko S, Pasanen K. Prevalence of adolescent physical activity-related injuries in sports, leisure time, and school: the National Physical Activity Behaviour Study for children and Adolescents. BMC Musculoskeletal Disord. 2018;19:1-8. [Crossref][Googlescholar][Indexed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.