Screening for Depressive Symptoms in Patients with Celiac Disease in Al-Qassim Region, Saudi Arabia
Citation: Khalid Lafi Alharbi. Screening for Depressive Symptoms in Patients with Celiac Disease in Al-Qassim Region, Saudi Arabia. Ann Med Health Sci Res. 2017; 7:9-12
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aim: The aim of study was to screen patients with celiac disease for symptoms of depression which can affect their adherence to gluten-free diet and quality of life. Methods: A retrospective study, the study was done in celiac disease awareness campaign in Al-Qassim region, Saudi Arabia. Results: 43% of celiac patients were suffering from symptoms of depression meeting the criteria according to PHQ-9 questionnaires. Conclusion: There is a high prevalence of depression symptoms among celiac patients.
Introduction
Celiac disease is an autoimmune disorder characterized by hypersensitivity to gluten which is a major protein found in different kind of food, such as wheat and grains. Celiac disease can affect different systems of the body. Celiac disease affects about 1% of total population. Females are usually two to three times affected compared to males. [1]. A cohort study in Saudi Arabia estimated that 2.2% of young healthy students are diagnosed with celiac diseases [2]. Mal-absorption, weight loss, chronic diarrhea, and steatorrhea are considered as the typical manifestations of celiac disease. However, there are atypical manifestations such as hair loss, osteoporosis, growth retardation and epilepsy. [3,4]. The only therapy for this disease, until now, is gluten free diet. But there is a poor compliance to this diet which reaches up to 30% of patients. [1].
The diagnosis of celiac disease is usually delayed in both primary health care providers and the secondary care. [5]. Early diagnosis and intervention will improve the quality of life and decrease the incidence of many complications which include osteoporosis, anemia and malignancy. [6,7].
In addition to the usual complaints of patients, psychological manifestations especially depression is consider as a big concern for patients. [8]. Depression or the behavioral changes may be the first symptoms to be noticed for celiac disease. [9].
A study estimated that celiac patients have a high risk to develop psychiatric symptoms like depression in adult and children. [10]. In addition, one-third of celiac disease patients have symptoms of depression. [11]. The low quality of life after diagnosis and malnutrition can be considered as risk factors for depression in celiac patients. [12]. Therefore, celiac disease patients with depression may need psychological support to improve the quality of life and adherence to the gluten-free diet. [13,14]. However, the actual cause is still unknown. [15].
Additional studies are necessary to clarify the prevalence of depression in patient with celiac diseases and strengthen this association
Objective
The aim of this study is to look for depressive symptoms in patients with celiac disease in Al-Qassim region, Saudi Arabia.
The Importance of this study
Depression may decrease the interest in life. So, celiac patients with depression may not follow the gluten free-diet adequately.
Methodology
Study design
It will be a cross sectional survey among diagnosed celiac patients.
Study population
The target population includes the patients diagnosed with celiac disease in Al-Qassim region.
Study setting
Campaign was made in a mall in Al-Qassim for celiac disease and from there we got an access to their social media (whatsapp and twitter accounts).
Inclusion criteria
All patients with a confirmed diagnosis of celiac disease regardless of their age and gender will be included in our study.
Exclusion criteria
Patients suffering from chronic comorbid diseases, cancers, normal bereavement or history of psychiatric disorders will be excluded and all of these will be excluded through the questionnaire.
Data collection
The data will be obtained by distributing electronic The Patient Health Questionnaire (PHQ-9) which is a validated tool used to screen, diagnose, and measure the severity of depression. PHQ-9 contains 10 questions of symptoms occurring within the past two weeks. The first nine questions are regarding anhdonia, depressed mood, sleep disturbance, decrease energy, appetite changes, guilt feeling, decrease concentration, moving/speaking speed changes, and suicidal thoughts which can be answered by not at all, several days, more than half of the days or nearly every day.
The tenth question is regarding daily functioning which can be answered by not difficult at all, somewhat difficult, very difficult, or extremely difficult.
Each answer is represented by a corresponding point, patients scoring 5-9 are of minimal symptoms, 10-14 are of minor depression, 15-19 are of major depression disorder moderate severity, and >20 are of the severe form of major depression disorder.
A validated Arabic form of PHQ-9 will be used. No permission is required to use it.
Study sample
The study sample was convenience sampling. So, no much role for randomization is there.
Study duration
This study done in June and July 2017.
Study analysis
All values will be analyzed using software Statistical Package of Social Science (SPSS 18 for windows evaluation version). In addition, χ2 tests will be used for categorical variables and the Mann-Whitney U test for continuous variables; P<0.05 will be considered statistically significant.
Data management and confidentiality
The questionnaire will state the goal of the study and that it is a voluntary participation. Patients will have the right to refuse to fill the questionnaire. Data will be collected anonymously without any personal identifiers. Primary Investigator’s contact information will be in the questionnaire in case they have any inquires. When data is collected, we will apply the data to the inclusion and exclusion criteria and then the data will be entered into an excel-format file.
Results
Total responders were 109, the samples were composed of 83.5% (n=91) females and 16.5% (n=18) males.
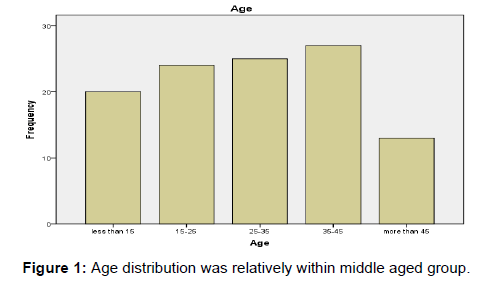
The age distribution was relatively within middle aged group [Figure 1], out of all responses analyzed, 47 (43.1%) patients met the criteria for the diagnosis of depression according to PHQ-9 questionnaires and the majority of them were diagnosed as major depression [Tables 1 and 2].
| Symptoms | Never | More Than One Day | More Than Half The Days | Nearly Everyday |
|---|---|---|---|---|
| Little interest or pleasure in doing things | 39 (35.8%) | 34 (31.2%) | 10 (9.2%) | 26 (23.9%) |
| Feeling down, depressed or hopeless | 35 (32.1%) | 34 (31.2%) | 23 (21.1%) | 17 (15.6%) |
| Trouble falling or staying asleep or sleeping too much | 28 (25.7%) | 24 (22%) | 31 (28.4%) | 26 (23.9%) |
| Feeling tired or having little energy | 19 (17.4%) | 27 (24.8%) | 22 (20.2%) | 41 (37.6%) |
| Poor appetite or overeating | 24 (22%) | 38 (34.9%) | 20 (18.3%) | 27 (24.8%) |
| Feeling bad about yourself or that you are a failure to yourself or family | 44 (40.4%) | 25 (22.9%) | 16 (14.7%) | 24 (22%) |
| Trouble concentrating on thing e.g. TV or reading a newspaper | 34 (31.2%) | 27 (24.8%) | 18 (16.5%) | 30 (27.5%) |
| Moving or speaking so slowly or the opposite moving around a lot or being flighty that people can notice | 55 (50.5%) | 22 (20.2%) | 16 (14.7%) | 16 (14.7%) |
| Thought that you would be better off dead or hurting yourself | 82 (75.2%) | 11 (10.1%) | 11 (10.1%) | 5 (4.6%) |
Table 1: Frequency of patients endorsing each of PHQ-9 symptoms in the last two weeks.
| Diagnosis according to PHQ-9 | No. |
|---|---|
| Major depression | 29 |
| Other depressive disorders | 18 |
| Total | 47 |
| Severity of Symptoms | No. |
| Minimal | 0 |
| Mild | 5 |
| Moderate | 15 |
| Moderately severe | 11 |
| Severe | 16 |
Table 2 : Diagnosis of depression according to PHQ-9 questionnaires and the majority of them were diagnosed as major depression.
Discussion
Five significant differences (p ≤ 0.05) were found in the sex category, 7 were found in the age category, and 8 were found in the marital status category, as respectively discussed in the following.
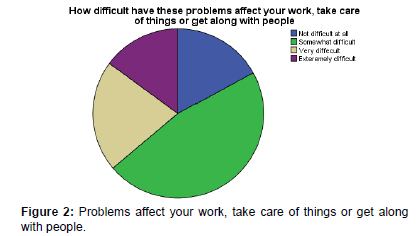
Our study found that the prevalence of depression in celiac patients around 43% which is much higher than the general population which is about 7%. [16]. Although there are few researches targeting psychiatric manifestation of celiac patients; a meta-analysis study found that the depression in adults with celiac disease is more severe and common than in healthy adults. [17]. The exact cause for depression in celiac disease is still not well understood but there is an evidence of alteration in brain blood flow in untreated celiac patients [18]. and strict adherence to gluten-free diet (GFD) can reduce the severity of depressive symptoms. [19]. As shown in Figure 2, celiac disease can have a negative impact on the quality of life represented by difficulties in relationship with friends, taking care of things at home or work and these findings concluded by a study conducted by Celiac Disease Center at Columbia University. [20]. Furthermore, a study showed Celiac disease negatively affected the quality of life in children. The Adherence to GFD is associated with more reduction in depression symptoms. [21]. The intensity of the psychological symptoms of celiac disease was found to be in a strong relationship with gastrointestinal symptoms and these symptoms dramatically will be improved once the patients started on GFD. [22].
The cost and the availability of gluten-free diet are important aspects of patients’ compliance. a study conducted in Saudi Arabia concluded that out of 113 samples, 100 (88.5%) of them reported that gluten-free products are not easily available in their area and 93% describe gluten-free products as very expensive. Another explanation is that patients may have social limitations because of the treatment. [23].
Limitations of the study
Samples were taken once at some point, multiple factors may influence the results, as patients may complain of stress or other systemic illnesses affecting their mood rather than celiac disease.
Conclusion
This study showed a high prevalence of depression symptoms among celiac patients which has an impact in adherence to gluten-free diet. Health care providers must be aware of psychiatric manifestations and provide well psychological support for the patients.
Acknowledgements
All authors disclose that there was no conflict of interest.
REFERENCES
- Green PHR, Cellier C. Celiac disease. New Eng J Med. 2007; 357:1731-1743.
- Aljebreen AM, Almadi MA, Alhammad A, Al-Faleh FZ. Sero-prevalence of celiac disease among healthy adolescents in Saudi Arabia. World J Gastroenterol WJG. 2013; 19:2374-2378.
- Hill ID, Dirks MH, Liptak GS. Guideline for the diagnosis and treatment of celiac disease in children: Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2005; 40: 1-19.
- Green PH, Jabri B. Coeliac disease. Lancet. 2003; 362: 383-391.
- Hin H, Bird G, Fisher P. Coeliac disease in primary care: A case finding study. BMJ. 1999; 318:164-167.
- Walters JR, Banks LM, Butcher GP, Fowler CR. Detection of low bone mineral density by dual energy X-ray absorptiometry in unsuspected sub-optimally treated coeliac disease. Gut. 1995; 37: 220-224.
- Ferguson A, Kingstone K. Coeliac disease and malignancies. Acta Paediatr Suppl. 1996; 412:78-81
- Addolorato G, Leggio L, D'Angelo C, Mirijello A, Ferrulli A, Cardone S, et al. Affective and psychiatric disorders in celiac disease. Dig Dis. 2008; 26:140-148.
- Potocki P, Hozyasz K. Psychiatric symptoms and coeliac disease. Psychiatriapolska. 2002; 36: 567-578.
- Cannings-John R, Butler CC, Prout H. A case control study of presentations in general practice before diagnosis of coeliac disease. Br J Gen Pract. 2007; 57: 636-642.
- Van Hees NJ, Van der Does W, Giltay EJ. Coeliac disease, diet adherence and depressive symptoms. J Psychosom Res. 2013; 74:155-160.
- Ludvigsson JF, Reutfors J, Osby U, Ekbom A, Montgomery SM. Celiac disease and risk of mood disorders - a general population based cohort study. J Affect Disord 2007; 99: 117-126.
- Holmes GK, Prior P, Lane MR, Pope D, Allan RN. Malignancy in coeliac disease-Effect of a gluten free diet. Gut. 1989; 30: 333-338.
- Holmes GK. Non-malignant complications of coeliac disease. Actapaediatrica (Oslo, Norway: 1992) Supplement. 1996; 412:68-75.
- Addolorato G, Di Giuda D, De Rossi G, Valenza V, Domenicali M, Caputo F, et al. Regional cerebral hypoperfusion in patients with celiac disease. The American journal of medicine. 2004; 116: 312-317. PubMed PMID: 14984816.
- Pynnonen PA, Isometsa ET, Aronen ET, Verkasalo MA, Savilahti E, Aalberg VA. Mental disorders in adolescents with celiac disease. Psychosomatics. 2004; 45(4):325-35.
- Smith DF, Gerdes LU. Meta-analysis on anxiety and depression in adult celiac disease. Acta Psychiatrica Scandinavica. 2012; 125:189-193.
- Addolorato G, Di-Giuda D, De-Rossi G, Valenza V, Domenicali M, Caputo F, et al. Regional cerebral hypoperfusion in patients with celiac disease. Am J Med. 2004; 116:312-317.
- Van Hees NJ, Van der Does W, Giltay EJ. Coeliac disease, diet adherence and depressive symptoms. Journal of Psychosomatic Research. 2013; 74:155-160.
- Lee A, Newman JM. Celiac diet: Its impact on quality of life. Journal of the American Dietetic Association. 2003; 103:1533-1535.
- Simsek S, Baysoy G, Gencoglan S, Uluca U. Effects of gluten-free diet on quality of life and depression in children with celiac disease. J Pediatric Gastroenterol Nutr. 2015; 61: 303-306.
- Martinez Cerezo FJ, Castillejo G, Guillen N, Morente V, Simo JM, Tena FJ, et al. Psychological alterations in patients with adult celiac disease. Gastroenterologia y hepatologia. 2014; 37: 240-245.
- Sarkhy A, El-Mouzan MI, Saeed E, Alanazi A, Alghamdi S, Anil S, et al. Socioeconomic impacts of gluten-free diet among Saudi children with celiac disease. Pediatric Gastroenterol Hepatol Nutr. 2016; 19:162-167.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.