Study of the Effects of Combined Therapy with Sodium Valproate, Peg-interferon and Corticosteroid on Proviral Load of HTLV-1 and the Expression of Rel-A, Creb and IL-1 Genes in Patients with HTLV-1 associated Myelopathy/Tropical Spastic Paraparesis
2 Molecular Research Center, Sabzevar University of Medical Sciences, Sabzevar, Iran, Email: atabati123@gmail.com
3 Department of Immunology, Mashhad University of Medical Sciences, Mashhad, Iran
4 Department of Neurology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
5 Inflammation and Inflammatory Diseases Research Center, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran, Email: Rezaeer@mums.ac.ir
6 Student Research Committee, Department of Anatomy, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Email: Amirrezaraoofi@yahoo.com
Amir Raoofi, Student Research Committee, Department of Anatomy, Iran, Tel: 00989368698934, Email: Amirrezaraoofi@yahoo.com
Citation: Atabati H, et al. Study of the Effects of Combined Therapy with Sodium Valproate, Peg-interferon and Corticosteroid on Proviral Load of HTLV-1 and the Expression of Rel-A, Creb and IL-1 Genes in Patients with HTLV-1 associated Myelopathy/Tropical Spastic Paraparesis. Ann Med Health Sci Res. 2018;8:340-345
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background and Objective: Human T-Cell Lymphotropic Virus Type I (HTLV-I) is endemic in northeast of Iran. Although chronic inflammation of spinal cord seems to play a major role in the disease pathogenesis, immunomodulatory treatments have not shown significant improvement in disease symptoms. This study was conducted to evaluate the effect of sodium valproate in combination with Peg-Interferon (Peg-IFN) and prednizolone on proviral load and inflammatory factors of patients with HTLV-I associated myelopathy/tropical spastic paraparesis (HAM/TSP). Materials and Methods: In this pilot clinical trial, 10 HTLV-1 Associated Myelopathy/Tropical Spastic Paraparesis (HAM/TSP) patients, referred to HTLV- 1 clinic of Qaem Hospital of Mashhad, Iran in 2012, were treated with sodium valproate, Peg-IFN and prednizolone for 6 months. Peripheral blood mononuclear cells (PBMCs) were isolated using Ficoll Hypaque and the RNA was extracted from PBMCs. Complementary DNA was synthesized using TaqMan Gold RTPCR Kit. A real-time PCR TaqMan method was designed and optimized for evaluation of Rel-A, Creb and IL-1 genes expression. Results: The analysis in this study indicated that proviral load and IL-1 mRNA expression in patients were significantly lower after treatment. Despite this decline, Creb and IL-1 mRNA expression was not significant. Conclusion: The combination of sodium valproate, Peg-IFN and prednizolone seems an effective treatment for proviral load and relatively efficient for damaging inflammatory factors of HAM/TSP; however, further studies with sufficient sample sizes are necessary.
Keywords
Sodium valproate; Peg-Interferon; Prednisolone; HAM/TSP
Introduction
The first human retrovirus discovered was Human T-cell lymphotropic virus type I (HTLV-I), and the studies have revealed that 10-20 million people are infected with HTLV-I all over the world. [1] HTLV-I is endemic in certain regions of the planet such as south of Japan, Sub- Saharan Africa, Caribbean countries and Brazil. It was concluded in 1992 that north of Khorasan (a province at north-east of Iran) could be an endemic area for HTLV-I infection. [2] HTLV-I can be transmitted through three main routes: 1-mother-to-child transmission by breastfeeding is one the main modes of HTLV-I transmission. 2-sexual contact is another way for HTLV-I transmission. 3-the third mode of HTLV-I transmission is blood transfusion. A factor playing the role of infectious agent is the proviral DNA in donors’ blood lymphocytes. [3] It has been dem-onstrated that HTLV-1 is the etiological agent of adult T cell leukemia (ATL) and a progressive neurological disease called HTLV-I associated myelopathy/tropical spastic paraparesis (HAM/TSP). This neurological disease reveals itself as a progressive and slow spastic paraparesis without remission. The vast majority of individuals infected by HTLV-1 are clinically asymptomatic; less than 5% of infected individuals develop HAM/TSP. [4]
The fundamental mechanisms of the HAM/TSP etiopathogenesis in people infected by HTLV-I are not fully understood. Both viral factors and host genetic background may affect the outcome of HAM/TSP in HTLV-I infection. HTLV-I virus type in Mashhad, Iran is the same as that found in Japan. However, there is no clear evidence proving the association between HTLV-I variants and vulnerability to HAM/TSP. While an amino acid substitution in the Tax protein (essential for viral transcription) has been suggested to increase the risk of developing HAM/TSP after HTLV-I infection, the Tax gene mutation is associated with to HTLV-I subtype rather than risk of HAM/TSP. [5]
There is not any standard therapy for HAM/TSP. Several studies have suggested the application of anti-inflammatory drugs, immune modulator drugs and others. [6] Treatment options are generally divided into symptomatic and etiologic groups. Antispastic and anticholinergic agents, analgesics, physiotherapy, and the management of emotional and social problems fall into symptomatic management group. Etiological treatments comprise corticosteroids, cytotoxic agents, interferon alpha, plasma exchange (PE), and other immunomodulatory agents like Danazol, Erythromycin, Phosphomycin, Sulphasalazine, and Pentoxyphillin. Because of the more rapid progress of the disease during the first year, early treatment during this period provides the chance of improvement. [7]
This study was conducted to evaluate the effect of sodium valproate in combination with Peg- IFN and prednizolone on proviral load and inflammation factors in patients with HAM/TSP.
Materials and Methods
Study design
The cross-sectional study Via primary investigation among 68 new case HAM/TSP patients, 10 patients who referred to neurology clinic of Ghaem Hospital of Mashhad were selected with related inclusion (being a new case, demonstration of virus occurrence in CSF, and lack of any contradiction for Peg-IFN administration such as cardiac failure, renal failure, hepatic disease, thrombocytopenia, anemia, leucopenia, pregnancy, breast-feeding, etc.) and exclusion (occurrence of further causes for paraparesis other than HTLV-1, presence of active hepatic disease, and the risk of renal failure) criteria. The disease was diagnosed in these persons by a neurologist according to WHO criteria. After taking consent and filling clinical and personal information checklists, 10 cc of venous blood was taken and transported to Immunology Laboratory of Medicine Faculty of Mashhad University of Medical Sciences during less than six hours. To establish HTLV-1 infection, ELISA was conducted for all blood samples and if the result was positive, confirmed by PCR. Then, cerebrospinal MRI, vasculitis, and other tests were done to reject other causes of spastic paraparesis. To prove the presence of virus, the patients were subjected to cerebrospinal fluid puncture and included in the study according to Possioni et al. algorithm with a diagnosis of HAM/TSP. [8,9]
Treatment protocol
The patients were weekly visited by neurology resident in the clinic and injected with Peg-IFN (Pegasis, Roche, Germany with a dose of 180 micrograms) up to 25 weeks and 10-20 mg/Kg/day of sodium valproate (orlept) and 5 mg/day of prednizolone were also prescribed for the patients during this period. During this time, blood count formula and hepatic functionality tests were exploited weekly in the first month, once two weeks in the second and third months, and monthly in the case of being normal, to examine potential complications. Thyroid functionality tests were performed at months 0, 3, and 6. [10]
Laboratory methods
At first, the peripheral blood lymphocytes (PBMCs) were isolated from the whole blood by Ficoll gradient centrifugation using ®Lympholyte-H solution. Tri-pure solution (tripure isolation kit, Roche) was used to extract the RNA. The integrity of RNA was examined by agarose gel electrophoresis. To detect the RNA, first it was converted into single stranded complementary DNA (cDNA) by the aid of reverse transcriptase (RT) and then, amplified by PCR. Random hexamer was exploited to synthesize cDNA and then, this cDNA was applied for real time PCR. H minus First Strand cDNA Synthesis KitRevertAidTM kit (Frementas) was used to synthesize cDNA. PCR was utilized to confirm correct cDNA synthesis and the result was visualized on agarose gel. [11]
Gene sequencing
GeneBank section of NCBI (http://www.ncbi.nlm.nih.gov) was the source used for providing the sequences of Rel-A, Creb, and IL-1 genes. Primer sequences were determined according to Table 1. 5 microliter of forward primer and 5 microliter of reverse primer related to Rel-A and Creb genes and 30 microliter of PCR product were sent to Bioneer, South Korea by Takapouzist Corporation.
| Targeted gene | Sequence (5’ to 3’) | Purpose | Product size (Base pairs) |
|---|---|---|---|
| Rel-A | ACCCCTTCCAAGTTCCTATAGAAGAG | Forward | 145 |
| CGATTGTCAAAGATGGGATGAGAAAG | Reverse | ||
| ACTACGACCTGAATGCTGTGCGGCTCT | probe | ||
| Creb | ACTCCAAAAGTAAAGTCCCGTTAC | Forward | 90 |
| TCCAAAGAAACAGGAAGCAGATTG | Reverse | ||
| TTCTCCTCCCACCGCCCTTGTCCC | probe | ||
| IL-1 | CTGGACCTCTGCCCTCTG | Forward | 78 |
| CAGCATCTTCCTCAGCTTGTC | Reverse | ||
| ACGAATCTCCGACCACCACTACAGCAA | probe |
Table 1: Primer and probe sequences used in quantitative real-time polymerase chain reaction.
Performing real time PCR by TaqMan method
Real time PCR by TaqMan method (Maser MixTaq Man, Japan) was utilized to measure expression level of Rel-A, Creb, and IL-1 genes in the samples before and after treatment. To attain the samples with the maximum expression level of Rel-A, Creb, and IL-1 genes, the reaction mixture was prepared for each gene as follows: 9 microliter of reaction mixture and 1 microliter of cDNA sample were added into each 0.1-mililiter micro-tube special for Corbett device. After adjusting the thermal conditions for the reaction, the micro-tubes were place in the Corbett device. All real time PCR experiments were conducted using Rotor Gene Q (Qiagen, Germany). Thermal cycles in TaqMan method were of two-step type. The PCR program was as follows: a) the first cycle: 95°C for 10 minutes; b) 40 to 45 cycles: 95°C for 15 seconds, 60°C for 60 seconds, and reading the green fluorescence at 60°C.
Comparative analysis of gene expression
Comparative analysis of gene expression was carried out by the aid of Standard Curve Method. In this method, the values of unknown sample were resulted from plotting standard curves for the desired gene and normalized using the resultant values for the desired genes. Therefore, the acceptable standard curve was depicted for target genes. After acquiring the sample concentrations, data for the desired gene was normalized using the values for the desired genes. Then the values for the desired genes were compared for the desired genes among test groups.
Measurement method for proviral load level
Since the viral genome is inserted into the host genome, proviral load measurement requires DNA extraction from patient’s lymphocytes. In this study, the extraction kit Genetbio PrimePrep Genomic DNA Isolation Kit from Blood Cat. No. K-2000 was utilized. Novin Gene kit was exploited to assess proviral load level. In the kit, the occurrence frequency of TAX and LTR regions from proviral genome is divided into the albumin gene frequency against the standard curve with five defined concentrations that are commercially provided and have fixed copy numbers. Both copies of albumin gene are considered equal to one cell. The number of copies resulted are reported in the 104PBMC value. Two extraction-based calculation methods can be used in this kit: in the first method, with isolation of PBMCs from peripheral blood by ficoll; and in the second method, by the extraction of DNA from whole blood in which CBC must be done for the patient and HTLV-I titer× 100/Cell titer× (% Lymphocyte+Monocyte) formula must be applied for calculating viral load. In the present investigation, the first method was used for determination of viral load.
Result analysis
Radiation channel of green color was related to HTLV-1 and Radiation channel of red color was related to albumin. Because the last Ct standard is about 40, all samples uprising below this Ct were reported as positive. [12]
Statistical calculations
All data were presented as mean value ± standard deviation. Alteration percent in values of Rel-A, Creb, and IL-1 genes was calculated for patients’ samples before and after treatment. Statistical analysis was conducted using SPSS 19 software. Initially Colmogrov-Smirnov statistical test was utilized to determine whether the data were parametric or non-parametric. Wilcoxon tests were used to analyze non-parametric data and for analyzing parametric data, t-test method was exploited.
Results
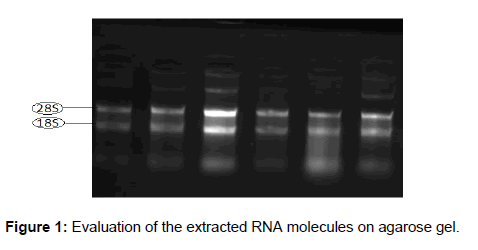
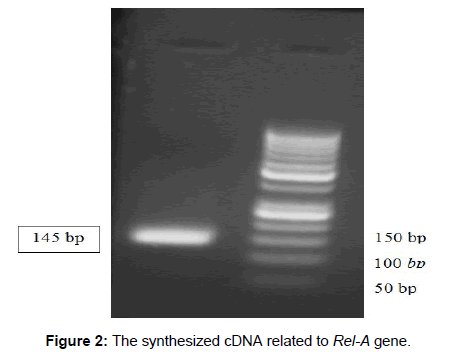
Evaluation of the extracted RNA on Agarose gel and quality examination for cDNA
Figure 1 demonstrates an example of evaluation of the extracted RNA molecules on agarose gel that was done for all samples. PCR reaction was conducted to examine the quality of the synthesized cDNA molecules and an example of this is represented in Figure 2.
Age & gender of the studied patients
Age distribution of 10 studied HAM/TSP patients shows that 4 males and 6 females had the average age of 42, standard deviation was 15.9, the maximum was 62 and the minimum age was 40 [Table 2].
| Patient number |
Sex | Age(years) | Rel-A expression (Copy Rel-A/β2 m × 1000) |
Creb expression (Copy Creb /β2 m ×1000) |
IL-1 expression (Copy IL-1/β2 m × 1000) |
HTLV-1 proviral load | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | |||
| 1 | F | 32 | 71.1 | 9.8 | 536.4 | 52.1 | 186 | 0.5 | 547 | 254 |
| 2 | M | 57 | 6.2 | 4 | 28 | 1.1 | 0.1 | 0.7 | 293 | 925 |
| 3 | F | 27 | 98 | 21.5 | 473.6 | 47.4 | 0.2 | 130 | 520 | 62 |
| 4 | F | 27 | 1276 | 7.1 | 1.2 | 27 | 664 | 4.5 | 2166 | 1822 |
| 5 | M | 20 | 1.9 | 12.8 | 1.3 | 17.5 | 0.03 | 0.6 | 1893 | 969 |
| 6 | F | 31 | 12.9 | 2.3 | 1.7 | 13.2 | 0.006 | 0.38 | 3802 | 1295 |
| 7 | M | 62 | 8.7 | 3 | 4.4 | 23.6 | 110 | 18.4 | 1520 | 732 |
| 8 | M | 54 | 1.8 | 67.3 | 4 | 76.1 | 398 | 0.8 | 769 | 378 |
| 9 | F | 52 | 8 | 12.5 | 1.4 | 0.9 | 1.7 | 0.6 | 638 | 429 |
| 10 | F | 58 | 1.9 | 6 | 21.1 | 1.1 | 0.1 | 0.57 | 751 | 284 |
Table 2: Summarizes real time PCR results for Rel-A, Creb, IL-1 and HTLV-1 proviral load in samples before and after treatment.
Rel-A gene expression and statistical analysis of its real time PCR results before and after treatment
Table 2 summarizes real time PCR results for Rel-A gene in samples before and after treatment and these data have been normalized using β2-microglobolin gene. The expression of Rel-A gene before treatment with mean value of 148.6, standard deviation of 19.3, minimum expression level of 1.8 and maximum expression value of 1276 was compared to the expression of this gene after treatment with mean value of 14.63, standard deviation of 397.5, minimum expression level of 2.3 and maximum expression value of 67.3. Although the mean value for the expression of this gene has decreased after treatment, this difference was not statistically meaningful because the data were parametric (p-value=0.31).
Creb gene expression and statistical analysis of its real time PCR results before and after treatment
Table 2 summarizes real time PCR results for Creb gene in samples before and after treatment and these data have been normalized using β2-microglobolin gene. The expression of Creb gene before treatment with mean value of 107.3, standard deviation of 210.3, minimum expression level of 1.2 and maximum expression value of 536.4 was compared to the expression of this gene after treatment with mean value of 26, standard deviation of 25.3, minimum expression level of 0.9 and maximum expression value of 76.1. Although the mean value for the expression of this gene has decreased after treatment, this difference was not statistically meaningful because the data were parametric and paired T-test was exploited (p-value=0.22).
IL-1 gene expression and statistical analysis of its real time PCR results before and after treatment
Table 2 summarizes real time PCR results for IL-1 gene in samples before and after treatment and these data have been normalized using β2-microglobolin gene. The expression of IL-1 gene before treatment with mean value of 136, standard deviation of 226.3, minimum expression level of 0.006 and maximum expression value of 664 was compared to the expression of this gene after treatment with mean value of 15.7, standard deviation of 40.5, minimum expression level of 0.38 and maximum expression value of 130. Although the mean value for the expression of this gene has decreased after treatment; this difference was not statistically meaningful at assurance level of 95% (p-value=0.1), but because of being at assurance level of 90%, it should be investigated in a larger population.
HTLV-1 viral load
The patients’ viral load before treatment has the BMCs Copies/mean value of 1289.9, standard deviation of 546.7, the minimum value of 62, abd the maximum load of 1822. The normalization of results was carried out via Colmogrov-Smirnov statistical test and paired T-test was exploited because the data were parametric. Statistical analysis confirms that the difference between viral load before and after the treatment is meaningful (p=0.02). In comparison of viral load before and after treatment, the correlation between them was determined to be up to 0.71 [Table 2].
Discussion
HAM/TSP is a progressing chronic neurological disease causing axonal damage in the brain and spinal cord. Most of cells participating in immune responses are CD4+ T lymphocytes, CTLs and monocytes able to pass through the blood-brain barrier and to reach the cerebral parenchyma. Infiltrated cells cause the beginning of immune response after migration to the central nervous system and its outcomes affects the neurons and causes axonal damage and gradual demyelination. Axonal and neural destruction is associated with neurological disorders in HAM/TSP patients. The exact mechanisms of these destructive responses are unclear, but it is assumed that mechanisms such as inflammatory-environment-caused lateral destruction and the mechanism of gradual demyelination has a role in these disorders. However, the exact pathophysiology is not known and therefore, the effective treatment is controversial. [1] Valproate (VPA) is the center of attention nowadays. This compound causes the intense histone acetylation and as a result, activation of transcription from five promoters of HTLV-1 viral genome. [13] Several reports have pointed the effect of valproate on the immune system. Many studies demonstrate serum immunoglobulin depletion by valproate, [14,15] while some studies have shown that valproate inhibits the production of TNF-α and IL-6 in LPS-stimulated THP-1 cells (in-vitro) and causes the repression of NF-κB migration to the nucleus. This repression of NF-κB migration to the nucleusis not dependent on IκB-α maintenance. Decreased NF-κB expression in glioma cells has also been observed. [16]
Monocytes play an important role in inflammatory reactions through the production of pro-inflammatory cytokines. The glial cells pay a similar inflammatory role in the central nervous system. Noting that valproate blocks the activation of NF-κB in both blood monocytes and neural glial cells, decreased expression of this protein in monocytes is extensible to glial cells. With the inhibitory effect of valproate on NF-κB, we should naturally expect the decreased expression of proinflammatory cytokines, especially IL-1, TNF-α, and IL-6. As the average expression of Rel-A gene decreased in the present study (from 148.6 to 14.6), the average expression of IL-1 gene also has decreased after treatment (from 136 to 15.7). Other investigations have proved the effect of valproate on inflammation and the cells involved in inflammation.
The effect of valproate as a histone deactylase-blocking drug in rats buffering from an MS-like disease called EAE (some kind of neural inflammatory disease similar to HAM/TSP) causes the depletion of Th1 and Th2 cells, which play an important role in inflammation. [17]
Valproate administration has been reported safe in patients suffering from HAM/TSP. [18] It has also been determined that this drug causes increased expression of viral genes because of its histone deactylaseblocking properties and as a result, makes the viruses recognizable for the host immune system. Through stimulation of CTLs, the host immune system makes the HTLV-1-infected CD4+ T cells destroy. This process leads to the decreased viral load. [13] In another work, expression of Tax protein in cultivated infectious cells altered from 1.5 in the absence of valproate to 2.3 in its presence. While the expression of HBZ protein decreased. [18] HBZ protein is a transcription suppressor of viral genes that acts via Tax. This suppressive property takes place by intervening in the activity of Creb transcription factor and it’s joining protein. [19] Since the mean expression of Creb genes has decreased after treatment in this study, this decreased expression can be justified by depletion of expression of HBZ genes caused by inhibitory effects of valproate. The primary examinations showed evidence of a relationship between valproate treatment and HTLV-1 viral load and an idea that decreased viral load makes the clinical symptoms adjusted, was the motivation for several investigations in this realm. [19] Valproate treatment in HAM/TSP patients increases the HTLV-1 viral load in peripheral during the initial weeks. [13] In addition, azidothymidine (AZT) treatment restrains virus production and combinatory treatment of AZT along with valproate rather than valproate alone, strongly decreases the viral load in STLV-1 (simian model of HTLV-1). [20]
Accordingly, viral load depletion is meaningfully observed in HAM/ TSP patients taking this drug. In these studies, muscular spasticity has been decreased following viral load decline. [13] Although the viral load decline is expected in treatment with valproate in HAM/TSP patients, in some cases this depletion has not been reported; for instance, in an investigation by Olindo et al. in 2011, valproate treatment in 19 HAM/TSP patients resoled in non-significant effect on viral load and lethality of CD8+ cells and only the walking time had been increased significantly in 3 patients. Because of 24-month treatment with valproate, their survey proved the safety of valproate in these patients. [21]
In accordance with other studies based on depletion of viral load, in this study, this case showed a significant decrease after combinatory treatment (p=0.02). Since these is not yet clear that why some HTLV-1 carriers suffer from HAM/TSP, it seems that the immunological factors related with this virus play the major role in the disease pathology. Therefore, treatment with immunomodulatory drugs like interferon-α can cause alteration in the course of disease. It is well accepted that interferon α (IFN-α), is a cytokine with strong antiviral, antimultiplication, and immunomodulatory effects. Interferon α is the main responsive cytokine for amplifying CD8+cell response and resistance against viral infections. Furthermore, it is a Th1 cell regulator with an important role in development of immune responses. [22]
Several studies have focused on examination of the effect of interferon α on HAM/TSP patients and its effects on disease symptoms and viral load. Multiple investigations have confirmed the safety and effectiveness of interferon α. [23-25] Depletion of Th1 cells with administration of interferon α has been observed in a number of studies conducted in HAM/TSP patients. A four-week administration of interferon α in 9 HAM/TSP have decreased CCR5+ and Th1 cells significantly in patients’ cerebrospinal fluid and blood. Reduction in IFN-γ+ cells to IL-4+was also observed in these patients. Therefore, depletion of Th1 cells (pathological agent of this disease) was observed. [26] Nakagava and coworkers prescribed different drugs for examining clinical symptoms in 200 patients suffering from HAM/TS; among 32 patients who had muscularly injected interferon α, 20 patients showed weak to high alterations on kinetic symptoms. [27]
In the present investigation that takes the benefit of interferon α combinatory treatment, the viral load shows significant depletion after the treatment (p=0.02). One reason that interferon α is known as an immunomodulator drug, is its effect on the production of other cytokines. Accordingly, an investigation eas conducted in the field of effects of type one interferon on the production of IL-1. This study determined that type one interferons strongly suppress IL-1 production. This suppression is exerted via blocking the activity of inflammasomes NLRP1 and NLRP3, which play a role in pro-IL-β maturation pathway and stimulate STAT3 via promoting IL-10 production and depletion of Pro-IL-1α and Pro-IL-1β. [28] Also the decreased expression of IL-1 genes in this study may be caused by blocking inflammasomes.
Prednizolone is one of immune-suppressor drugs with several applications in multiple sclerosis (MS) and other autoimmune diseases and some studies have been conducted in the field of administering this drug for HAM/TSP patients. In an investigation on 23 patients suffering from HAM/TSP with intra-muscular injection of methylprednizolone,the limited effect of drug was observed in patients; so that one of the studied patients who had the symptoms onset only 5 months ago, showed some extent of improvement in clinical symptoms. At the end of that study, it was suggested that methylprednizolone was proper for administrating in patients who had already onset the clinical symptoms. [29] Prednizolone administration as an immonomodulator was also investigated in HAM/TSP patients and clinical symptoms such as musculat tension and paraesthesia returned to the normal state. This drug generally relives the disease symptoms. [30]
Prednizolone effect has also been demonstrated on the expression of immune system genes. Intravenous administration of methylprednizolone in patients suffering from multiple sclerosis (MS) is similar to HAM/TSP in terms of inflammation emerged in the central system and decreased expression of immune system has been observed. [31] Methylprednizolone decreases the plasma levels of cytokines IL-6, TNF-α, and IL-1β. [32] This depletion of inflammatory cytokines takes place because of blockage of NF-κB activation by triggering increased κB-α synthesis. [33,34] The effect of methylprednizolone on depleted levels of activated Rel-A protein (a subset of transcription factor NF- κB) shows decreased level of pro-activating inflammatory factor. [35]
Conclusion
I this research combination of sodium valproate, Peg-IFN and prednizolone seems an effective treatment for proviral load and relatively efficient for damaging inflammatory factors of HAM/TSP.
Conflict of Interest
The authors disclose that they have no conflicts of interest.
REFERENCES
- Vakili R, Sabet F, Aahmadi S, Boostani R, Rafatpanah H, Shamsian A, et al. AR. Human T-lymphotropic virus type I (HTLV-I) proviral load and clinical features in Iranian HAM/TSP Patients. Iran J Basic Med Sci. 2013;16:268-272.
- Boostani R, Saber HR, Etemadi MM. Effects of danazol on clinical improvement of patients with human T-cell lymphotropic virus type I associated myelopathy/tropical spastic paraparesis (HAM/TSP): A placebo-controlled clinical trial. Iran J Basic Med Sci. 2013;16:213-216.
- Rafatpanah H, Farid R, Golanbar G, Azad FJ. HTLV-I Infection: Virus structure, immune response to the virus and genetic association studies in HTLV-I-infected individuals. Iran J Allergy Asthma Immunol. 2006;5:153-166.
- Taghaddosi M, Rezaee SAR, Rafatpanah H, Rajaei T, Farid Hosseini R, Valizadeh N. Association between HLA class I alleles and proviral load in HTLV-I associated myelopathy/tropical spastic paraperesis (HAM/TSP) patients in Iranian population. Iran J Basic Med Sci. 2013;16:264-267.
- Shirdel A, Azarpazhooh MR, Sahebari M, Ghanbari M, Mirfeizi Z, Hutchinson I, et al. Association of IL-10 gene polymorphisms and human T lymphotropic virus type I-associated myelopathy/tropical spastic paraparesis in North-East Iran (Mashhad). Iran J Basic Med Sci. 2013;16:258-263.
- Pillat MM, Bauer ME, Penalva de Oliveira AC, Ulrich H, Casseb J. HTLV-1-Associated myelopathy/tropical spastic paraparesis (HAM/TSP): Still an obscure disease. Cent Nerv Syst Agents Med Chem. 2011;11:1-7.
- Shoeibi A, Etemadi MM, Moghaddam AA, Amini M, Boostani R. “HTLV-I Infection” Twenty-year research in neurology department of Mashhad University of Medical Sciences. Iran J Basic Med Sci. 2013;16:202-207.
- Rafatpanah H, Hedayati-Moghaddam MR, Fathimoghadam F, Bidkhori HR, Shamsian SK, Ahmadi S, et al. High prevalence of HTLV-1 infection in Mashhad, Northeast Iran: a population-based seroepidemiology survey. J Clin Virol. 2011;52:172-176.
- Matsuzaki T, Nakagawa M, Nagai M, Usuku K, Higuchi I, Arimura K, et al. HTLV-I proviral load correlates with progression of motor disability in HAM/TSP: Analysis of 239 HAM/TSP patients including 64 patients followed up for 10 years. J Neurovirol. 2001;7:228-234.
- Boostani R, Vakili R, Hosseiny SS, Shoeibi A, Fazeli B, Etemadi MM, et al. Triple therapy with prednisolone, pegylated interferon and sodium valproate improves clinical outcome and reduces human T-cell leukemia virus type 1 (HTLV-1) proviral load, tax and HBZ mRNA expression in patients with HTLV-1-associated myelopathy/tropical spastic paraparesis. Neurotherapeutics. 2015;12:887-895.
- Rafatpanah H, Rezaee A, Etemadi MM, Hosseini RF, Khorram B, Afsahr L, et al. The impact of interferon-alpha treatment on clinical and immunovirological aspects of HTLV-1-associated myelopathy in northeast of Iran. J Neuroimmunol. 2012;250:87-93.
- Saifi B, Rezaee SA, Tajik N, Ahmadpour ME, Ashrafi M, Vakili R, et al. Th17 cells and related cytokines in unexplained recurrent spontaneous miscarriage at the implantation window. Reprod Biomed Online. 2014;29:481-489.
- Lezin A, Gillet N, Olindo S, Signate A, Grandvaux N, Verlaeten O, et al. Histone deacetylase–mediated transcriptional activation reduces proviral loads in HTLV-1–associated myelopathy/tropical spastic paraparesis patients. Blood: 2007;110:3722-3728.
- Fujiwara K, Yoshida A, Ochi M, Yoshioka H. Serum immunoglobulin levels in children receiving valproic acid Brain Dev. 1983;5:193.
- Joubert P, Aucamp A, Potgieter G, Verster F. Epilepsy and IgA deficiency--The effect of sodium valproate. S Afr Med J. 1977;52:642-644.
- Castelo-Branco G, Stridh P, Guerreiro-Cacais AO, Adzemovic MZ, Falcao AM, Marta M, et al. Acute treatment with valproic acid and l-thyroxine ameliorates clinical signs of experimental autoimmune encephalomyelitis and prevents brain pathology in DA rats. Neurobiol Dis. 2014;7:220-233.
- Cardinale JP, Sriramula S, Pariaut R, Guggilam A, Mariappan N, Elks CM, et al. HDAC inhibition attenuates inflammatory, hypertrophic, and hypertensive responses in spontaneously hypertensive rats. Hypertens. 2010;56:437-444.
- Belrose G, Gross A, Olindo S, Lezin A, Dueymes M, Komla-Soukha I, et al. Effects of valproate on Tax and HBZ expression in HTLV-1 and HAM/TSP T lymphocytes. Blood. 2011;118:2483-2491.
- Lemasson I, Lewis MR, Polakowski N, Hivin P, Cavanagh MH, Thebault S, et al. Human T-cell leukemia virus type 1 (HTLV-1) bZIP protein interactswith the cellular transcription factor CREB to inhibit HTLV-1 transcription. J virol. 2007;81:1543-1553.
- Afonso PV, Mekaouche M, Mortreux F, Toulza F, Moriceau A, Wattel E, et al. Highly active antiretroviral treatment against STLV-1 infection combining reverse transcriptase and HDAC inhibitors. Blood. 2010;116:3802-3808.
- Olindo S, Belrose G, Gillet N, Rodriguez S, Boxus M, Verlaeten O, etal. Safety of long-term treatment of HAM/TSP patients with valproic acid. Blood. 2011;118:6306-6309.
- Nakamura T, Shibayama K, Nagasato K, Matsuo H, Tsujihata M, Nagataki S. The efficacy of interferon-alpha treatment in human T-lymphotropic virus type-I-associatedmyelopathy. Jpn j med. 1990;29:362-367.
- Shibayama K, Nakamura T, Nagasato K, Shirabe S, Tsujihata M, Nagataki S. Interferon-alpha treatment in HTLV-I-associated myelopathy: studies of clinical and immunological aspects. J Neurol Sci. 1991;106:186-192.
- Feng J, Misu T, Fujihara K, Saito H, Takahashi T, Kohnosu T, et al. Interferon-α significantly reduces cerebrospinal fluid CD4 cell subsets in HAM/TSP. J Neuroimmunol. 2003;141:170-173.
- Feng J, Misu T, Fujihara K, Misawa N, Koyanagi Y, Shiga Y, et al. Th1/Th2 balance and HTLV-I proviral load in HAM/TSP patients treated with interferon-α. J Neuroimmunol. 2004;151:189-194.
- Saito M, Nakagawa M, Kaseda S, Matsuzaki T, Jonosono M, Eiraku N, et al. Decreased human T lymphotropic virus type I (HTLV-I) provirus load and alteration in T cell phenotype after interferon-α therapy for HTLV-I–associated myelopathy/tropical spastic paraparesis. J Infect Dis. 2004;189:29-40.
- Nakagawa M, Nakahara K, Maruyama Y, Kawabata M, Higuchi I, Kubota H, et al. Therapeutic trials in 200 patients with HTLV-Iassociated myelopathy/tropical spastic paraparesis. J neurovirol: 1996;2:345-355.
- Guarda G, Braun M, Staehli F, Tardivel A, Mattmann C, Förster I, et al. Type I interferon inhibits interleukin-1 production and inflammasome activation. Immun. 2011;34:213-223.
- Araujo AdQ-C, Afonso CR, Leite ACB, Dultra SV. Intravenous methylprednisolone in HTLV-I associated myelopathy/tropical spastic paraparesis (HAM/TSP). Arq Neuropsiquiatr. 1993;51:325.
- Karimooy HN, Derakhshan M, Rezaee SA, Hosseini M. Prednisolone as a new approach for treatment of HTLV-1 associated polyneuropathy. Pakistan Journal of Medical Sciences. 2009;25:142-145.
- Airla N, Luomala M, Elovaara I, Kettunen E, Knuutila S, Lehtimäki T. Suppression of immune system genes by methylprednisolone in exacerbations of multiple sclerosis. J Neurol. 2004;251:1215-1219.
- Meduri GU, Tolley EA, Chrousos GP, Stentz F. Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving acute respiratory distress syndrome: evidence for inadequate endogenous glucocorticoid secretion and inflammation-induced immune cell resistance to glucocorticoids. Am J Respir Crit Care Med. 2002;165:983-991.
- Scheinman RI, Cogswell PC, Lofquist AK, Baldwin AS. Role of transcriptional activation of IκBα in mediation of immunosuppression by glucocorticoids. Sci: 1995; 270: 283-6.
- Auphan N, Di Donato JA, Rosette C, Helmberg A, Karin M. Immunosuppression by glucocorticoids: inhibition of NF-κB activity through induction of IκB synthesis. Sci. 1995;270:286-290.
- Eggert M, Goertsches R, Seeck U, Dilk S, Neeck G, Zettl UK. Changes in the activation level of NF-kappa B in lymphocytes of MS patients during glucocorticoid pulse therapy. J Neurolog Sci. 2008;264:145-150.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.